Sleep deprivation is an important root cause or exacerbating factor for various health conditions — and it’s also all-too-common in our modern world.
For some people, prioritizing sleep is the biggest hurdle, but others may struggle with sleep despite their best efforts, due to physiological factors. While some people with Hashimoto’s struggle with insomnia, for most of my life, I actually had the opposite problem… I could fall asleep anytime, anywhere. In fact, I actually had an issue with hypersomnia, or sleeping too much.
I once took a nap in undergrad at a crowded bar, during a daytime event (and this was without any alcohol!). Before I was diagnosed with Hashimoto’s, I needed to be in bed for at least 11 hours each night, in order to function and get through my classes without feeling like a zombie. Even with 11 hours of sleep, I was always tired. I’ve focused a great deal on resolving this with my previous articles on resolving fatigue.
However, many of my clients have reported issues with falling asleep, staying asleep, and waking up too early — symptoms that may be classified as insomnia, given a long enough duration. Over the years of helping my clients, I have found that there can be various root causes of sleep issues, but there are a few low-hanging fruits that can help about 50 percent of people, as well as some more advanced things, that I have found to help about 80 percent of people with getting better sleep.
Furthermore, I had to dig a little deeper for certain clients that left me stumped (I’ll share some insight into some of their root causes), as well as for myself, when I struggled with insomnia while pregnant (this was due to a nutrient deficiency that I’ll discuss in this article), and more recently, due to a hormonal issue. Additionally, my husband has struggled with sleep issues (his issue was also nutrient-related, though it involved too much of the same nutrient).
And then, of course, my son initially took after daddy instead of mommy in the sleep department. During the first few years of life, he woke up every two hours, all night long, for almost three years. (I am so excited to share that he’s now sleeping from 8:30 pm to 8 am most nights!) I am still deeply triggered by the phrase “sleeping like a baby”… a phrase only uttered by those who have clearly never had children. 😂
As such, I have spent a lot of time NOT SLEEPING, while focusing on sleep, over the past few years — and I know firsthand the effects of sleep deprivation… because when the baby doesn’t sleep, no one sleeps. 🙂
I often see healthcare professionals without children, preaching about the many issues that are caused by sleep deprivation. They tell people to “just prioritize sleep.” I also see baby trainers who focus on promoting “sleep habits and routines” as be-all-end-all solutions to sleep. I will cover the fundamentals of sleep hygiene for completeness’ sake, but if you’ve been doing ALL of the “basic” things and are still not sleeping, this article will hopefully provide you with additional root cause relief.
This article will focus on different root causes of sleep issues — how to tell which one applies to you, and what to do about it — as well as ways to deal with sleep deprivation for the mamas and dadas with children.
Fortunately, our son, who is now five years old, sleeps a solid 11 to 12 hours — and that means that I get to sleep too. 🙂 I will share more about the reason he was having frequent night wakings, and how we finally got him to sleep so well.
Read on to learn more about:
- Sleep hygiene: a fundamental checklist
- Medications and natural protocols that act like bandaids (ones I do and don’t recommend)
- Easy starting point protocols that can help 50 percent of people get more sleep in just a few days
- Deeper protocols that have helped 80 percent of my clients get more sleep
- Extra deep ideas for the special 20 percent circumstance situations
- Protocols for sleep-deprived parents 🙂
The Importance of Sleep
Sleep is the primary healing time for both our bodies and our minds — and when we don’t get adequate, quality sleep, our health suffers.
All-cause mortality rates may be three times higher (or even more) in sleep-deprived people! [1]
Lack of sleep is a huge stressor on the body and is the quickest way to HPA-axis disruption and adrenal dysfunction, which can initiate — and perpetuate — autoimmune thyroid disease. [2]
Sleep deprivation can also cause symptoms such as fatigue, brain fog, insomnia, blood pressure issues, and a decreased ability to handle stress.
Most of my clients with Hashimoto’s hypothyroidism have some degree of adrenal issues.
The adrenals are two small glands located on top of each kidney that release hormones such as cortisol and adrenaline. These “stress hormones” impact many important functions throughout the body. They help establish our stress tolerance, tame inflammation, regulate blood sugar and body fat, control potassium and sodium levels (impacting blood sugar), influence libido, and help with keeping us young by ensuring we are in a restorative repair mode… among other things.
Getting good sleep, at regular intervals, is incredibly important for adrenal balance, and can help us reset our body’s circadian rhythm. It’s also the most fundamental recommendation of all for adrenal health.
It’s especially important for us to get “deep sleep,” which is the restorative stage that promotes muscle repair and metabolism. Making sure our brain gets REM (rapid eye movement) sleep is also vital, as that is the stage where the brain filters out the information it received during the previous day, and moves information from our short-term memory to our long-term memory. [3] (For this reason, quality sleep helps reduce brain fog.)
While getting a good night’s sleep is just a matter of making sleep a priority for some people, others need help falling and/or staying asleep.
When you have insomnia, it’s obvious that you don’t get enough sleep due to the sheer quantity of time spent sleeping. However, you are also not getting enough sleep when you have hypersomnia, which is likely due to poor sleep quality.
Let’s first take a look at how the thyroid is affected by a lack of sleep, and then explore the strategies to turn things around and make a good night’s sleep a reality.
The Thyroid and Sleep Connection
The circadian rhythm is the body’s natural 24-hour biological clock. It helps us to feel energetic in the morning when the sun is out, and sleepy in the evening before bed. Sleep helps to set and maintain the circadian rhythm — when that rhythm is thrown off, it can affect everything in the body, especially the immune system and hormone balance. An out-of-balance circadian rhythm can leave us with fatigue during the day and increased sugar cravings, as well as make it hard to fall asleep at night, even when our body is tired. [4]
The endocrine system, which is composed of all the hormones in the body, is closely entwined with the circadian rhythm. Thyroid Stimulating Hormone (TSH) is known to be influenced by the sleep-wake cycle. In a 2019 study of almost 5000 participants, those who slept less than seven hours per night, and those who slept greater than eight hours per night, were more likely to have subclinical hypothyroidism compared to those who slept seven to eight hours per night, which is what the researchers have defined as the “optimal sleep duration.” [5]
I wish I had known about this when I was sleeping >10 hours per night in my 20s, yet struggled with daytime fatigue!
One study showed that slow-wave sleep, which is the deepest dreamless sleep, was reduced in those with hypothyroidism. [6] This deep sleep is where the body heals, repairs, and detoxifies, so not getting enough of this critical sleep phase can impact the body’s ability to heal from Hashimoto’s.
Interestingly, a 2006 study found that third shift workers who typically have disrupted sleep patterns due to the nature of working overnight, were found to be at greater risk for developing thyroid antibodies compared to daytime workers. Subsequent research supports that shift work can negatively impact thyroid health as well. [7]
There are links between Hashimoto’s and sleep apnea, as well as with hypersomnia, the condition I had throughout college and grad school where I slept a lot, but never felt rested. Needless to say, having a deficiency in thyroid hormones can certainly make someone feel sluggish, fatigued, and sleepy.
