As the gluten-free diet has gained popularity in recent years, you may hear mixed messages about it.
One expert may say that gluten is toxic to humans (and all living things), and many alternative health experts recommend a gluten-free diet as a “cure-all” for various diseases. On the other hand, conventional medicine experts will say that a gluten-free diet is unnecessary and even harmful, unless you have celiac disease.
So what is a person to do, if they have an autoimmune thyroid condition like Hashimoto’s thyroiditis?
My readers often ask me: What about eating gluten free for people who have Hashimoto’s, but do not have celiac disease?
In the following article, you’ll discover:
- The connection between gluten, celiac disease, and thyroid disease
- What to do if you’re already on a gluten-free diet and not in remission
- If there is harm to eating a gluten-free diet
- What to do if you’ve been “glutened”
- If you need to stay on a gluten-free diet forever
My Personal Experience Going Gluten Free
When I was first diagnosed with Hashimoto’s, I was working as a consultant pharmacist helping people with complicated healthcare needs in getting better health outcomes.
As a pharmacist, I knew that autoimmune conditions tend to co-occur and that having Hashimoto’s would put me at a greater risk for other types of autoimmune conditions, including celiac disease. In fact, I came across a study that suggested gluten could be a trigger for both celiac disease and Hashimoto’s.
Celiac disease is known for creating gastrointestinal distress… I had numerous gut-related symptoms including bloating, irritable bowel syndrome, acid reflux, and frequent stomach pains.
This was in addition to the “typical” hypothyroid symptoms of brain fog, fatigue, hair loss, weight gain, and cold intolerance!
I also had “non-typical” symptoms like anxiety, palpitations, joint pain, carpal tunnel, allergies, and panic attacks that are sometimes associated with celiac disease, so I had my doctor test me for celiac disease.
While I wasn’t exactly excited about having a second autoimmune condition, I was hopeful that gluten sensitivity and celiac disease would be my root cause, and that getting the right diagnosis would help me feel human again. But the celiac test came out negative, and my doctor told me I didn’t need to bother with the gluten-free diet.
As a result, I didn’t attempt the gluten-free diet. Instead, I started thyroid medications, but continued to deepen my research into my triggers as many of my symptoms continued, despite taking thyroid medications.
The medications helped me feel less tired (my sleep went from over 12 hours to 11 hours per night), and I was also less cold (I no longer needed two blankets at night!), but the other symptoms remained.
Digging Deeper
About a year into my journey, I decided to dig deeper. I still had an interest in exploring whether diet could play a role in my condition. I learned about three distinct reactions a person could have to foods.
- The celiac reaction – This is a reaction specifically to gluten, the protein found in wheat, barley, and rye, that is mediated by the IgA branch of the immune system and results in damage to the intestines.
- The allergic reaction – This is governed by the IgE branch of the immune system and results in immediate reactions like anaphylaxis, difficulty breathing, rashes, and hives (think hallmark reactions to peanuts or shellfish).
- The Type IV delayed hypersensitivity reaction – This is governed by the IgG branch of the immune system. Interestingly, Hashimoto’s is also a Type IV delayed hypersensitivity reaction.
Most research has focused on celiac disease and IgE reaction testing, while IgG testing is still considered experimental.
I had already been tested for celiac disease as well as IgE food reactions, but both of those tests came up negative, so I decided to try IgG food sensitivity testing.
The tests revealed that I had IgG reactions to gluten, as well as to the dairy proteins whey and casein.
At that point, my condition was only getting worse, despite taking higher and higher doses of thyroid meds.
With nothing to lose, I decided to give the gluten- and dairy-free diet a try.
To my complete disbelief and amazement, the bloating and stomach pains (a lifelong phenomenon), the irritable bowel syndrome (with me for almost 10 years at that point), and acid reflux (an unwanted guest for more than three years) vanished within three days!
I had previously been symptomatic despite taking proton pump inhibitors, Pepcid, Tums, and Pepto Bismol, and yet after three days of this diet, ALL of my symptoms were gone! I made a brave decision to try and stop my acid-suppressing medications, and guess what! The symptoms never came back.
That is, until a couple of months later when I got hungry at work and decided to try eating something at Panera. I didn’t realize the meal I had contained gluten and dairy… until I found myself with acid reflux and doubled over in the bathroom with stomach pain (just like I used to have) within hours of my meal. That convinced me to stay away from gluten and dairy for the long term.
As time went on, I saw more improvements in my health: the carpal tunnel went away, my panic attacks and anxiety resolved, and my thyroid antibody numbers (a potential marker of how aggressive the attack on the immune system is) were reduced.
I know skeptics will say, “Great, but you’re only one person — what about everyone else? What about me?”
While the research for IgE food reactions in Hashimoto’s is lacking, I want you to be aware of the important role of the other two types of reactions: celiac disease (IgA) and the Type IV delayed hypersensitivity (IgG) reaction.
Thankfully, there is now a lot of research about celiac disease and how it relates to Hashimoto’s and thyroid function.
I’ve also done some of my own research with over 2000 people with Hashimoto’s (with and without celiac disease), and have used IgG testing extensively, which I believe will support the role of Type IV delayed hypersensitivity (IgG) reactions with Hashimoto’s.
In this article, I’ll touch on the controversial concept known as “non-celiac gluten sensitivity” (NCGS), which I personally believe could be an umbrella term that may one day include the Type IV delayed hypersensitivity (IgG) reaction I’ve documented.
What Is Gluten?
It’s important to understand what gluten is to then understand how it can create a toxic response in people with autoimmune disease, including those with Hashimoto’s.
Gluten is found in grains like barley, rye, and wheat. It’s a staple in the Western diet that you’ll encounter in most breads, cereals, and pasta.
Gluten is made up of many different types of proteins, but the two main ones are “gliadins” and “glutenins.” Gliadin makes up the majority of gluten’s structure, and is usually responsible for the reactions observed in those with celiac disease (gliadin antibodies are used to diagnose celiac disease).
Within the two proteins that make the structure, different peptides (smaller chains of protein) can affect one’s reaction to gluten. Modern wheat contains two specific forms, Glia-α9 and Glia-α20, which are also the forms that contribute to gluten reactions. These peptides are recognized by the body’s gluten-sensitive T cells (cells that are part of the immune system) — these cells then label gluten as a foreign invader, contributing to part of the immune-mediated gluten reaction.
What Is Celiac Disease?
An estimated one percent of people (about three million worldwide) have celiac disease, which is an autoimmune disease that results in an autoimmune attack on the gut every time gluten is consumed. Those with celiac disease must stay absolutely 100 percent gluten free in both their diet and their lifestyle, or else they will have significant life-affecting symptoms.
For those who develop celiac disease, exposure to gluten triggers the release of zonulin, a chemical that signals the tight junctions of the intestinal wall to open up. This creates intestinal permeability (also known as leaky gut), where toxins, partially-digested food particles, and microbes are allowed to pass into the bloodstream. The body’s immune system is then triggered to attack these invaders.
Every time someone with celiac disease consumes gluten, their immune system is engaged again, resulting in a variety of symptoms.
Research has shown that gluten triggers this issue in everyone, even those who don’t have celiac disease! But those with celiac disease will also experience an autoimmune attack on the intestines with every bite of gluten. As mentioned above, this reaction is mediated by the IgA branch of the immune system and results in intestinal damage.
This attack destroys the villi, which are delicate, hair-like projections that cover the intestines.
The villi are important as they help the body digest and absorb nutrients from food.
This destruction of the villi can result in malabsorption of nutrients such as selenium, a well-known risk factor for Hashimoto’s; as well as lead to issues relating to nutrient deficiencies such as fatigue, failure to thrive, anemia, osteoporosis, digestive issues, and other autoimmune diseases.
Celiac disease is often referred to as “the great imitator,” as many of the symptoms of the disease mimic those of other diseases. It can go undiagnosed for a long time, as it may be misdiagnosed as something else. Symptoms vary widely, with some people experiencing the classic severe diarrhea, nausea, weight loss, vomiting, and acid reflux, while others may not experience any gut issues at all.
Left undetected, people with celiac disease are at greater risk of developing intestinal cancer.
What Is Non-Celiac Gluten Sensitivity (NCGS)?
It’s important to note that gluten sensitivity can also be found in people who do not have celiac disease.
After finding out that I had IgG reactions to gluten, as well as to the dairy proteins whey and casein, I came across a condition known as non-celiac gluten sensitivity (NCGS). A 2017 paper published in the World Journal of Gastroenterology suggests that about six percent of people in the U.S. have NCGS, though I wouldn’t be surprised if this number was higher.
With non-celiac gluten sensitivity, people have celiac-like reactions to gluten, yet they don’t test positive for the typical IgA celiac antibodies, nor do they present with the characteristic damage to intestinal cells seen in celiac disease.
However, research has shown that there are many correlations between those with thyroid disease and gluten sensitivities. For example, a 2002 study in the European Journal of Endocrinology found that 43 percent of people with Hashimoto’s showed activated mucosal T cell immunity, which is usually correlated with gluten sensitivity.
While there is research to support this condition, the condition is considered controversial by conventional medical circles and conventional media. It seems that every other month, I see a headline in the news that supports the condition, followed by another headline that states that the condition does not exist!
The challenge, in my opinion, is that there is no single diagnostic test or cause for non-celiac gluten sensitivity.
There could be numerous reasons why a person may react to wheat or gluten products. It’s worth noting that wheat-based foods contain FODMAPS (fermentable oligosaccharides, disaccharides, monosaccharides and polyols), a collection of short-chain carbohydrates that aren’t absorbed properly in the intestines of those with IBS and certain intestinal disorders like small intestinal bacterial overgrowth (SIBO). In a recent study, researchers have concluded that fructan, a type of oligosaccharide that is found in wheat, is to blame for NCGS symptoms, and not gluten. (I personally believe this could be the case for some, but not all people with NCGS.)