Because thyroid hormones play such a big role in sleep quality, I suggest that anyone with Hashimoto’s who is struggling with sleep, begin by running a full thyroid panel. Thyroid labs, especially TSH, free T3, and free T4, are going to be critical for determining if you need to start, increase, or reduce the dose of your thyroid hormone medications, as well as if you’re on the right thyroid medications.
Excess thyroid hormones in the body can also lead to insomnia, so testing can help with determining if the thyroid is overactive and if sleep issues are stemming from that. [8]
As levels of TSH can fluctuate depending on the day, especially in the early stages of thyroid dysfunction, I also recommend testing for thyroid antibodies for Hashimoto’s (thyroid peroxidase and thyroglobulin antibodies) and Graves’ disease (TSH receptor antibodies). Antibodies can be elevated for up to a decade before a change in TSH is detected.
The Conventional Approach to Insomnia
Sleep hygiene is a term that refers to all of the practices we put in place to ensure that we get a quality night of sleep. This can include the sleeping environment we set up for ourselves, our activities throughout the day, and the use of therapeutic devices and techniques to help us wind down for the night and achieve adequate rest.
These are often the first place to start for people who are experiencing insomnia, and are widely recommended by health practitioners — although to be completely transparent, many of my clients have told me that conventional doctors have never discussed these approaches, and are more likely to write a prescription for a sleep medication.
Tips to Promote Better Sleep Hygiene
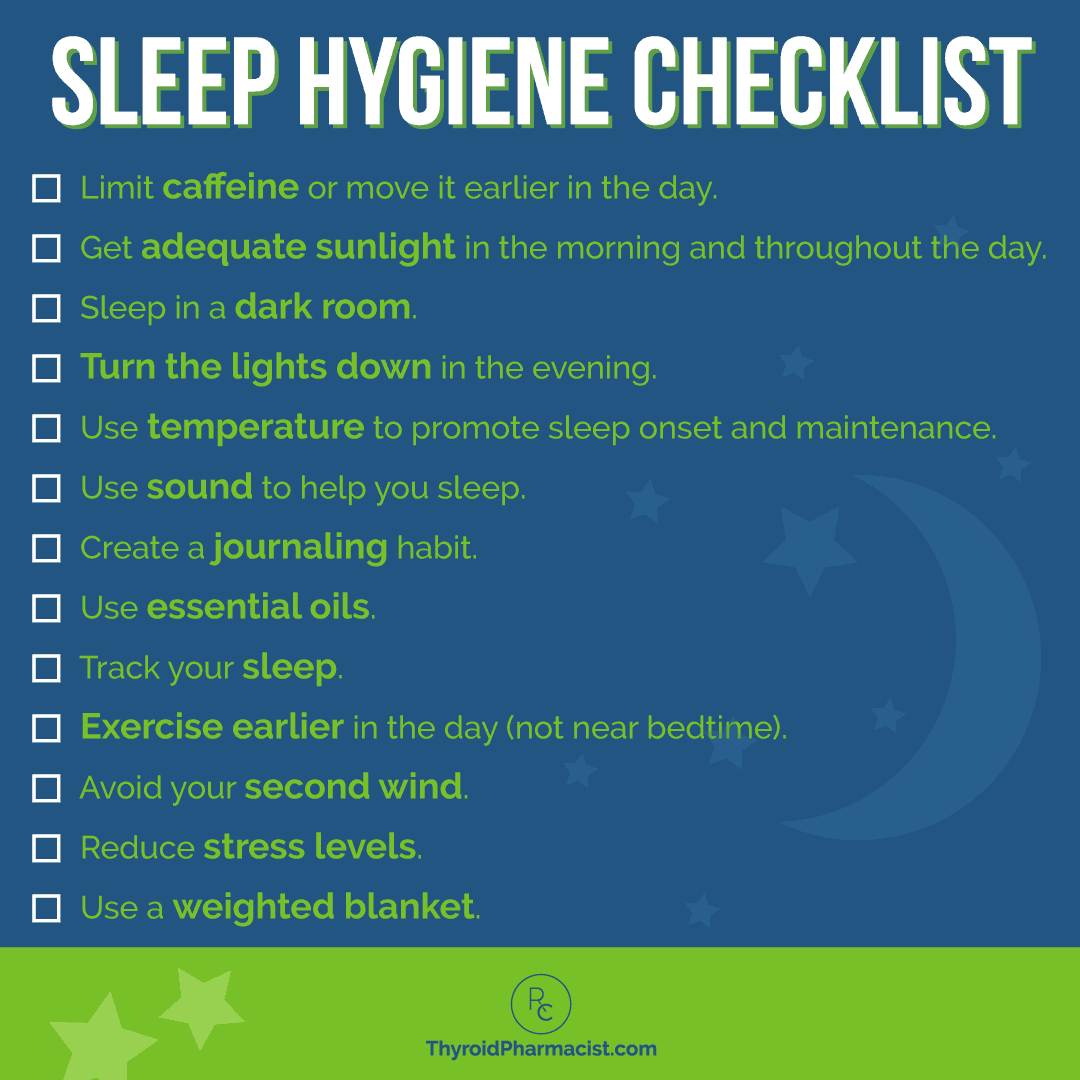
Here’s a checklist of steps you will want to begin with, to promote good sleep hygiene (I’ve tried to list them out in the order that I have found to be most helpful).
- Limit caffeine or move it earlier in the day. Caffeine intake can certainly impact sleep, especially for those who are particularly sensitive to its stimulating effects. I used to consider myself to be a light sleeper… until I dropped my caffeine intake to two black teas each morning, instead of having six to eight black teas a day (including my usual bedtime black tea). I was so surprised when things no longer woke me up at night! Although some may find completely eliminating caffeine to be beneficial, I understand that this is not going to be possible for other people. Limiting caffeine to the morning only, preferably before 2 pm, or at least eight hours before bedtime, can be helpful. (If giving up caffeine sounds daunting, there are actually a bunch of great coffee alternatives to try — I suggest some later on in this article. :-))
- Get adequate sunlight in the morning and throughout the day. The amount, type, and timing of light we get throughout the day can have a profound effect on our circadian rhythm. [9] I recommend getting outside for at least 20 minutes within the first hour of waking up (ideally before 8 am, but even if you are waking up later, getting outside ASAP will help to shift your circadian rhythm), and avoid wearing sunglasses if possible. Sunlight on our retinas helps activate morning cortisol production and helps set our circadian rhythm for the day. Keeping the body in tune with natural cycles of sunlight throughout the day, and darkness in the evening, will help regulate sleep hormones and promote better nighttime rest. I know this is tough in Northern climates, especially in the winter, so using devices such as a blue light lamp in the morning and blue light blocking glasses at night, can help mimic these natural cycles. For me personally, morning sunshine and blue light therapy in the morning during the winter, have been critical components of reversing morning fatigue and boosting my cortisol levels in the morning.