Histamine intolerance (which many people with Hashimoto’s may have) has also been tied to NCGS, as have other reactions to other particles, including nickel sensitivity.
A recent review article of the available scientific literature proposed that gluten sensitivity may occur as a result of a specific type of gut imbalance (known as dysbiosis).
Leccioli and colleagues proposed that the root cause of gluten sensitivity may be due to a decrease in the gut bacteria Firmicutes and/or Bifidobacteria, which produce the anti-inflammatory, gut-healing, short-chain fatty acid butyrate. This is a really interesting theory, as I’ve seen low butyrate levels in many of my Hashimoto’s clients who have taken the GI-MAP gut test.
I personally believe that NCGS is still an emerging concept that should be considered an umbrella term for the various reasons why a person may react to gluten-containing foods. I also believe that until science has a definitive answer, we should disregard the disempowering, gas-lighting headlines that say gluten sensitivity is all in our heads, and listen to our own bodies when a certain type of food does not agree with us!
I will tell you that my personal and clinical experience has shown that gluten sensitivity is one of the most significant triggers in Hashimoto’s. I base this opinion on the severity of symptoms that thousands of people with Hashimoto’s have reported, as well as the health improvements they experience once they remove gluten from their diets.
Why Are Gluten Allergies and Sensitivities So Common Today?
The first “official” (documented and reported) case of NCGS was only in 1980, and it is well known that the incidence of celiac disease has also been steadily rising, possibly even at an average rate of 7.5 percent per year since the 1950s, according to the Celiac Disease Foundation.
Both of these conditions are “new” and on the rise, but why is this so?
Gluten-containing foods have changed over the years, partly due to agricultural practices. And starting with the industrial revolution, the consumption of grain-based foods was encouraged as a cheap option to consume enough calories (whereas society had previously put much less emphasis on these gluten-containing foods).
In addition to these components, gluten-containing foods such as bread were once prepared differently, using a “sourdough” fermentation process. This process breaks down the gluten protein (as the technique requires putting a special type of yeast in the flour).
Small studies show breads prepared from wheat in a traditional sourdough process, appear safe for people with celiac disease. Another study showed the types of beneficial bacteria produced in the fermentation of breads might actually promote healing for those with celiac disease. I have not personally tried sourdough breads after going gluten-free, as my life improved significantly after removing gluten from my diet, and I don’t have a desire to make myself sick again.
The increased hybridization and processing of wheat in today’s world (as opposed to using traditional fermentation techniques), specifically with industrial agriculture, could be behind the fairly recent rise in gluten sensitivity and intolerance. (Gluten proteins in modern cereals are more prevalent than in ancient varieties.)
This increased production and consumption of gluten-containing foods are likely part of the reason gluten allergies and sensitivities are on the rise.
Why are we eating more gluten than ever before? It’s hiding in other food products. For example, you’ll often see wheat flour added to many sauces and even chocolates! Foods may also be cross-contaminated with gluten during processing — oats are a common example.
(Did you know? Hidden gluten is everywhere, and can even be found in personal care products!)
It is also possible that chemicals such as pesticides could have something to do with a rise in gluten sensitivity and intolerance. One small pilot study published in Environmental Research found that younger adults who had high levels of chemicals in their blood were more likely to develop gluten sensitivity or be diagnosed with celiac disease, than those with lower levels of certain chemicals in their blood.
Other researchers have theorized connections between synthetic pesticides and celiac disease — particularly that glyphosate has contributed to the rise in celiac disease. This is an interesting possibility, but research remains inconclusive.
(Even though we don’t know that pesticides in wheat contribute to gluten-related disorders, it is exactly because of this type of unknown that I encourage you to eat organic whenever possible!)
Research points to another possibility to do with the prevalence of “baker’s asthma” (a wheat allergy that develops over time from inhaling wheat flour), and wheat sensitivity/allergy. A group of non-gluten proteins called alpha-amylase/trypsin inhibitors (ATIs) essentially act as “natural” pesticides in wheat, and are known to trigger baker’s asthma, as well as contribute to general inflammation and gut inflammation.
The most severe forms of wheat allergies (this level of allergy is rare, but can include anaphylaxis) are definitely triggered by gluten, not ATIs. That said, ATIs are behind baker’s asthma, and glycosylated ATIs appear to be particularly bad.
Per a 2021 comprehensive review of the research (published in Frontiers in Nutrition), we do know that the ATIs in wheat flour contribute to bakers’ occupational health issues (asthma, eczema) and some allergies, and are also involved in gut disorders. ATIs may negatively affect gliadin digestion and contribute to celiac disease.
But researchers still question some of the mechanisms behind how this happens, or what specifically triggers certain allergies and sensitivities — in other words, both gluten and ATIs are potential culprits, broadly speaking.
So, multiple components in wheat (wheat-containing foods) could contribute to NCGS and/or celiac disease.
Is It Just American Gluten That’s Problematic?
I often hear people in the U.S. claim that they only have issues with “American gluten,” and do not have problems when they travel to Europe and elsewhere — they can eat bread overseas. This leads some individuals to believe that only “American gluten” is an issue.
Yet having lived in Europe myself, and having worked with clients from Europe, Asia, Australia, South America and Africa of diverse nationalities, I can tell you something.
- People living in Spain with Hashimoto’s feel better gluten free
- People living in Italy with Hashimoto’s feel better gluten free
- People living in Poland with Hashimoto’s feel better gluten free (My colleague Dominika Gier recently co-published a study about this in 2021.)
- People living in mainland China with Hashimoto’s feel better gluten free
- People living in Germany with Hashimoto’s feel better gluten free
- People living in the UK with Hashimoto’s feel better gluten free
- People living in Greece with Hashimoto’s feel better gluten free
- People living in Australia with Hashimoto’s feel better gluten free
Just as we locals react to the wheat here in the U.S., people in Europe and elsewhere can be sensitive and react to their own local wheat. (I learned this first-hand while living in Europe in 2014 and consulting numerous European clients over the years.)
Furthermore, the prevalence of celiac disease in a large sample of the European population (Finland, Germany, Italy, and the U.K.) was found to be about one percent, similar to the rates in the U.S.
Having consulted with clients from all over the world, I can attest that most Hashimoto’s clients feel better off wheat, no matter where they live! As such, being somewhere on the gluten intolerance spectrum is not just an American phenomenon.
The reason why a person who goes abroad may not react to gluten-based foods in that region is because the proteins in foods are slightly different depending on where they are grown. Thus, the body may not immediately recognize the foreign proteins as something it should react to. In my experience, people may be non-reactive for up to two weeks to the local wheat, but longer-term eating of wheat abroad will produce symptoms eventually, as the proteins are similar enough for the immune system to link them up and produce the same reaction. I call this the “gluten honeymoon phenomenon.”
The Celiac and Thyroid Connection
Gluten sensitivity is often linked to the thyroid.
Celiac disease can co-occur with Hashimoto’s. In fact, studies have estimated that between 1.2 and 15 percent of Hashimoto’s patients also have celiac disease!
Furthermore, the antibodies produced in celiac disease can cross-react with thyroid antibodies because they may share similar molecular structures, so molecular mimicry may be one of the reasons for the common co-occurrence of both conditions.
When I first began to research lifestyle interventions that could improve my condition, I came across an Italian study focused on people who had subclinical hypothyroidism, Hashimoto’s, and celiac disease, but who had not been following a gluten-free diet.
As the gluten-free diet is indicated for people with celiac disease, the diet was helpful for the study participants’ intestinal symptoms and helped them recover the health of their intestines.
There were also improvements in thyroid function! The study found that when most of those with subclinical hypothyroidism were placed on a gluten-free diet, their thyroid function normalized! About 71 percent of people who had subclinical hypothyroidism (a mildly underactive thyroid) and who had strictly followed a one-year gluten withdrawal (as confirmed by intestinal mucosa recovery), saw a return in normal thyroid function.
Additionally, 19 percent of people who followed the gluten-free diet were able to normalize their thyroid antibodies, no longer testing positive for Hashimoto’s. The researchers of the study concluded: “In distinct cases, gluten withdrawal may single-handedly reverse the abnormality.”
In another study involving patients with Hashimoto’s and celiac disease, the average dose of levothyroxine needed (prior to the study) to treat patients with Hashimoto’s alone, was lower than the average dose required to treat patients with both conditions (that is, Hashimoto’s and celiac disease). Furthermore, the study showed that when the Hashimoto’s and celiac disease patients went on a gluten-free diet, their TSH levels decreased, along with the amount of T4 thyroid medication needed to achieve a targeted lower TSH level!
The study concluded that their TSH likely decreased because of better absorption of thyroid medications. This makes sense as untreated celiac disease can significantly impair medication absorption. However, I’ve also seen some patients with celiac disease and hypothyroidism wean off thyroid meds completely after being off gluten for 3-12 months, so I suspect that some of the patients in the study also had a recovery of thyroid function that was missed by the researchers because the patients were not followed for a long enough period of time.
In yet another study involving 104 Hashimoto’s patients, researchers found that 50 percent of patients with Hashimoto’s also had celiac-specific genes, putting them at risk for celiac disease. (However, it’s important to remember that though these people had the right genes, genes are not always our destiny — an environmental trigger is often required for the expression of celiac genes and for the condition to manifest.)
Additional Effects of Gluten
I often see articles and comments online ridiculing people without celiac disease for going gluten free to improve their health. I find this to be a very closed-minded point of view, and quite frankly, a dangerous one as well.
A growing body of research suggests that gluten-related disorders can affect an individual’s psychological state and decrease an individual’s quality of life and overall well-being.
Celiac disease has been associated with psychological disorders and mood imbalances. One study found individuals with celiac disease experienced a significant improvement in quality of life, anxiety, and depression one year after implementing a gluten-free diet.