- Consider changing your mattress. Having a mattress that properly supports your body and is free of toxins, can make or break your sleep patterns. Make sure that your bedding is free of allergens as well. One of my favorite non-toxic mattress options is Obasan. You can read more about reducing your toxic load in your home, in my articles on flame retardants and improving indoor air quality.
- Sleep in a dark room. Here are a few ways to make your room darker:
- Use blackout curtains.
- Turn off all lights (including nightlights).
- Try wearing a sleep mask.
- Cover any blinking or tiny blue lights in your home. Use black tape to cover lights on smoke detectors (be sure that you check regularly to ensure the smoke detector is still working), or on anything else that has a small light that is always on. I cannot stress how important this is! I recently started waking up in the middle of the night without any changes in diet or supplements. This continued for a week or so, and then I noticed that the sticker I had put over the blue light on a light switch in my bedroom had fallen off. This tiny but mighty blue light managed to shine enough light to wake me up! Once I put the sticker back on, those night wakings stopped completely!
- Ensure that you have an alarm clock that allows you to shut its light off.
- Ensure that your phone does not blink throughout the night if you have it on.
- Turn the lights down. For at least a half-hour to two hours before going to bed, try to avoid bright lights. Here are some things to consider
- Turn off your lights after sunset. Candlelights and salt lamps, as well as certain red lights, can provide ample illumination for most evening activities, while still promoting melatonin production.
- Stop watching TV and looking at your phone or computer two hours before bedtime. You can also use a blue-blocking app, the “night mode” setting on your phone, or opt for blue blocker glasses, to minimize the effect of bright screens on melatonin. This has been a big game-changer for my hubby! (The brand True Dark makes some fun glasses that block out blue light — if you want to test them out, you can get 10% off your purchase when you use code IZABELLA at checkout!)
- If possible, avoid screens entirely after dark. Even five minutes of white light from a screen shuts off melatonin production and can sabotage our quality of sleep.
- Use temperature to promote sleep onset and maintenance. [10] One way to improve sleep quality is by maintaining an optimal body temperature before sleep onset, as well as throughout the night (which can be extra challenging for those with hormone imbalances). This can mean adjusting the temperature in the room itself, as well as using techniques to adjust the core body temperatures. Here are some examples:
- Heating up the body to prepare for resting: It is widely known that bedtime routines that heat up the body, like taking a hot bath, or using a sauna, allow the body to relax, and I’ve found that the most beneficial form of sauna therapy involves using an infrared sauna. Not only will you be sweating out toxins, but you may also find that you feel much better, more rested, and less stressed after just one session! Infrared saunas also raise and then lower the body’s temperature, which is conducive to deeper sleep. I love and use the Sunlighten sauna regularly, which helps me to detox and relax. (However, please note that sauna use may not be recommended in specific circumstances, or for those with certain medical conditions. You can learn more about infrared sauna contraindications in my article on saunas and Hashimoto’s.)
- Cooling down the body to support sleep onset and maintenance: Have you ever tossed and turned and had trouble falling asleep, even though you were tired, only to realize you were too hot? While warming rituals can put us in a relaxed and tired state, cooling off the body actually helps with sleep onset and maintenance, and being too warm can actually interfere with sleep! [11] When I was a little girl, I noticed that I would frequently wake at night due to nightmares, if the room where I slept was too hot. Interestingly, researchers have in fact confirmed the link between nightmares and warm sleeping environments that cause the body to stay in REM sleep for too long. To counteract this, you can lower your thermostat at night or open a window.
- The ideal sleeping temperature is between 60 and 67 degrees Fahrenheit, although some individuals with poorly controlled hypothyroidism might find that to be too cold. I generally keep my room temperature between 65 and 70 degrees when going to sleep. Surveys have found that people who sleep in cooler rooms tend to fall asleep faster and stay asleep longer. [12]
- Consider your bedding materials and PJs. Linen and cotton are materials that tend to be more breathable than synthetic materials like polyester. Some individuals may vary the thickness of their blankets, as well as enjoy sleeping with very limited clothing (or even nude) to ensure that they are not overheating at night. For those that may experience hot flashes, I like Cool-jams’ pyjamas that wick away moisture. 🙂
- My husband loves Chilipad by Sleepme to help regulate his body temperature during sleep. It utilizes water to match the body’s heat load, which not only improves comfort, but also affects core body temperature, recovery, and deep sleep. I suggest checking out their Chilipad Cube Sleep System!
- Use sound to help you sleep. Soothing sounds can help us get a more restful sleep all night long. Here are some things that can help create a peaceful sleep space:
- Use a white/pink noise machine to block outside sounds.
- I love using air purifiers to reduce the effects of toxins like allergens and molds. The AirDoctor is a great air purification system which doubles as a white noise machine (it also has a “sleep” mode, so no annoying blue lights to cover).
- The Hatch Rest is another option that I like — I used it with my son, as it plays lullabies. 🙂
- Turn on a fan.
- Ensure your phone and other devices are turned off or set to “silent.”
- Wholetones – This frequency-based therapeutic music can help you to fall asleep and promotes more restful sleep… like lullabies for adults. It even worked on my son when he was a baby and refused to nap in the car!
- Dodow – This is a metronome-based sound that helps to retrain the brain to fall asleep. It’s scientifically designed to soothe brain activity, slow your breathing, and relax your body.
- Use a white/pink noise machine to block outside sounds.
- Create a journaling habit. Oftentimes, the inability to fall asleep arises from an overactive mind. Sometimes, just the act of writing down the thoughts that are on our minds, allows us to let go, de-stress, and rest. Try one of these methods right before you go to bed:
- Brain dump – Simply write down every thought that comes into your head. Put all of your worries, fears, and events of the day on paper, without judgment. Then, close the notebook and let those thoughts go.
- Make a to-do list – Write down all of the tasks in your head that you need to get done, and assign them each a day that you will tackle them. You’ll rest better knowing that you have a plan and don’t have to keep the list in your brain. I credit my daily to-do list with my ability to fall asleep with ease most nights.
- Start a gratitude journal – Take a few moments to write down the things you are thankful for each day, and notice how this positive focus begins to shift your attitude and your ability to find rest.
- Use essential oils. This is particularly helpful for those who have a cortisol spike at night, or catch that “second wind.” Research suggests that inhaling certain essential oils can help to lower stress and promote sleep. [13] There are a few options for using essential oils, such as in a diffuser near the bed before/during sleep, placing a couple of drops on your pillow, or mixing them with a carrier oil (such as coconut oil) and massaging them onto the skin before bed. I highly suggest giving lavender, cedarwood, bergamot, vetiver, Roman chamomile, neroli, and/or frankincense a try!