A 2018 review also demonstrated that gluten can contribute to mood disorders for individuals with NCGS. The authors of this study found individuals experienced improvements in mood on a gluten-free diet.
Gluten and Intestinal Permeability
Another important point to make about gluten and autoimmune disease is that studies have shown that gluten can induce intestinal permeability in all individuals, regardless of whether or not they have celiac disease.
Why is that important?
It’s because Dr. Alessio Fasano, MD, an expert on gluten-related disorders, and other researchers, have found that every case of autoimmune disease needs three things present to occur:
- A genetic predisposition
- An environmental trigger
- Intestinal permeability
If one of the three things is missing, the condition will go into remission. (Please read my article on gut health for more information on this.)
While we can’t change our genes (just yet), and while we don’t always have power over our triggers, we can always address the strength of our intestines and work on making them less permeable!
One obvious strategy to make intestines less permeable is to remove the substances that induce their permeability.
I find it is helpful to think of the intestinal permeability (commonly called leaky gut) reaction to gluten in terms of a spectrum.
On one side of the spectrum, some people may only experience momentary discomfort after eating gluten, such as brief bloating. On the other side of the spectrum, you will find people with celiac disease who suffer greatly, and even tiny amounts of gluten can cause significant damage to their intestines and symptoms for many weeks.
Testing for Celiac Disease
If you suspect you may be sensitive to gluten and are currently eating gluten, you may first wish to get tested for celiac disease.
The risk for celiac disease increases if you have a family history of the disease, European ancestry, and/or a personal history of other autoimmune disorders.
There are several options to diagnose celiac disease. However, current testing is far from perfect, with blood-screening tests often coming back negative. Additionally, a person must be eating gluten to test positive for celiac disease!
These are the current blood-screening tests available:
- The Tissue Transglutaminase Antibodies (tTG-IgA) test: This blood test is often used to diagnose celiac disease. If you are currently on a gluten-free diet, a gluten challenge (which requires you to have eaten two slices of wheat-based bread per day over the course of 6 to 8 weeks) is often recommended prior to taking this test, to allow any antibodies to appear in your bloodstream. Unfortunately, this test may result in false negatives and false positives.
- IgA Endomysial antibody (EMA) test: This test is not as sensitive as the tTG-IgA test. It’s usually used for patients that are difficult to diagnose, but about 5-10 percent of those with celiac disease do not have a positive EMA test.
- Total serum IgA test: This test checks for IgA deficiency, which is often associated with celiac disease. IgA deficiency can cause false negatives on tTG-IgA or EMA tests.
- Deamidated gliadin peptide (DGP IgA and IgG) test: This test can be used to further screen for celiac disease in those who test negative for both tTg and EMA antibodies, as well as in those with IgA deficiency.
Please note, it’s possible for people with celiac disease to have negative test results, especially if they’re already following a gluten-free diet.
The biopsy of the small intestine is considered the “gold standard” way to confirm a diagnosis and will find more cases of celiac disease than the blood tests. However, again, the person must be eating gluten in order for the biopsy results to be accurate.
A genetic test is a test for celiac disease that can be utilized without a gluten trial. Most people with celiac disease have the HLA-DQ2 and HLA-DQ8 genes, and about 30 percent of all people have these genes. Please note, the genes only predict susceptibility, not whether the celiac disease is expressed. One can do genetic testing through various companies such as 23andMe to help determine if you are genetically at risk for developing celiac disease.
If you’re already following a gluten-free diet and feeling better, I personally believe that your body’s own response to gluten is the best test to determine if you should be gluten-free, and I am apprehensive about “gluten challenges” just to get a diagnosis. Specifically, this test is not recommended for pregnant women who have been gluten-free, as they can precipitate a miscarriage. But even if you’re not pregnant, I believe in treating your body well and nourishing it!
I remember one of my readers with multiple autoimmune symptoms had started the gluten-free diet. Within weeks, the diet resolved her symptoms, but in order to qualify for specialized health benefits in her country, she had to undertake a trial of gluten and was nearly hospitalized with intestinal bleeding during this trial!
IgG Gluten Sensitivity as a Trigger in Hashimoto’s
If you do not test positive for celiac disease, you may still have NCGS.
The current studies of NCGS have not come up with conclusive opinions, or even diagnostic tests for gluten sensitivity on IgG reactions to gluten.
However, I believe that Type IV hypersensitivity (IgG) reactions are a critical piece of why gluten is a problem for many with Hashimoto’s. People with Hashimoto’s often present with numerous food sensitivities, and testing may show IgG antibodies to various food proteins. IgG antibodies are thought to be the same types of antibodies that target the thyroid gland in autoimmune disease.
Thus, removing IgG-reactive foods may attenuate the IgG response to the thyroid gland. These reactions can be tested via lab testing, as well as through an elimination diet (more on testing options further below).
The Benefits of Going Gluten Free
While the mainstream research and “evidence base” for eliminating food antigens like gluten in Hashimoto’s is still lagging, I’ve seen tremendous benefits in my own personal health as well as the health of many of my private clients using unconventional methods… So I decided to create my own evidence base!
I used my outcomes research training to create a little survey that went a bit viral… In the summer of 2015, I developed a survey to assess the impact of various interventions on Hashimoto’s. Some 2,232 people with Hashimoto’s provided feedback as to the factors that seemed to make their conditions better as well as worse. Many food and non-food triggers were assessed, but I would like to focus on gluten for this article.
First of all, it is worth noting that out of all who responded, only 3.5 percent had also been diagnosed with celiac disease. (This is consistent with the reported rate of celiac disease of 1-15 percent in people with Hashimoto’s.)
Yet, 86 percent of respondents who had gone gluten free reported improvements in digestive symptoms. I believe this re-confirms my earlier points — you do NOT have to have celiac disease to benefit from a gluten-free diet!
Most readers said their gluten reactions had included gut issues like constipation, diarrhea, cramping, bloating, gas, and burning or burping from acid reflux, as well as brain-related symptoms such as headaches, brain fog, anxiety, depression, fatigue, and insomnia. And most felt better going gluten free.
In fact, 88 percent of people with Hashimoto’s who chose to remove gluten from their diets felt better.
Thirty-three percent of respondents had a reduction in their thyroid antibodies on a gluten-free diet. (As mentioned above, thyroid antibodies are considered to be a potential marker of how aggressive the attack is against the thyroid gland, and a lower number generally indicates a less aggressive attack.)
Along with feeling better and seeing a reduction in antibodies, the biggest benefits seen in people with Hashimoto’s on the gluten-free diet were more energy (in 67 percent of people), a better mood (in 60 percent of people), and a healthier weight (in 52 percent of people). As a pharmacist, I was surprised to see that more people reported improvements with the gluten-free diet in these domains than they did with using thyroid replacement hormones!
The survey results mirrored the outcomes I had been tracking from my clients as well!
Based on my clinical experience and the results above, I firmly believe that the gluten-free diet can be a very effective intervention for most people with Hashimoto’s, even in the absence of celiac disease.
Can Eating a Gluten-Free Diet Be Harmful?
Often, people worry about missing out on essential nutrients by removing gluten-containing grains from their diet. Fortunately, in many cases, people actually absorb nutrients more effectively from their food when they remove gluten from their diet! In fact, I’ve seen multiple cases of iron/ferritin deficiency resolve on a gluten-free diet. That said, there are some documented deficiencies that are reported on a gluten-free diet, but the good news is that you can supplement accordingly.
One of the most common nutrients depleted in gluten-free diets is selenium, which also happens to be a common deficiency in Hashimoto’s! To counter this, I recommend taking a selenium supplement, such as Pure Encapsulations Selenium, or Rootcology’s Selenium + Myo-Inositol. (Check out my Selenium article for more information on the synergistic benefits of these two nutrients in those with Hashimoto’s.)
Grain-free diets can also result in a deficiency of thiamine (vitamin B1), another common nutrient deficiency. (Read my full thiamine article for more information.) I recommend supplementing with Benfomax by Pure Encapsulations to ensure you’re getting enough of this vitamin.
Other vitamin deficiencies that may occur on the gluten-free diet include vitamin A, B2, B3, B5, B6, B7, B9, B12, vitamin D, calcium, copper, iron, magnesium, phosphorus, and zinc. If you’re also following the Paleo diet, you may be deficient in vitamin B7 and chromium as well. Again, testing for nutrient deficiencies and boosting your nutrient levels with supplements will help you maintain optimal vitamin levels!
How to Feel Better
So what can you do today to feel better?
I hope I have convinced you (or at least tempted you to do some of your own detective work to learn more :-)) that gluten is a common trigger for those with Hashimoto’s.
Based on all of the research and the results from 2,232 of my readers, I firmly believe that every person with an autoimmune thyroid condition should try removing gluten from their diet.
Even for those who do not have celiac disease or a diagnosed gluten sensitivity, gluten causes intestinal permeability and can cause significant life-affecting symptoms. You owe it to yourself to at least try eliminating it from your diet… and let subsiding symptoms speak for themselves. You can always add it back if you do not feel any improvements.
Food Sensitivity Testing
Some people need to see that they react to a food “on paper” before they commit to making a change. I get it. I was one of them! If you are looking for that proof, I have found that IgG-based food sensitivity tests can be incredibly helpful in recognizing your food reactions and minimizing your symptoms!
Food sensitivities are very individualized, so you might be surprised to find some odd things you are sensitive to!
For me, I wasn’t just reactive to the usual suspects of gluten and dairy, but I had reactions to pineapples and peaches too! They both triggered my acid reflux. It is also worth noting that I tested borderline for gluten intolerance (although I was positive for dairy protein intolerance), but felt much better after removing both from my diet. A follow-up elimination challenge with both foods confirmed my sensitivity to both.
However, not all IgG tests are created equally — there are no defined standards in the IgG food testing industry, and some tests I’ve seen are highly inaccurate. They may show up with numerous false negatives (meaning you’ll still be eating foods that are causing inflammation in your body) and numerous false positives (meaning you’ll be left feeling overwhelmed and with nothing you can eat)!