- Track your sleep. I like the Oura Ring device for tracking sleep. The ring can track how much time it takes until we fall asleep (sleep onset), how many times we wake up at night, and how much REM sleep and deep restorative sleep we get each night, as well as offer coaching suggestions for improving our sleep. I wore this ring for almost two years, but stopped wearing it after I had my son, because I thought it was too judgy: “You woke up 17 times last night, you need more sleep!” Yeah, thanks for that, Oura Ring! That said, I encourage you to see how different foods, supplements, and sleep hygiene strategies impact your personal sleep pattern and depth.
- Exercise earlier in the day (not near bedtime). Exercising raises cortisol levels, and although this is generally a good thing, it’s highly energizing and can interfere with sleep. Try to exercise no later than two hours prior to your bedtime. If you love to exercise in the evenings, consider sleep-promoting exercises such as restorative yoga, stretching, and tai chi. Water exercises have also been shown to be helpful in promoting sleep. Studies have shown that this form of exercise may help improve joint tissue and reduce the pain and symptoms of arthritis, which can keep many people up late at night. [14] A gentle water aerobics class, or a few laps in the pool, may also be beneficial in relieving aches and pains, as well as promoting a restful night’s sleep.
- Identify your “second wind” time window and avoid it. After sunset, most of us naturally get tired, and we have an ideal window of opportunity to fall asleep. This can happen between 8 pm and 11 pm, depending on the season and time zone. (Hint: the best way to know your personal “tired” window is to listen to your body.) If you decide to stay up past that window, the body may get a “second wind” of energy, and before you know it, it’s 2 am and you’re still awake! Going to bed when you feel tired (for most of us, this is before 11 pm) will also allow you to get better sleep and feel more rested on waking than if you went to bed later and still got the same amount of sleep. Please note that getting a “second wind” earlier than expected in the evening, is often a consequence of adrenal issues.
- Reduce stress levels. Do you have a hard time clearing your mind before bed? Do you worry about things you feel are not necessary at bedtime? There are a few things you can do to help your mind relax and shut down before bed:
- Try stress-relieving exercises. These can do wonders to help the brain shut down, recuperate and prepare for another day. Some exercises that I recommend include:
- Deep breathing exercises
- Neurofeedback
- Yoga
- Meditation (finding guided meditations or using a device like the Muse can help get you into a meditative state)
- Try stress-relieving exercises. These can do wonders to help the brain shut down, recuperate and prepare for another day. Some exercises that I recommend include:
- Use a weighted blanket. Weighted blankets resemble standard blankets, but are weighted with beads or pellets to make them heavier than a standard blanket. They are known to help relieve anxiety and stress, and are a common tool used with children who are autistic or have behavior issues.
In my latest book, Adrenal Transformation Protocol, I outline a four-week plan which can help you assess your adrenal health, understand why you might be sleeping poorly, and optimize your adrenals so you can have lots of energy during the day and get restorative sleep at night. If you are interested in learning more about how to lose that “tired-but-wired” feeling and regain your energy and vitality, you can order my book here.
Sleep Medications
In addition to recommended lifestyle changes, the conventional medicine approach to dealing with sleep issues often involves prescription sleep medications, such as Ambien or Restoril. While there might be circumstances in which one of these medications is indicated, they can often become habit-forming and lead to other unwanted symptoms, such as daytime drowsiness, dizziness, lightheadedness, headaches, gastrointestinal problems, allergic reactions, and memory/performance problems. [15] (I could write a whole article on this topic, as I am a pharmacist after all, but I will spare you the details, and assume you are here for root cause solutions.😉)
For some individuals, Benadryl may work to help them sleep better, as it is an antihistamine, and high levels of histamine are actually correlated with increased alertness and poor sleep. [16] However, I don’t recommend using this medication on a regular basis due to its numerous side effects. This was a high-risk medication I often recommended against, especially for the elderly, in my consulting pharmacist days. In addition, there are more natural ways to balance histamine in the body.
Fortunately, there are many holistic approaches to getting a better night’s sleep that don’t come with unwanted side effects, but may promote better thyroid and adrenal health instead!
The Alternative Medicine Approach to Occasional Insomnia
Alternative medicine professionals often focus on herbal remedies for sleep, such as the hormone melatonin, or the herbs chamomile and passionflower.
Melatonin is a naturally occurring hormone that promotes sleep. It is also available as a supplement. Many years ago in a previous career, I studied melatonin to support parents of children with autism. While I think it is generally safe for short-term use, it may have some negative long-term consequences of suppressing our own melatonin production, as it is dosed in megadoses compared to what the body would normally make on its own. (There is some promising information on megadose melatonin for cancer suppression, but for purposes of sleep, it may not always be the right choice.)
Furthermore, melatonin is mostly helpful for people who have trouble falling asleep, but not super helpful for those who wake up too early, or wake up too frequently at night. In my experience, a dark room can work just as well as melatonin, especially for jet lag and for individuals who are not getting the proper input from the sun into their retinas, such as shift workers and those who are visually impaired.
A few herbal teas I might recommend for occasional use include:
- Chamomile tea: Chamomile is an herb well known for supporting sleep. In addition, recent research suggests it may have thyroid benefits, including decreasing the risk of thyroid cancer by up to 80 percent. [17]
- Catnip tea: Although catnip can cause cats to go wild, in humans, it can have calming effects when consumed as a tea. Catnip contains constituents called nepetalactones, which have been found to have sedative effects. [18]
- Passionflower tea: Studies suggest that passionflower might help relieve insomnia and anxiety, as it appears to boost the level of gamma-aminobutyric acid (GABA) in the brain, which lowers brain activity and can lead to relaxation and better sleep. [19]
- Tulsi tea: Also known as holy basil, tulsi has been used for thousands of years to support a healthy stress response and promote more restful sleep. This is actually one of my favorites. [20]
Some of these can work well on occasion. However, for those who are having problems sleeping regularly, we should take a deeper dive into possible root causes, to ensure we aren’t overlooking other important causes of sleep issues.
Now, let’s dive into my root cause approaches for getting a better night’s sleep, and explore the strategies that have helped the majority of my clients feel more rested and energized!
The Root Cause Approach to Insomnia
In my initial functional medicine training, I learned about two main drivers of sleep issues: magnesium deficiency and adrenal dysfunction.
Addressing these two issues resolved sleep issues for about 50 percent of my clients, and since these two issues are pretty common, I think this is a reasonable place to start for most people.
Magnesium Deficiency and Sleep
Magnesium deficiency can be tied to insomnia. [21] Magnesium is important in balancing our levels of glutamate (an excitatory neurotransmitter that can lead to sleep deprivation and anxiety), as well as producing serotonin (a precursor to melatonin, our sleep hormone).
Many people with Hashimoto’s have a magnesium deficiency, [22] and supplementation can relieve a long list of symptoms, including insomnia. Other symptoms that might be a clue that you have a magnesium deficiency include anxiety, depression, headaches, acid reflux, fatigue, constipation, cramps, PMS, and more. A sensitivity to loud noises is a BIG red flag for magnesium deficiency. An ex-boyfriend of mine used to have a bumper sticker on his car that said: “It’s not too loud, you’re just old.” I think I would like to make one that says: “It’s not too loud, you’re just magnesium deficient”… or maybe: “you’re not too old, you’re just magnesium deficient”…
Okay, I’ll stop, but be sure to check out my full article on magnesium and thyroid health to learn about more symptoms!