The test that I have found to be highly accurate for myself and my clients is the Alletess Lab food sensitivity test. If a type of food comes up positive on that test, I know that it is a reactive food for that person.
Alletess Lab works primarily through integrative and functional medicine physicians, so if you’re working with such a doctor, you can ask him/her to order the test for you. I’ve also worked with a couple of lab providers to offer Alletess Lab food sensitivity tests for people to self-order without a doctor’s prescription. The test kit comes with a little blood spot collection paper, and can be mailed to just about anywhere in the world!
The results are also self-explanatory, so you don’t need a highly-skilled healthcare professional to interpret them for you. You either react to a food or you don’t!
Alletess offers two options to test for the most commonly eaten foods (including gluten):
The 96 food panel is a good one to uncover most food triggers. You’ll get a comprehensive report that identifies your sensitivities. I do recommend people repeat sensitivity testing on an annual basis for best results, as reactions to foods can change.
I’ve used this test for hundreds of people with Hashimoto’s, and most do come up with an IgG gluten reaction. I hope to have the results published after my team and I have crunched all of the numbers!
Why an Elimination Diet Is the Best Gluten Sensitivity Test
If you can’t afford food sensitivity testing, I have some good news for you. There is a test you can do that’s absolutely free, but it does require more work and paying attention. The elimination diet is still considered the gold standard for food sensitivity testing. Your body will always tell you which foods do not agree with it, but only if you listen to it very carefully.
Why are food sensitivities so difficult to pinpoint? One reason is because we keep eating the foods that our body is sensitive to. For me, I ate dairy and bread every day, never connecting those foods to my long list of symptoms. When you eat a particular food on a daily basis, it is difficult to connect that food to any symptoms you are having.
You might have joint pain, bloating, and acid reflux every day, but how would you ever connect that to the dairy you have always had?
As you continue to consume the food you are sensitive to, your body becomes depleted in its ability to protect itself from the antigenic food. The reactions become less specific and more chronic. Additionally, your body will become sensitive to more and more things.
That is why an elimination diet helps greatly. If you remove a particular sensitizing food for a few weeks, you should feel better and experience less bloating, reflux, and other digestion-related symptoms. And when you are exposed to that food again, your body will be able to produce a stronger, more specific reaction, which will allow you to recognize which particular food is problematic.
I always recommend an elimination diet where you avoid the food in question for 2-3 weeks. See how you feel, and then try it again to see if you react to it.
Check out my podcast with Tom Malterre for more info about elimination diets!
Tips for a Gluten-Free Diet
If you’re ready to move to a gluten-free diet now, I’ve got plenty of resources to help you get started.
- Take a peek at my articles, How to Eat for Thyroid Health on a Budget, Autoimmune Paleo Diet, A Paleo Diet: Will It Resolve Your Hashimoto’s?, and The Best Diet for Hashimoto’s.
- Having a plan and some good substitutions will help, so I developed a quick start guide with some delicious gluten-free recipes to help you ease into the transition. Download my Thyroid Diet Quick Start Guide with gluten-free recipes.
- Check out some of the thyroid-friendly recipes from my book, Hashimoto’s Food Pharmacology: Nutrition Protocols and Healing Recipes to Take Charge of Your Thyroid Health.
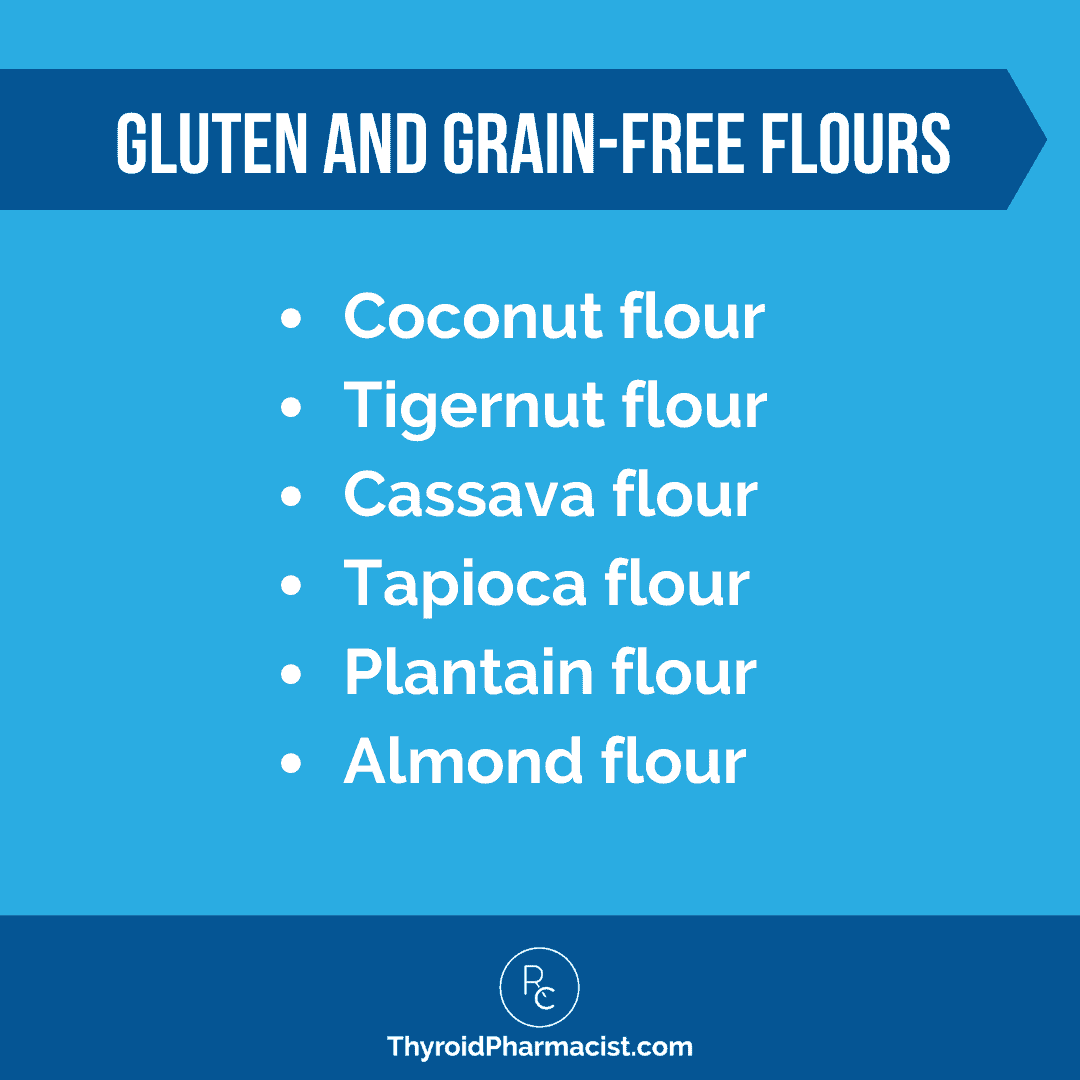
- Don’t give up on baking! There are plenty of gluten- and grain-free flours out there today, many of which can be found in conventional grocery stores.
- Keep simple, gluten-free ingredients and snacks prepped ahead of time so that you have something healthy to reach for when hunger strikes!
- Make smoothies part of your regular routine. My favorite green smoothie is packed with nutrition for your thyroid, helps to reduce inflammation, and can help with detoxification. I start my day with this recipe (which includes one of Rootcology’s protein powders) every morning, and it has transformed my day!
For more gluten-free snack and meal ideas, download my free recipe book!
Do You Need to Stay on a Gluten-Free Diet Forever?
I would say generally with Hashimoto’s, most people should remain on a gluten-free diet for the long term. That said, I have seen some people who have been able to reintroduce all foods back in and seemingly don’t have any adverse reactions to gluten.
Some readers have reported that they tolerate sourdough, einkorn and imported non-GMO wheat products, but I can’t verify this with their medical records. In other cases, some people I have consulted believe that they do not react to gluten, but in my opinion, have symptoms that make me suspicious of gluten sensitivity, like joint pain, anxiety, and Hashimoto’s flare-ups. As such, I wonder if they are truly not reactive.
If gluten sensitivity is indeed caused by an imbalance of butyrate-producing bacteria, in theory, replenishing the beneficial bacteria could deem gluten sensitivity reversible. Some individuals have reported no longer reacting to gluten after taking the Megaspore probiotic. (I also offer a spore-based probiotic by Rootcology.)
I’m still studying the phenomenon of reducing gluten reactions and improving digestion, and I’m hoping to get to the bottom of it for myself, and to share it with all of you. 🙂
(This will be the focus of one of my future books. I generally spend about three years on research and testing, and one year or so in writing, before I publish a book on a topic or give a definitive opinion!) But for now, I would say that long-term avoidance of gluten is going to be best for most people. (Be sure to subscribe to my newsletter to receive any future updates!)
What to Do if You’ve Been “Glutened” or May Be Accidentally Exposed to Gluten
Though I do recommend avoiding gluten, there are times that we may eat it by accident — here’s what you can do if you find yourself in this situation.
Prevention
How many times have you been to a restaurant that was supposed to be safe to eat at, only to discover you’ve been glutened?
Depending on the person, the effects can last from a few hours to a few weeks. One supplement that I’ve found to be helpful in uncertain situations is Gluten/Dairy Digest. Gluten/Dairy Digest contains enzymes that assist in breaking down gluten and dairy proteins and can help to lessen reactions to them.
These enzymes can be very helpful for those of us with gluten and dairy sensitivity in times where we’re concerned about cross-contamination or when we’ve accidentally consumed something we shouldn’t have.