You can choose to take a relaxing Epsom salt bath to reap the benefits of magnesium, or take an oral supplement of magnesium citrate, at a dose of ½ to 1 teaspoon in 8 ounces of water (or maximum 400 mg), before bed.
Note: The citrate version of magnesium may cause sleep issues in some. If so, magnesium glycinate may be a better option. However, those with anxiety may find that magnesium glycinate can exacerbate their anxiety levels, if they have a gene variation that converts the glycinate to glutamate (an excitatory neurotransmitter that causes anxiety/irritability in excess). In those with oxalate issues and B6 deficiency, the glycine can over-convert to glyoxylate, an oxalate precursor, and cause a whole host of unpleasant symptoms. As a side note, a P5P supplement is my key to restoring proper glutamate and oxalate metabolism, and can help you sleep if you have glutamate or oxalate issues. 🙂 #thingsIlearnedthehardway
Adrenal Issues and Sleep
In a normal person with healthy cortisol production, we see a big surge of cortisol in the morning, followed by a slow and steady decline until bedtime, when cortisol is super low, allowing us to feel tired so that we can fall asleep.
However, in the case of adrenal dysfunction, we see two different issues that can be associated with sleep disruption.
The first presents as an excess of cortisol all day long, including in the evening, when a person is supposed to have low amounts of cortisol and fall asleep. This person can feel anxious, irritable, and wired (but tired) during the day. They will be ready to get to work in the mornings, be agitated or hypervigilant, and be startled or experience sensations of shock, upon sudden nocturnal awakenings.
For this particular profile, I was initially trained to recommend phosphorylated serine, especially at bedtime, to help reduce cortisol and thus help promote sleep. Seriphos is a phosphorylated serine blend that may help to lower cortisol levels that are elevated due to stress. A dose of 1 capsule, 4 to 6 hours before an elevation in cortisol (maximum 3 capsules/day), is used for a short period (no longer than 7 days), to reset the sleep cycle.
However, in testing hundreds of people with Hashimoto’s, I have found that very few of them actually have excess overall cortisol. Furthermore, those with fatigue during the day and then a second wind at bedtime, often feel worse overall when they take phosphorylated serine. This is because most people I have seen with Hashimoto’s who are already taking thyroid hormones, actually have low levels of cortisol overall, sometimes known as “adrenal burnout” in the morning, noon, afternoon, and at bedtime. [23] These individuals generally feel tired all day and do not present with insomnia… as long as they go to sleep at a decent time.
This is actually the profile for the majority of people I see. I think this is because thyroid hormones can promote the clearance of adrenal hormones.
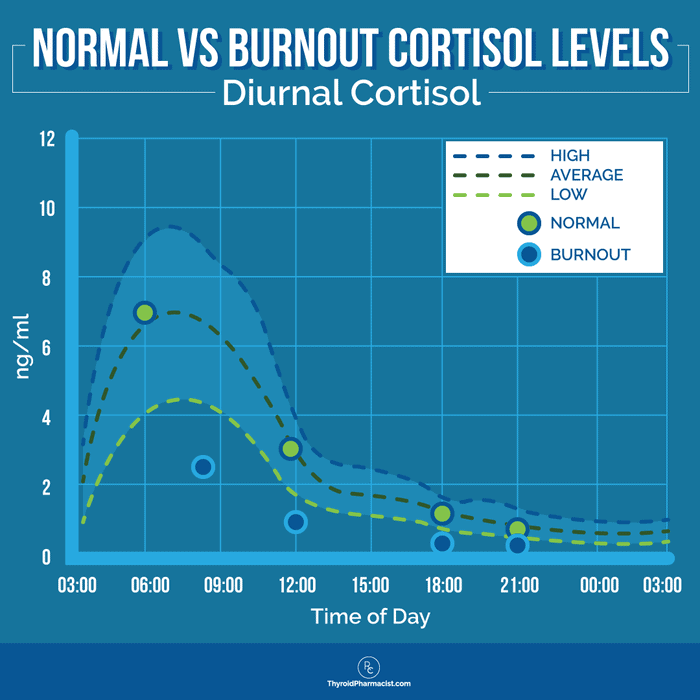
Additionally, a subset of individuals with Hashimoto’s may have overall low cortisol during the day, but will present with slight elevations at bedtime (especially if they end up staying up too late) — this is known as a flipped cortisol curve. This person’s typical profile is tired all day with difficulty in getting going in the morning, followed by a second wind in the evening, and trouble falling asleep. #beentheredonethat
For this person, the phosphorylated serine taken at bedtime can actually make adrenal issues far worse and lead to depression and more fatigue, due to it further breaking down the very little cortisol they have (I’ve been there, done that as well).
The approach I like to use in this situation is to incorporate blood sugar balancing techniques with adrenal adaptogens in the day, to support a healthy release of cortisol. When more cortisol is released during the day, the body often forgoes that second wind of cortisol in the evening, and the person can sleep better at night. You can learn more about using adaptogens as well as techniques to balance blood sugar in my book, Adrenal Transformation Protocol.
I like to recommend Rootcology Adrenal Support. It contains a curated blend of adaptogens and nutrients which can help maintain normal cortisol levels, promote healthy function of the hypothalamic-pituitary-adrenal (HPA) axis, and support normal production of neurotransmitters (dopamine, norepinephrine, and epinephrine), which help the brain with regulating sleep. [24] It also contains small amounts of B vitamins (B6 and folate are especially important for producing neurotransmitters) which assist in maintaining balanced cortisol output, and supporting the body’s natural cortisol rhythm throughout the day and at night. Furthermore, it contains vitamin C, which supports adrenal function, especially during stressful times when cortisol levels are high.*
Vitamin C can also be taken separately. I recommend a dose of 500 to 2000 mg, taken daily and/or during times of high stress.
As I mentioned earlier, by using lifestyle recommendations, adrenal support, and magnesium in my early days of working with people with Hashimoto’s, I had about a 50 percent success rate in helping people overcome sleep disorders. However, there were some people who continued to struggle with sleep, despite their excellent adherence to these protocols. We would see some things improve (like cramping, mood, and headaches), but the sleep issues would remain, and I realized that further strategies were needed.
Addressing 80 Percent of Sleep Issues
In 2020, I developed my Adrenal Transformation Program, and was thrilled when the results of clients who went through the program showed that 81 percent were able to resolve their sleep issues!
I developed this program, and the corresponding book, Adrenal Transformation Protocol, after further study of my clients that had issues with sleeping. I found that they usually had other symptoms that would co-occur with their sleep issues, such as brain fog, sore throat, hoarse voice, digestive issues, persistent blood sugar swings, and hormonal issues, that weren’t always resolved with my Root Cause approach of dietary changes, adrenal support, and magnesium.
Before I became the Thyroid Pharmacist, my parents and hubby would joke that I should have been a professional analyst, because of how I love to analyze things and find patterns. I love to look at common patterns I see in my clients, to come up with researched-based methods that can alter the patterns.
My love for finding patterns led me to these common conclusions in those who experienced insomnia:
- Blood sugar swings can wake people up in the middle of the night. This can be due to excess carbohydrate consumption, inadequate fat and/or protein intake, and nutrient deficiencies.
- Dehydration can cause leg cramps, as well as dry mouth and passages, which can lead to sleeping with one’s mouth open. This in turn can result in a hoarse voice, snoring, and sore throat, as well as waking up thirsty. Sleeping with the mouth open can also lead to sleep apnea, asthma, dental problems, elevated stress, high blood pressure, heart problems, and insomnia.
- Lack of hormones, such as progesterone, tends to be more common in Hashimoto’s, and this can also lead to sleep deprivation (hello perimenopause and menopause).
- Gut dysbiosis can lead to a buildup of ammonia, which has been tied to brain fog and frequent night wakings.
Dietary Interventions
Blood sugar swings and lack of protein may contribute to fluctuating energy levels throughout the day, difficulties with falling asleep, and frequent night wakings.
1. Balance blood sugar. Blood sugar imbalances can put us on an emotional rollercoaster. After consuming carbohydrate-rich foods, some people find their blood sugar goes up too high, too quickly. This leads to a rapid, sometimes excessive, release of insulin (a hormone that regulates blood sugar levels). These insulin surges can cause low blood sugar, which can cause unpleasant symptoms such as anxiety, nervousness, lightheadedness, fatigue, excessive hunger, and irritability (or feeling “hangry,” as I like to call it), and can also affect sleep patterns at night. We can often wake at night if blood sugar levels drop too low, which can be a sign that blood sugar is dysregulated throughout the day as well. If this sounds like you, I recommend reducing your intake of carbohydrate-rich foods, ensuring you are consuming adequate protein and fats, and experimenting with taking chromium or biotin at bedtime. Read on to learn more about supplements that can help balance blood sugar. My book, Adrenal Transformation Protocol, features a food plan and recipes specifically designed to help you balance blood sugar, as this is a key feature of adrenal dysfunction.
2. Consume more healthy fats. Fat is a long-burning fuel for your mind and body. I used to wake up drenched in sweat due to blood sugar swings at night… until I limited my carbs and tried adding healthy fats to my diet. Animal fats and coconut oil are great choices.
3. Get adequate amounts of protein (amino acids). Our bodies use amino acids from protein, for muscle repair and immune function. Muscle repair happens at night during deep sleep, so we want to make sure our body has all the raw materials it needs at night to heal and grow new tissue.
Many people with Hashimoto’s may need additional protein to meet their needs, and some individuals may not break down the protein properly due to low levels of stomach acid. Low stomach acid can lead to poor protein digestion, and can leave you with a heavy feeling during the night. Undigested protein also raises levels of orexin, an alertness chemical in the brain, which can disrupt your sleep. [25]
Here’s how to make sure you are getting enough protein:
- Calculate protein intake. For general health purposes, you should be consuming about 0.45 to 0.55 grams of protein per day, for each pound that you weigh. (The official calculation is done by kilograms of body weight: 1.0 to 1.2 grams of protein per kilogram.) This translates to roughly 50 grams of protein per day, for a person who weighs 100 pounds. Higher protein intake (0.55 to 0.68 grams per pound of body weight, per day) is recommended for most older adults who have acute or chronic diseases. (The official calculation is done by kilograms of body weight: 1.2 to 1.5 grams of protein per kilogram.) In this case, a person who weighs 100 pounds should aim for 54 to 68 grams of protein per day. Generally, the more active you are, the more protein you need. Bodybuilders need even more protein — as much as 1 gram of protein per pound of body weight — so a 100-pound person would want to aim for 100 grams of protein each day!
- Supplement with protein. Adding in a high-quality protein powder can help ensure adequate protein intake in an easily digestible form. I recommend Rootcology’s protein powders.
Supportive Supplements
In addition to focusing on blood sugar balance and adding adequate protein in my Adrenal Transformation Program, I also focus on six supportive supplements. I’ve already addressed the importance of Adrenal Support and magnesium above.
The four other supplements that I recommend as part of my Adrenal Support Kit are:*
- Carnitine Blend: This provides blood sugar balance support and reduces ammonia levels.
- S. Boulardii: This balances the gut microbiome and reduces ammonia levels.
- Myo-Inositol: This increases sex hormone binding globulin (SHBG) and progesterone levels, as well as improves insulin sensitivity, leading to more progesterone and fewer blood sugar swings.
- Electrolyte Blend: This blend supports hydration and balances our electrolyte levels, as well as provides a foundation for nutrients to be absorbed in the body.
Some 80 percent of people with sleep issues who have taken my Adrenal Transformation Program course have found these strategies effective in resolving sleep issues and feeling more rested, clear, and energized!
Strategies to Address the Other 20 Percent of Sleep Issues
If you have tried the above strategies, but are still struggling to get good sleep, there are further strategies that I recommend. About 20 percent of the people who go through my Adrenal Transformation Program, will need to dive a little deeper and explore one or more of the strategies listed below.
I often get frustrated with the basic recommendations on the web and in popular books, that only address really basic concerns and help no one. At the same time, I know it’s not possible for everyone to spend the time and money to see a functional medicine practitioner and do a gazillion different tests. I consider it a personal challenge to help individuals “personalize” health information to their own needs. In order to personalize health information for your very unique body, here are some targeted lab tests and symptoms to consider, to determine your best solution.
Addressing Nutrient Deficiencies to Improve Sleep Quality
Oftentimes, nutrient deficiencies are at the root of our inability to achieve quality sleep. As such, testing for and supplementing with the right nutrients, can make a big difference.
The most common nutrient deficiencies I see in Hashimoto’s that affect sleep include:
- Ferritin – In some cases, low iron/ferritin levels can cause insomnia, as well as restless leg syndrome (which can contribute to difficulty falling asleep), in those who have iron-deficient anemia. [26] Common symptoms of ferritin deficiency include fatigue, dizziness, headaches, weakness, ringing in your ears, irritability, leg pains, and shortness of breath. Low levels of ferritin can also be the cause of frequent night wakings. OptiFerin-C contains ferritin and has helped many of my clients boost their ferritin levels. Ester-C, a natural, water-soluble version of vitamin C, is added to increase its intestinal absorption. When I was pregnant, I found myself emotional, restless, and having trouble sleeping. In addition, I had MAJOR burger cravings! It turned out that I had a ferritin deficiency, and getting my ferritin levels normalized (using intravenous iron) helped me alleviate all of the above symptoms.