Other digestive enzymes may also offer some protection by helping to break down difficult proteins like gluten. Betaine HCl and pepsin are naturally occurring components of the gastric juices that support our digestion by breaking down protein bonds in our food so their nutrients are easier for our intestines to absorb. They can also help us break down gluten particles. You can learn more about the benefits of betaine with pepsin, and how to find out the appropriate dosage for you, here.
Unfortunately, enzymes only work when you take them with the offending food. Furthermore, while they can minimize the reactions to gluten and dairy, they are not likely to completely eliminate them. So, I don’t recommend trying to eat a pound of cheese or a loaf of bread just because you’re taking this type of supplement.
After the Exposure
- Magnesium citrate – Magnesium is something that I recommend taking daily for most people with Hashimoto’s, as getting adequate magnesium from a standard diet can be difficult, and symptoms are often confused with those of other conditions. Taking additional magnesium in cases of accidental exposure to foods that you’re sensitive to will ensure that your bowels are moving properly and will support a healthy detoxification process.
- Physicians Elemental Diet – After you’ve been exposed to foods that you are sensitive to, one very important step in recovery is giving your digestive system time to rest. The best way to do this is through a period where you do not consume any solid foods, which will allow the inflammation to die down. The tricky part is, if you’re not consuming enough food, you can wind up feeling tired and drained. One way to prevent this from happening is to use a special formula, like the Physician’s Elemental Diet, designed to provide the body with the nutrients it needs while allowing your intestines to repair. Please note, Integrative Therapeutics has removed the distribution of this formula from retail channels, as it is an FDA-regulated medical food. As always, I do recommend working with your personal health care provider to ensure this (or any other) intervention is appropriate for you. However, if you and your practitioner are having trouble obtaining this elemental formula, Dr. Siebecker’s homemade Elemental Diet may be a suitable alternative.
- Lemon Water – Drinking this first thing in the morning and throughout the day will help increase and support your stomach acid, as well as your liver detox pathways. It will also assist in the removal of toxins to help your body recover faster from accidental gluten exposure.
- Bone broth – While gluten and dairy exposure can lead to a leaky gut by perforating the walls of the intestines, bone broth can help soothe the gut and heal the damage. The gelatin in bone broth helps to seal the junctions in the intestines so they are no longer permeable. That way, gluten and dairy particles, as well as other food particles and toxins you may be sensitive to, can no longer pass through the intestinal wall. (In addition to boosting gut health, bone broth has many other benefits: boosting immunity, relieving joint pain, increasing energy, improving digestion, and giving you a more youthful appearance. You can find how to make my own version of bone broth here!)
- Epsom Salt Bath – Taking a hot Epsom salt bath every day is not only a wonderful way to relax and de-stress, it’s also a great source of magnesium. The magnesium will stimulate the bowels and help your body eliminate toxins. All you need is one cup of Epsom salts in a bath of hot water.
- Activated charcoal – Activated charcoal is an amazing supplement that binds up toxins and can minimize food reactions. I recommend taking one to three capsules at bedtime, at least four hours away from other medications or supplements (to avoid impairing their absorption), to help detoxify from food reactions. Additionally, I recommend supplementing with magnesium when taking activated charcoal because it can cause constipation, and it’s important to keep the stools and toxins moving out of the body.

What You Can Expect With a Gluten-Free Diet
Although the idea of removing gluten from your diet may seem daunting, in the bigger picture you’ll likely find that going gluten free offers you much more freedom.
Up to 20 percent of people with celiac disease and Hashimoto’s can be free of Hashimoto’s within a year of going gluten free, and some may go into remission in as little as three months.
Moreover, up to 90 percent can be free of numerous, often lifelong symptoms!
Here are just a few comments from my readers and clients:
- “[A] gluten-free diet has helped me reduce antibodies almost to a normal range.”
- “Going gluten free helped me tremendously. It took eight months to feel the difference, and now after two years, most of my symptoms are gone. Nothing to lose by going gluten free.”
- “Since I went gluten free, my hair started growing back, my bloating and diarrhea [are] gone, [and I have] no more reflux either.”
- “Going gluten free has helped my hair to start growing back after losing all my hair — even my eyebrows and eyelashes.”
- “Gluten free and soy free for three months and I was able to lower my meds, and [my] stomach pain, alternating diarrhea and constipation, anxiety, and body aches [are] all gone!!”
- “I’m gluten free and have brought my antibodies down to normal range. So thankful!
Moving Forward… Gluten Free!
I know giving up gluten may sound daunting! It may take some work and some sacrifices to start cutting out gluten, but you are worth it.
You only have your symptoms to lose and you can go back to your previous diet if the gluten-free diet doesn’t help! I recommend giving it at least a month, though many people see the results in just a week. (I saw life-changing results in three days!)
Going gluten free is really one of the best things you can try when you have a thyroid condition like Hashimoto’s, hypothyroidism, or Graves’ disease.
Next Steps
If gluten is the sole root cause of your condition, you will likely see a complete remission of thyroid antibodies after you eliminate it from your diet, and your thyroid function may even return to normal within three to 12 months. If you don’t see such improvements, you will need to put your detective hat back on and dig deeper for other contributing root causes.
Getting off reactive foods almost always helps in the healing process.
Aside from gluten, other substantial food triggers include dairy (a large sensitivity for me!), eggs, sugar, soy, grains (corn, in particular), nightshades (tomatoes, potatoes, eggplants, and peppers), alcohol, caffeine, nuts, and seeds.
In my survey of 2,232 people with Hashimoto’s, 87 percent of respondents felt better on a sugar-free diet, 81 percent felt better on a grain-free or Paleo diet, 79 percent felt better on a dairy-free diet, 75 percent felt better on the Autoimmune Paleo diet, and 76 percent felt better on the Low Glycemic Index diet. (I discuss much more about these common food sensitivities and dietary interventions, as well as the healing foods you can eat to help you feel better, in my book, Hashimoto’s Protocol.)
Once you find your food triggers, you will still need to help your digestive system heal by adding supportive foods and nutrients.
I recommend a diet that keeps your blood sugar balanced, is rich in grass-fed meats, and features plenty of organic, nutrient-dense vegetables.
Survey respondents reported that homemade bone broth helped 70 percent of those that tried it, green smoothies helped 69 percent, and fermented foods helped 57 percent. Other foods that I have found to be particularly healing for a leaky gut include turmeric, fibrous vegetables, fermented foods, cilantro, and berries.
In that survey, there were nine great areas of learning beyond the issue of gluten intolerance, including supplements that had proven to be beneficial, the positive results of people using the medication Naltrexone in low doses, and the impact of stress as a trigger. It is also worth noting that many dietary interventions received higher percentages of “feeling better” results than actual prescribed thyroid medications. While 43 percent of people reported feeling better on Synthroid, and 58.9 percent felt better on Armour,* 88 percent felt better on the gluten-free diet.
As a pharmacist and someone who advocates for the proper use of thyroid medication, I am obviously a supporter of physician-prescribed thyroid medications to help manage patient symptoms and their condition. But as a “detective” who works diligently to solve my own — and my clients’ — health puzzles, I also want to point out the tremendous benefits you can see by trying some of these food elimination strategies.
*Note: While Armour Thyroid does not have any gluten-containing ingredients, it is not tested for gluten content, and cannot be certified as gluten-free. Armour does contain sodium starch glycolate, which can be derived from wheat or corn.
You may also need to focus on removing toxicity in your environment and supporting your body’s detoxification pathways. All of this is part of my two-week Liver Support Protocol.
You can learn the step-by-step instructions for this highly successful reparative protocol in my book, Hashimoto’s Protocol. The book also covers many other important protocols such as gut balancing, adrenal recovery, addressing infections, stress management, and more.
I hope this helps you on your healing journey!
P.S. You can download a Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free, by signing up for my weekly newsletter! You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow me on Facebook, Instagram, Pinterest, and TikTok too!
References
- Sategna-Guidetti C, Volta U, Ciacci C et al. Prevalence of thyroid disorders in untreated adult celiac disease patients and effect of gluten withdrawal: an Italian multicenter study. The American Journal of Gastroenterology. 2001;96(3):751-757. doi:10.1111/j.1572-0241.2001.03617.x.
- Lerner A, Jeremias P, Matthias T. Gut-thyroid axis and celiac disease. Endocrine Connections. 2017;6(4):R52-R58. doi:10.1530/EC-17-0021.
- Vojdani A, Tarash I. Cross-Reaction between Gliadin and Different Food and Tissue Antigens. Food and Nutrition Sciences. 2013;4(1):20-32. doi:10.4236/fns.2013.41005.
- Virili C et al. Atypical celiac disease as cause of increased need for thyroxine: a systematic study. The Journal of Clinical Endocrinology and Metabolism. 2012;97(3):E419-E422. doi:10.1210/jc.2011-1851.
- Celiac Disease Foundation. Screening. Celiac Disease Foundation. https://celiac.org/celiac-disease/understanding-celiac-disease-2/diagnosing-celiac-disease/screening/#O8ai1iT6IsODzqfu.99. Accessed December 28, 2017.
- Valentino R, Savastano S, Maglio M et al. Markers of potential coeliac disease in patients with Hashimoto’s thyroiditis. European Journal of Endocrinology. 2002;146(4):479-483. doi:10.1530/eje.0.1460479.
- Skodje G, Sarna V, Minelle I, et al. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-reported Non-celiac Gluten Sensitivity. Gastroenterology. 2017;S0016-5085(17):36302-36303. doi:10.1053/j.gastro.2017.10.040.
- Schnedi W, Lackner S, Enko D, Schenk M, Mangge H, Holasek S. Non-celiac gluten sensitivity: people without celiac disease avoiding gluten-is it due to histamine intolerance? Inflammation Research. 2017. doi:10.1007/s00011-017-1117-4.