- Testing: Ferritin levels may be low, even if all other screening tests for iron and anemia come out within the reference range. You need to specifically test for ferritin. Ferritin level tests can be ordered by your doctor, or you can self-order one via Ulta Labs. The optimal ferritin level for thyroid function is between 90 and 110 ng/mL.
- Dose: 1 to 3 capsules per day, in divided doses, with meals
- B12 – B12 deficiency may result in gastrointestinal lesions and neurological damage, as well as symptoms such as depression, memory loss, weakness, personality and mood changes, and impaired cognitive performance. [27] Impaired digestion and inflammation are also symptoms of a B12 deficiency. When all of these other symptoms are happening, this can greatly affect our sleeping patterns. [28] I recommend Pure Encapsulations B12 5000, which comes in a convenient liquid form that can be administered sublingually for optimal absorption. The active form of B12 in this formulation is highly bioavailable and has been shown to support neurological function, healthy cognitive and nerve function, improved memory, and emotional well-being. Another good option is Pure Encapsulations Adenosyl/Hydroxy B12 Liquid, which combines adenosylcobalamin, an an activated form of B12 that is stored in the mitochondria, and hydroxycobalamin, another highly bioavailable form of B12.
- Testing: You can test your B12 (cobalamin) levels through your healthcare provider or through Ulta Labs. Optimal B12 levels should be between 700 and 900 pg/mL.
- Dose: 5000 mcg, sublingually, daily for 10 days; then 5000 mcg, once per week, for 4 weeks; then 5000 mcg monthly for maintenance
- Methylfolate – Low folate levels have been associated with sleep disturbances. Common symptoms of low folate include persistent fatigue, weakness, lethargy, pale skin, shortness of breath, and irritability. [29] Furthermore, if we don’t have enough folate on board, homocysteine may not convert to methionine, an important sulfur-containing amino acid that aids in building tissue and organs within the body. When we have this conversion happening, our circadian rhythm is improved.
- Testing: Folate levels can be tested via a serum test from Ulta Labs; the recommended range for adults is 2 to 20 μg/L.
- Dose: 1000-5000 mcg per day
- B6 – A B6 deficiency can be directly related to insomnia because B6 is required to make tryptophan, an essential amino acid that is used in the biosynthesis of proteins (and the reason you feel sleepy after eating a turkey dinner!). Common symptoms of a B6 deficiency include skin rashes, cracked lips, a sore tongue, mood changes, weakened immune function, fatigue, tingling in the hands and feet, and seizures. A zinc deficiency can also cause a B6 deficiency, since B6 needs zinc to be able to make tryptophan work for us within the body. [30] B6 is also needed for the creation of several important neurotransmitters, such as serotonin and gamma-aminobutyric acid (GABA). This deficiency was the root cause of my hubby’s sleep issues. He has a genetic SNP (gene variation) that leads him to produce less B6.
- Testing: The Organic Acids Test (OAT) from Mosaic Diagnostics tests for B6 levels; the reference range for pyridoxal phosphate (PLP), the biologically active form of vitamin B6, is 5 to 50 µg/L.
- Dose: I recommend using vitamin B6 in the P5P form (the pyridoxine form of B6 can build up in the body), taken at a dose of 50 to 200 mg/day. (Please note, do not use more than 300 mg/day of B6 in the pyridoxine form, as it has been associated with neuropathy.)
If you are deficient in several of the above nutrients, you may want to opt for a broad-spectrum vitamin and mineral supplement, such as Nutrient 950 by Pure Encapsulations, to cover all bases for optimal nutrition, which in turn can help improve your quality of sleep. Be sure to follow the package directions and your practitioner’s guidance to determine the right dosage for you.
Food Sensitivities
Food sensitivities can cause a whole host of issues, such as hives, fatigue, gastrointestinal issues, and even insomnia, especially if they’re caused by acid reflux, silent reflux, or GERD. Those with a hoarse voice and sore throat are especially likely to experience these. Histamine issues are also a frequent cause of food sensitivities for many people.
The most common food sensitivities I’ve seen in people with Hashimoto’s are gluten, dairy, soy, grains (corn, in particular), nightshades (potatoes, tomatoes, and peppers), nuts, and seeds. However, a person can become sensitive to just about any food. Identifying and eliminating problematic foods from your diet can relieve many of the symptoms associated with Hashimoto’s, including sleep issues.
Digestive Enzymes
If a person is already eating enough protein, but still struggles with fatigue, muscle loss, brittle hair nails, and poor immune function, I may recommend Rootcology Betaine with Pepsin as a first step. Many people with Hashimoto’s, in particular, have low levels of stomach acid, which can inhibit the breakdown of protein. This leads to poor digestion and absorption of the vital amino acids and other nutrients (such as B vitamins and iron), that our bodies need for energy and quality sleep. Supplementing with a digestive aid, such as Betaine with Pepsin, can make a big difference for many people with Hashimoto’s, as taking betaine and pepsin helps with the proper breakdown of food, the utilization of amino acids, and the lowering of ammonia production (which can be a by-product of poor digestion and dysbiosis).
Blood Sugar Balancing Supplements to Consider
- Chromium – If you are experiencing frequent night wakings and symptoms of blood sugar imbalances, you may be deficient in chromium. This mineral is involved in carb and fat metabolism, and also helps control blood sugar levels. A lack of chromium may make one more intolerant to carbohydrates, so it’s important to boost one’s intake of foods high in chromium, such as egg yolks, coffee, nuts, green beans, broccoli, and meat. Additionally, I recommend supplementing with ChromeMate GTF by Pure Encapsulations, at 600 mg per day.
- Biotin – Biotin helps with blood sugar balance, which, as mentioned earlier, is important for a good night’s sleep. Biotin also helps to boost our mood and assists with thyroid function. I recommend a dose of 1000 to 5000 mcg per day.
- I may recommend an amino acid supplement, such as Amino Support by Rootcology or Amino Replete (Pure Encapsulations), for people who have adequate protein and take enzymes, but still struggle with sleep. Amino acids serve as precursors to neurotransmitters and help with stabilizing blood sugar.
- L-glutamine – L-glutamine helps to support blood sugar, which may be at the root of your insomnia. I recommend taking 1000 to 1500 mg between meals.
Cortisol Level Testing
Seeing where your cortisol levels fall throughout the day, can give some insight as to why you may not be sleeping. Generally, we want our cortisol levels to be higher during the day, and gradually fall lower as we approach bedtime. Sometimes, a test can show the reverse, which can explain why we may feel groggy in the morning, tired but wired in the afternoon, and ready to party by evening.
If you’re still struggling with sleep issues after implementing the strategies mentioned above, you may need to do some further digging by testing your cortisol levels.
I recommend working with your practitioner to test cortisol levels throughout the day (it only takes a simple salivary or urine test at four intervals), and then developing a personalized plan for optimal support.
Digging Deeper into Specific Sleep Issues
For people who don’t get better with the above-mentioned protocols, I will go in a bit deeper and ask a LOT of questions. For specific issues, I may recommend the following interventions:
Sleep Issue: An inability to recall dreams.