- Leccioli V, Oliveri M, Romeo M, Berretta M, Rossi P. A New Proposal for the Pathogenic Mechanism of Non-Coeliac/Non-Allergic Gluten/Wheat Sensitivity: Piecing Together the Puzzle of Recent Scientific Evidence. Nutrients. 2017;9(11):1203. doi:10.3390/nu9111203.
- Hollon J, Puppa EL, Greenwald B, et al. Effect of Gliadin on Permeability of Intestinal Biopsy Explants from Celiac Disease Patients and Patients with Non-Celiac Gluten Sensitivity. Nutrients. 2015;7(3):1565–1576. doi:10.3390/nu7031565.
- Mustalahti K, Catassi C, Reunanen A, et al. The prevalence of celiac disease in Europe: results of a centralized, international mass screening project. Ann Med. 2010;42(8):587-95. doi: 10.3109/07853890.2010.505931.
- Abigail G, Leonardo T, Kurunthachalam K, et al. Persistent organic pollutant exposure and celiac disease: A pilot study. Env. Res. 2020;109439. DOI: 10.1016/j.envres.2020.109439
- Busby E, Bold J, Fellows L, Rostami K. Mood Disorders and Gluten: It’s Not All in Your Mind! A Systematic Review with Meta-Analysis. Nutrients. 2018;10(11):1708. Published 2018 Nov 8. doi:10.3390/nu10111708
- Igbinedion SO, Ansari J, Vasikaran A, et al. Non-celiac gluten sensitivity: All wheat attack is not celiac. World J Gastroenterol. 2017;23(40):7201-7210. doi:10.3748/wjg.v23.i40.7201
- de Lorgeril M, Salen P. Gluten and wheat intolerance today: are modern wheat strains involved?. Int J Food Sci Nutr. 2014;65(5):577-581. doi:10.3109/09637486.2014.886185
- Geisslitz S, Shewry P, Brouns F, et al. Wheat ATIs: Characteristics and Role in Human Disease. Front Nutr. 2021;8:667370. Published 2021 May 28. doi:10.3389/fnut.2021.667370
- Canova C, Rosato I, Marsilio I, et al. Quality of Life and Psychological Disorders in Coeliac Disease: A Prospective Multicentre Study. Nutrients. 2021;13(9):3233. Published 2021 Sep 16. doi:10.3390/nu13093233
- Ostrowska L, Gier D, Zyśk B. The Influence of Reducing Diets on Changes in Thyroid Parameters in Women Suffering from Obesity and Hashimoto’s Disease. Nutrients. 2021;13(3):862. Published 2021 Mar 5. doi:10.3390/nu13030862
Note: Originally published in January 2018, this article has been revised and updated for accuracy and thoroughness.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Źle reaguje na nikiel, czy powinnam wykluczyć z diety produkty które go zawierają? Czy to może być wyzwalaczem mojego Hashimoto? Pozdrawiam.
Kasia – thank you for following this page. I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
Hi Isabella,
Many thanks for everything you do!
One question around gluten-free that is rarely addressed, is about whether it’s ok to eat organic, local, ancient, non GMO, non-industrial, varieties of wheat.
Also another not-addressed subject, is people (like me) who have Hashimoto’s hypothyroid but do not have a weight problem, on the contrary, need to put on weight.
I would be very grateful if you could address these issues…
Many thanks !!!
Chandan Fraser
Chandan – thank you for following this page and my research. Most people with Hashimoto’s will experience weight gain, and so of course that’s what gets the most focus, but some people actually experience weight loss, or they can’t keep their weight on. This is especially problematic when a person has multiple food sensitivities and needs to adhere to an autoimmune diet that restricts foods. Here are a few tips to keep in mind:
1. Get a calorie counting app like My Fitness Pal on your phone, to help you keep track of your daily calories. Eating real food can be more filling than eating simple carbohydrates and you may not be getting enough calories. Use the app to figure out your target weight and the number of calories per day you need to get there.
2. Supplement after dinner with The Root Cause Building Smoothie: 1 avocado (300 calories), 1 cup coconut milk (150 calories), 1 banana (100 calories), 2 egg yolks (100 calories, if tolerated), 1 scoop of protein of beef/pea protein (60 calories) – You can also add cooked sweet potatoes if you need more carbs.
3. Get tested for gut infections. Gut infections can prevent the digestion and assimilation of foods, leaving you underweight and malnourished. The 401H test or GI Effects test are my go to tests.
4. Get your adrenals tested with an adrenal saliva tests. In some, stressed adrenals may actually lead to poor absorption of foods.
5. Be sure that you are not over medicated.
6. Work on reducing your antibodies with a selenium supplement
7. Stress reduction, when we’re stressed we don’t digest.
8. Add coconut oil in your beverages, this can add extra calories in your day
9. Avoid caffeine, it can make you less hungry and stress out your adrenals.
In case you would like to read more, here are the links to my books:
Root Cause: https://www.amazon.com/gp/product/0615825796?ie=UTF8&camp=1789&creativeASIN=0615825796&linkCode=xm2&tag=thyroipharma-20
Hashimoto’s Protocol (this is my latest book): https://www.amazon.com/Hashimotos-Protocol-Reversing-Thyroid-Symptoms-ebook/dp/B01HXK6GVQ/ref=sr_1_1?ie=UTF8&qid=1505933035&sr=8-1&keywords=hashimotos+protocol+izabella+wentz
Thank you so much for the helpful info about putting on weight !
Please however could you answer the first part of my message, which was :
‘One question around gluten-free that is rarely addressed, is about whether it’s ok to eat organic, local, ancient, non GMO, non-industrial, varieties of wheat.’
Many thanks again,
Chandan
Chandan Thanks for your question! I am collecting suggestions of different research projects and I will add this to my list of future article possibilities. I would love to hear more about your experiences here on this page! 🙂
Thanks. I hope it’s not too late to respond. I stopped gluten a couple years ago (I have Hashi and have your book Hashi Protocol) but I’m losing too much weight and am starting to re-introduce ancient local organic varieties of wheat with no bad effects. Also I make my own bread with rye sourdough, lots of different gluten-free flours as well as a bit of organic spelt. So I’m not following your protocol exactly. So many people say gluten-free, but don’t address the question of ancient/local/organic varieties. I don’t seem to have any ill-effects from it, so I would love to have your opinion… much appreciation
Chandan – thank you for following this page. For questions pertaining to the protocols please contact my team at info@thyroidpharmacist.com and they will be happy to help you. <3
Tests may not work to diagnose Celiac. If a hair test shows low minerals and high heavy metals…then the intestines may not be absorbing well and the liver may not be detoxing well. Gluten may hurt most people. 100% no gluten/GMO may help heal the gut lining. LDN may help block hidden gluten. Eating gluten may make more attacks on the thyroid. Cheating may make a person go down a notch and not recover from it. It is not enough to take thyroid medicine. A person needs to fix the root cause…gluten usually and stop more destruction of the thyroid and other glands/gut lining/brain/body. A Zyto scan showed my thyroid was 1/2 not working and pituitary was not working 98% which is wear TSH is made. TSH should not be used since it may just mean the pituitary is also hurt by gluten. Going by symptoms for thyroid medicine is needed. Mitochondria may also be hurt. A person should avoid Cl/F/Br/uncooked cruciferous family/soy and more. Zn/Se/enough iron/probiotic/Vit B12/Vit A/Mn and more may help the thyroid work better. Some people are low in iodine which a hair test shows. Taking iodine with Se may help. Se may help stop attacks on the thyroid along with Vit D3/sunlight/no gluten etc. Gluten is wheat/barley/rye..oats/corn/rice which may cause autoimmune attacks. When gluten hurts the gut lining…intestines may not absorb the nutrients needed also to make the thyroid and other glands work right and make cells work right.
Shasha – thank you for following this page and sharing what has worked for you. 🙂
Fantastic Article!
I also noticed a remarkable improvement within three days of going gluten-free.
Before that I felt so bloated I could hardly sleep at night. I was in such deep psychological pain all the time that I prayed to die! That feeling completely lifted in my third day of being gluten-free! I have been gluten-free for 2 years now and the feeling never came back- not even once. My digestion also improved, with uncomfortable bloating being rare instead of part of my daily routine.
Cheryl
Cheryl – thank you so much for your support! <3 I'm looking forward to seeing your progress here.
Would sprouting the wheat grain reduce the gluten content? How about fermentation – bread made using sourdough method of leavening?
I have Hashimoto’s and have reactions to gluten, dairy, soy and get severe joint pain eyes swell and can hardly move and just feel like I am about 100 years old at times instead of the 50 that I am. I do well for a few weeks and not eat things that I should not and get to feeling really good then cheat again and go through the whole pain process again. Self inflicted!! So hard to stay Gluten free but I just know that I have to do it! My question is If I can stick to staying GF can I just try that for like a year before I go to a Doctor and they want to put me on medication? I really don’t want to be put on any medications so can I have Hashimoto’s and not take medications?
Wanda
Wanda – thank you for following this page. Going gluten free is always the first step that I recommend. Through my research I’ve found that a good percentage feel better off gluten. About 20% will actually go into remission by doing so. Some researchers have found that three to six months on a gluten-free diet can eliminate organ-specific antibodies.
10 MOST HELPFUL DIY INTERVENTIONS FOR HASHIMOTO’S
https://thyroidpharmacist.com/articles/10-most-helpful-diy-interventions-for-hashimotosaccording-to-my-clients
TOP 9 TAKEAWAYS FROM 2232 PEOPLE WITH HASHIMOTO’S
https://thyroidpharmacist.com/articles/top-9-takeaways-from-2232-people-with-hashimotos/
Great article, with substantiated information. Thank you for providing this!
Dawn – Thank you for your support! 🙂
Thank you for this excellent and thorough information.
Tanya – you are very welcome! 🙂
Dr. Wentz,
Thank you for your research, hard work and the willingness to share it. I have been diagnosed with HT very recently (1/16/18) due to blood panel results. I was advised to go gluten free, take a vitamin D supplement, as my D level was extremely low on the test, and started on 50 Mcg Levothyroxine. I have been doing my best at refraining from gluten but it seems that from reading about it that it is going to be hard to be 100% gluten free. If gluten still manages to sneak in unbeknownst to me, will it make a marginal difference in my health? Say I can consistently avoid it 90% to 95% of the time, will the small percentage I come in contact with have too much of a detrimental effect that it can hijack my treatment?
I have also bought a selenium and B complex supplement to take to help out.
Thanks,
Fred
Fred – thank you for following this page. Did you know that reactive foods trigger an inflammatory response in the GI tract, leading to malabsorption of nutrients (gluten sensitivity, in particular, has been implicated in causing a Selenium deficiency, a well-known risk factor for Hashimoto’s), and can also produce intestinal permeability whenever they are eaten?
Most people will see a dramatic reduction in gut symptoms, brain symptoms, skin breakouts, and pain by eliminating the foods they are sensitive to. Some will also see a significant reduction in thyroid antibodies! An additional subset of people will actually be able to get their Hashimoto’s into complete remission just by getting off the foods they react to, normalizing their thyroid antibodies, and some even normalizing their thyroid function! Here are a couple of articles you may find helpful.
FOOD SENSITIVITIES AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/food-sensitivities-and-hashimotos
AUTOIMMUNE PALEO DIET
https://thyroidpharmacist.com/articles/autoimmune-paleo-diet
Dr. Izabella,
I took a food sensitivity test bought from a Dr. in my area and did the blood work and it came back with showing nothing on it for me. It was both the IgA and IgG. Just wondering what your comments would be on this.
I was diagnosed with hypothyroidism 9 years ago and have been on levo since. 15 years ago I was told I had an enlarged thyroid and did an ultrasound but results changed from goiter to nodules, but at the time my TSH numbers were normal. Just 5 weeks ago I found out I have Hashimoto’s. I had asked my doctors for years what type I had and was always told it doesn’t matter. Typical! I’m very frustrated that I wasn’t allowed or offered a simple test years ago to find out and start the journey of healing myself.
I am planning on starting the elimination diet soon but still going through literature to try and understand everything better before I start. Since finding out I have hashimoto’s I have tried to eliminate gluten, still learning all the may contain gluten. Do you have a list of what to avoid or check for gluten in? It may be in your books, I’ll have to double check.
Thank you for all your research and information that you have shared with all of us dealing with the same things! I really appreciated it and think it’s amazing that you used yourself to test theories and have then shared them with us.
Looking forward to hearing back from you and your comments on my food sensitivity test. thanks again for taking the time to help!
Thanks!
Jamie
Thanks for your book. It truly saved my life. I have Hashimoto since 5 years now, and I always had week long episodes where I was so tired that I could not leave the couch. For some reason I never could take thyroid medication. Made me even more weak and dizzy. I went to several thyroid doctors, noone knew why those thyroid medication would make me so tired and dizzy. I tried out all different kinds of thyroid medication, but I felt dizzy and tired with all of them … . Even taking only 10 mikrograms per day would weaken me. Then I went to an endocrinologist and she tested me for adrenal fatigue. My cortisol was a little bit low but not so low that she would diagnose me with adrenal insufficiency. ACTH test was normal tough. She gave me low doses of cortisol but that made me dizzy too , so I could not take that medication either. No doctor could help me with my extreme fatigue. After 5 years of being half dead I somehow found out about your book and after reading it I started with glutenfree and dairy free diet, supplemented with a couple of vitamins and minerals, startet to take probiotics and occassionally ate sauerkraut . After only 3 weeks I felt like a human again. I could go outside for a walk without feeling too tired. I could even do a little bit of sports, and I even had the energy to see friends again. After 3 months I felt really good, but still now my TSH is around 5 and I still can’t take my thyroid medtication, because it makes me tired and dizzy. So now I try to strengthen my adrenal gland with adaptogens and see what happens. I am so glad that I found out about all of this no other doctor would tell me about. Thank you so much for your book, I am recommending to every Hashimoto patient I know!. Greetings from Austria.
Lilly – thank you so much for your kind words and support! Most people with Hashimoto’s are likely to have numerous signs of adrenal dysfunction as a result of chronic stress and anxiety. This may worsen symptoms such as feeling overwhelmed, as well as a reduced ability to handle stress and make decisions. Adrenal hormone imbalances may also exacerbate other symptoms such as feeling tired despite adequate sleep, difficulty getting up in the morning, increased effort required for everyday activities, low blood pressure, and mental fog.
If any of these symptoms sound familiar, I recommend trying Rootcology’s Adrenal Support™, which contains a combination of herbs and nutrients known for rejuvenating the adrenals and promoting healthy cortisol levels, so you can lower your stress levels, improve your stress-coping abilities, and say goodbye to adrenal fatigue!
https://rootcology.com/products/adrenal-support
Hello ,I have been gluten free for a few years and my antibodies have reduced by half. I just wonder what your thoughts on Oats were yes or no ?
Paula – thank you for reaching out. If you tolerate gluten free oats then it is certainly an option, but using an elimination diet can help to show you if you are reacting to the foods you commonly eat. These articles should give you some further pointers:
ELIMINATION DIET
https://thyroidpharmacist.com/articles/elimination-diet-for-hashimotos
SIBO
https://thyroidpharmacist.com/articles/sibo-prevent-remission-hashimotos/
Hi. Thank you so very much for all of your research and sharing it with us. I’ve learned so much more from you than all of my doctors. I’m so grateful for your knowledge!
After being sick for about 5 years, I was diagnosed with Hashimoto’s. While I have around 30 symptoms, debilitating fatigue is probably the worst. I am currently doing your protocol from your book and plan to dedicate the next year to the full elimination diet and slowly reintroducing foods. I also have many of the suggested vitamins.
My question is about gluten. Before my diagnosis I tried to find my own solutions. I was gluten free for a year. I felt no better at all. When I reintroduced gluten I had no bad reactions. I felt the same with or without. Although I was significantly happier with gluten in my life. I am now on levothyroxine which doesn’t help at all and makes me feel a little worse actually. And the only change since going gluten and dairy free ( and more- I am in the adrenal section of the protocol now) is that I am miserable. I am just as tired, joints still hurt, still have gerd and dizziness and all the others. I am completely dedicated to heeling my gut and doing everything in my power to stay healthy and fight this. But the thought of a lifetime with out bread and cheese ( my most favorite foods) really really upsets me since I don’t feel better at all without them. It’s a frustrating sacrifice. I’m upset about it daily. As silly as that may sound.
My question is that after another year gluten and dairy free, if I reintroduce them and feel the same- how detrimental is that to my thyroid health? I have tested negative for celiac with endoscopy and colonoscopy. I don’t want to hurt myself but would love your opinion on an occasional sandwich or a piece of pizza a few times a year? The thought of forever without is overwhelming but I don’t want to cause setbacks.
I would greatly appreciate your opinion on reintroduction. Is it possible??
Thank you!!
Rachael – thank you so much for reaching out and sharing your journey with me. <3 I understand how hard this is. We know that intestinal permeability (aka leaky gut) is present in every case of autoimmunity and often precedes the development of Hashimoto’s. Symptoms of leaky gut may include bloating, diarrhea, constipation, stomach aches, acid reflux and irritable bowel syndrome. According to the Institute of Functional Medicine, many people develop IBS 5-10 years before an autoimmune diagnosis. I was one of them and didn’t take my gut health as seriously as I should have. Gut problems are often caused by infections like H. pylori, parasites like Blasto, SIBO, an imbalance of bacteria, and enzyme deficiencies or food sensitivities (especially to gluten, dairy, and/or soy). Even stress can be a factor in gut permeability. Three things MUST be present in order for autoimmunity to occur ...
1. Genetic predisposition
2. Environmental triggers
3. Intestinal permeability (leaky gut)
Developing autoimmunity is like a three-legged stool, all of these factors must be present for autoimmunity to occur! When you remove one of these, you can prevent or stop autoimmune disease. While we can't change genes, if we know the trigger, we can remove it and we can heal the gut. Here are some links which might help:
REVERSING AUTOIMMUNITY? AND THE PERFECT STORM
https://thyroidpharmacist.com/articles/reversing-autoimmunity-and-the-perfect-storm/
IS HASHIMOTO’S HYPOTHYROIDISM GENETIC?
https://thyroidpharmacist.com/articles/is-hashimotos-genetic
WHAT’S CAUSING YOUR LEAKY GUT
https://thyroidpharmacist.com/articles/whats-causing-your-leaky-gut/
Hi Izabella, I recently got my results from the Alletesss intolerance testing. I have quite a few reactions. Some were surprising, others were not. My question is do you personally avoid all of them or depending on their ratings (i.e. 1’s, 2’s or 3’s) I read somewhere that only 2’s and 3’s need to be avoided. What is your experience with that? Thanks, Krystine
Krystine – thank you so much for reaching out. Please email my team at info@thyroidpharmacist.com and they will be happy to help you. 🙂
Thank you for your informative website! I’m just about to start the adrenal protocol and have been gluten free the last 2-3 weeks now. I do not have obvious gut symptoms, but just overall feel like I should have more energy. I’m really not bad off yet in terms of symptoms. I can function ok, but want to be at my best to keep up with my 4 kids. My thyroglobulin is 21 IU/mL and lab range is normal up to 3.9. My TSH was the highest ever in June at 3.74 uIU/mL. Knowing I have Hashimoto’s now I want to try to determine what my triggers are and reduce the attack on my thyroid before things worsen. My question is, do I need to have a gluten free kitchen? My daughter likes to bake now and then and I have to help her work with gluten flours. I also handle gluten bread when making sandwiches for my kids most days. My sister-in-law has Celiac and needed to have a gluten free kitchen. Is this the case for Hashimoto’s too?
Thank you so much for helping me to help myself through your books and website,
Jhannea – thank you for reaching out and sharing your journey with me! <3 I wish I could give you more direct advice but, each person will react differently. I would advise you to ask your trusted clinician who’s care you are under. <3
Hi Dr. Izabella! I love your work and am so grateful I found it so early in my Thyroid journey. I am wondering if you have any optimal reference ranges for the IgA and IgG results? I have been tracking my thyroid panels and antibody levels on my own with my PCM for about a year. I saw an Endocrinologist, whom looked at my 3.74 TSH & ultrasound and said I was fine, nothing to worry about and an OB would be better to talk to about stress and hormones. I’ve had to wait for months for an appt with a new endo, hoping this one will be better informed on up to date tests and optimal ranges vs. standard ranges. I keep track of everything and went gluten-free on my own recently due to family history of Celiac’s and my results. I feel better and am trying to transition to AIP diet as well. My biggest question is about the reference ranges for the IgA&G tests as I can’t seem to find much on optimal IgA&G. Thank you for you work & time!
Mariah – thank you so much for sharing your journey! I am happy to hear you are better! <3 Please email my team at info@thyroidpharmacist.com and they will be happy to help you.
Hi Dr. Izabella, i felt much better on a gluten free & dairy free diet. My TPO Antibodies decreased from 26 to 14 in 3 months when taking selenium as you recommended. TSH: 3.84; free t4: 1.4; free T3: 3.1. Are my thyroid levels are all in optimal range? Should I take Gluten/diary digest before, with, or after meal?
Connie – thank you for reaching out. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. I’ve found Gluten/Dairy Digest to be helpful in uncertain situations. Gluten/Dairy Digest contains enzymes that assist in breaking down gluten and dairy proteins and can help to lessen reactions to them. These enzymes can be very helpful for those with gluten and dairy sensitivity in times where you’re concerned about cross-contamination or when you’ve accidentally consumed something you shouldn’t have. While they can minimize the reactions to gluten and dairy, they are not likely to completely eliminate them. So, I don’t recommend trying to eat a pound of cheese or a loaf of bread just because you’re taking this type of supplement. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Hello! I definitely have reactions to wheat. However, I have found that I can tolerate sourdough with no issues. I assume it has to do with the starter bacteria. My question is: if I don’t react to it, is it safe to eat or should I assume that it is causing the same damage as regular wheat just with fewer symptoms?
Rebecca – thank you for reaching out and sharing. Until you eliminate the foods from your diet, it will be nearly impossible to correlate your symptoms with a food. This is because food sensitivities can take up to 4 days to manifest. You will only notice that you are reacting to the food if you withdraw it for a time-period of at least 3-4 days. The gold standard or the most accurate test for uncovering reactive foods and individual food sensitivities is actually the elimination diet. In contrast to other diets that simply exclude common problematic foods, an elimination diet is done to determine what particular food intolerances the individual may have. An elimination period of at least 2-3 months is a good starting place, but you may want to continue if you feel that you still have more healing to do. Then you can try a new food every 4 days and monitor yourself for reactions. Going through an elimination diet will help you figure out your own individual food triggers and your specific response to each trigger food. Here is an article I hope you find interesting!
https://thyroidpharmacist.com/articles/elimination-diet-for-hashimotos
Hi Dr. Izabella,
Thank you for the article.
I discover that I’m hypothyroid since 2009 and since this time I’m taking the medicine, I have all the symptoms, such as; IBS, Brain fog, fatigue, hair loss, cold intolerance, joint pain, weight LOSS, and anxiety.
I tested Celiac, and biopsy shows positive while the blood test shows negative but at the same time I’m at high risk (according to the results). The doctor says that the blood test is more accurate than the biopsy (!!).
my question is; why when I start following GF diet I don’t feel comfortable and I’m bloating all the time also having severe constipation? noting that I already stopped dairy products a long time ago.
Rasha – thank you for reaching out and sharing your journey. <3 I understand how frustrating and hard this can be. We know that intestinal permeability (aka leaky gut) is present in every case of autoimmunity and often precedes the development of Hashimoto’s. Symptoms of leaky gut may include bloating, diarrhea, constipation, stomach aches, acid reflux and irritable bowel syndrome. According to the Institute of Functional Medicine, many people develop IBS 5-10 years before an autoimmune diagnosis. I was one of them and didn’t take my gut health as seriously as I should have. Gut problems are often caused by infections like H. pylori, parasites like Blasto, SIBO, an imbalance of bacteria, and enzyme deficiencies or food sensitivities (especially to gluten, dairy, and/or soy). Even stress can be a factor in gut permeability. Here is an article you might find interesting.
6 DIFFERENT ROOT CAUSES
https://thyroidpharmacist.com/articles/6-different-hashimotos-root-causes/
Hi,
After doing a IgG test, my elevated foods included milk, gluten and eggs. My soya bean level was normal.
I notice that a lot of the recipes are soy free but not egg free.
Do i listen to my food panel and cut out eggs and use soy as an alternative or would you recommend the opposite. I also try and avoid nuts due to my partner being allergic (almonds are his worst which means no almond milk for me)
I’ve had Hashimotos since I was 7 (which is 17 years ago now) and I am finally trying to take a step towards improving my symptoms.
Emily – thank you for reaching out. <3 The most common food sensitivities found in people with Hashimoto’s are gluten, dairy, soy, grains (corn, in particular), eggs, nightshades (potatoes, tomatoes, and peppers), nuts, and seeds. Did you know that reactive foods trigger an inflammatory response in the GI tract, leading to malabsorption of nutrients (gluten sensitivity, in particular, has been implicated in causing a Selenium deficiency, a well-known risk factor for Hashimoto's), and can also produce intestinal permeability whenever they are eaten? Most people will see a dramatic reduction in gut symptoms, brain symptoms, skin breakouts, and pain by eliminating the foods they are sensitive to. Some will also see a significant reduction in thyroid antibodies! An additional subset of people will actually be able to get their Hashimoto's into complete remission just by getting off the foods they react to, normalizing their thyroid antibodies, and some even normalizing their thyroid function! Here are some articles you may find helpful:
FOOD SENSITIVITIES AND HASHIMOTO'S
https://thyroidpharmacist.com/articles/food-sensitivities-and-hashimotos
AUTOIMMUNE PALEO DIET
https://thyroidpharmacist.com/articles/autoimmune-paleo-diet
HOW AVOIDING SOY CAN BENEFIT HASHIMOTO’S
https://thyroidpharmacist.com/articles/soy-and-hashimotos/
You always seem to be talking about Hashimoto’s when I’ve read your postings and articles. What about those of us who have regular Hypothyroidism…should we be going gluten-free as well? I’ve tried to find decent tasting gluten-free bread that is organic and so far, have not found any. I am not a baker or a cook, so it would be wonderful if I could find decent-tasting organic, gluten-free bread to buy. Any suggestions?
Susan – thank you for reaching out. Hypothyroidism is associated with a lack of thyroid hormone that can occur as a result of a variety of different factors such as iodine deficiency, surgical removal of the thyroid, or damage to the thyroid. Most cases of hypothyroidism in the United States and other countries that add iodine to their salt supply are caused by Hashimoto’s. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target.
We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are a couple articles you might find interesting:
ARE YOU DOING EVERYTHING FOR YOUR THYROID BUT NOT YET WELL?
https://thyroidpharmacist.com/articles/are-you-doing-everything-for-your-thyroid-but-not-yet-well/
DO YOU HAVE HYPOTHYROIDISM OR HASHIMOTO’S OR BOTH?
https://thyroidpharmacist.com/articles/do-you-have-hypothyroidism-or-hashimotos-or-both/
After experiencing many unwanted GI symptoms for almost 2 years and being told is was healthcare-worker “stress” and IBS, I finally succeeded in advocating for further testing and a GI workup to be diagnosed with Celiac Disease and severe nutritional deficiencies. Three months after being diagnosed and going strict gluten-free, my GI symptoms improved but my fatigue and energy levels did not – I was diagnosed with thyroid cancer resulting in 2 surgeries, 8 months apart, to remove my entire thyroid and diseased lymph nodes. So now it’s been almost a year of finally being able to manage the autoimmune symptoms of Celiac only to be setback twice by thyroid surgeries and multiple prescription hormone adjustments, which has been pretty discouraging. A lot of your resources have been really helpful already!
Are there specific resources/recommendations you have that would be good for someone with surgically-induced hypothyroidism/cancer and Celiac Disease to achieve restored energy and long-term safety in terms of protecting nutritional/autoimmune health? I’m only in my late 20s, and don’t want to start making mistakes now that will have negative long-term effects for the rest of my life.
– Nicole
Nicole – thank you so much for sharing your journey. ❤️ I’m so sorry you had to go through all of this! Most thyroid conditions (Hashimoto’s, Graves’, thyroid cancer) result from an immune system that is out of balance. This can be caused by nutrient deficiencies, food sensitivities, toxins, a gut imbalance, poor stress response and/or a chronic infection that can be anywhere in the body. Even when the thyroid is taken out surgically or treated with radioactive iodine, the immune imbalance still persists in many cases, and a person may go on to develop additional health conditions, and still feel unwell. For those who have had a thyroidectomy, in addition to making sure your thyroid medications are optimized, I also encourage you to take on lifestyle changes and functional medicine, to ensure that the underlying triggers that led to the development of your condition don’t lead to another autoimmune condition.
Here are some articles that I hope you find helpful
TOP THINGS YOU SHOULD KNOW ABOUT THYROID CANCER
https://thyroidpharmacist.com/articles/top-things-know-thyroid-cancer/
THE MANY FACES OF HASHIMOTO’S
https://thyroidpharmacist.com/articles/the-many-faces-of-hashimotos/
10 FACTS ABOUT THYROID DISEASE
https://thyroidpharmacist.com/articles/need-know-thyroid-disease/