- Protocol: Take vitamin B6 in the P5P form at 50 to 100 mg per day.
- B6 is critical for serotonin and GABA production, and a deficiency can also manifest as anxiety/irritability after consuming MSG, bone broth, and glutamine. Glycine and B6 are needed to convert glutamate, the neurotransmitter that makes us alert, to GABA, our sleep and chill neurotransmitter. [31]
Sleep Issue: Persistent brain fog, trouble staying asleep, and frequent night wakings.
- Protocol: These are symptoms that can be due to ammonia overload in the body (this can be tested with the Mosaic Diagnostics amino acid plasma test, but it won’t show up on one’s amino acid urine test). [32]
- As a starting point, I recommend taking Rootcology Carnitine Blend (up to 2000 mg per day), S. Boulardii (2 capsules, twice per day), and Magnesium Citrate Powder (½ to 1 teaspoon per day). All three help to remove ammonia from the body.
- For deeper ammonia removal, I recommend targeted amino acids that help with detoxification: NOW Foods Ornithine (500 to 2000 mg) or citrulline at bedtime. This clears out by-products of pathogenic bacteria (ammonia). (You may also want to focus on gut testing and gut healing protocols.) I generally also recommend taking activated B6 (P5P) (50 to 100 mg) and magnesium when taking amino acids like citrulline or ornithine, to ensure proper utilization. I suggest either Pure Encapsulations P5P or Rootcology P5P, as both are high-quality options.
Sleep Issue: Trouble falling asleep.
- Protocol: Supplementing with melatonin, our sleep-cycle hormone, can help you get back into your regular circadian rhythm routine, by providing either an immediate release of melatonin for bedtime-only insomnia, or melatonin in a delayed-release form to help with later-in-the-night awakenings.
- I recommend taking Herbatonin Melatonin at bedtime, at a dose between 0.5 and 5 mg, starting with the lowest dose, and increasing until you find a dose that works for you.
Sleep Issue: Traumatic brain injury.
- Protocol: Branched-chain amino acids (leucine, isoleucine, and valine) are critical for brain repair, and studies have shown that these three specific amino acids can also aid in relieving sleep disturbances in those with traumatic brain injuries. [33] As an added bonus, they can help with a clearer mind during daytime hours.
- Look for a high-quality supplement of branched-chain amino acids, such as BCCA. You will want to speak with a practitioner to see which amino acids are appropriate for you, and for proper dosing.
Sleep Issue: Perimenopause/menopause.
- Protocol: If you are experiencing insomnia and other symptoms of perimenopause or menopause, consider looking into hormone imbalances, and testing your progesterone levels. Low progesterone levels can be at the root of insomnia for some people, caused by hypothyroidism, stress, and a number of other conditions. Myo-inositol supplementation, magnesium supplementation, and blood sugar balancing can sometimes resolve low progesterone levels, but others may benefit from supplemental progesterone (or balancing estrogen). [34]
- You never want to use a progesterone cream/serum without first being tested for low progesterone levels, under the care of a medical professional. However, if you have had your hormone levels tested and know that you have low progesterone, a natural progesterone serum might help relieve many of your symptoms, including insomnia. I recommend trying a topical progesterone product like Wellena’s topical progesterone cream.
Sleep Issue: Can’t sleep after having too much caffeine. (I once took caffeine pills the day before an exam, during my freshman year in undergrad, so I could study… I was an anxious mess and could not sleep until 4 am! I don’t ever recommend caffeine pills for ANYONE, but if you happen to drink too much coffee, too late, one day, rest assured that there is a protocol for that!)
- Protocol: Gamma-aminobutyric acid (GABA) and 5-hydroxytryptophan (5-HTP) have been studied for their use in supporting caffeine-induced sleeplessness. [35]
- 5-HTP is a natural amino acid that is produced within our body and is a precursor to serotonin, the mood-boosting hormone. An added benefit is that serotonin can be converted to melatonin, our natural sleep cycle hormone. I recommend Pure Encapsulations 5-HTP.
- GABA is our naturally-occurring neurotransmitter that is known to produce calmness, as well as reduce tension and anxiety. I recommend Pure Encapsulations GABA.
Sleep Issue: Sleep issues connected to frequent night wakings, hormonal abnormalities, sugar cravings, imbalanced blood sugar levels, and PCOS.
- Protocol: You may benefit from using D-Chiro Inositol, alone or in combination with myo-inositol, or L-glutamine.
Sleep Issue: Symptoms such as frequent night wakings, hyperactivity, anger, rashes, bloating, abdominal pain, diarrhea, headaches, low blood pressure, hives, swelling and fatigue, may suggest histamine issues.
- Protocol: Histamine is an activating neurotransmitter and may make it difficult to sleep. You can test for histamine excess by ordering a whole blood histamine test. There are numerous protocols for addressing histamine; one I like to use that works quickly, involves supplementing with Rootcology P5P, zinc, and the essential amino acid methionine (which helps with breaking down histamine) at a dose of 500-3000 mg. (When using methionine, I also recommend magnesium, B6, folate, and B12.)
Sleep Issue: Trouble sleeping after an Epstein-Barr Virus (EBV) infection or reactivation, which can present with skin issues and poor appetite.
- Protocol: The amino acid lysine, which has been used to combat the herpes virus, maintains healthy arginine production, promotes healthy protein synthesis, and boosts immune function. I recommend a dose of 1000-3000 mg per day.
Sleep Issue: Frequent night waking, snoring, difficulty in waking up, restless sleep, nasal speech, mouth breathing, attention deficit disorder (especially in children), fatigue, and nasal congestion, may suggest sleep apnea.
- Protocol: Sleep apnea, a condition which is characterized by pauses in breathing while one is sleeping, is not uncommon in those with Hashimoto’s, and can cause us to feel unrested despite getting adequate sleep. I recommend speaking with your healthcare provider to get started with sleep apnea testing.
Sleep Issue: Insomnia presenting with fatigue, anxiety, emotional lability, racing thoughts, acne, hair turning orange or having a reddish tint, poor concentration, skin rashes, poor wound healing, frequent colds/flu, PMS symptoms, white spots on fingernails, craving high copper foods (like chocolate), and dark blotches on one’s face, especially during pregnancy, may be an indication of copper toxicity.
- Protocol: To clear excess copper from the body, I recommend avoiding high copper-containing foods and supplements, and increasing zinc levels, which works to displace copper in our body. I recommend 30 to 60 mg per day of Zinc 30 from Pure Encapsulations. Additionally, molybdenum is an amino acid chelate that clears out copper from the bloodstream and binds to copper in the intestines, so it can be excreted. I recommend Molybdenum from Douglas Laboratories, at 100 to 500 mcg per day. [36]
Sleep Issue: People who tend to struggle with worries, anxiety, obsessive thoughts, depression, low self-esteem, winter blues, panic attacks, fibromyalgia, or cravings for carbs or alcohol, may have a serotonin/melatonin deficiency.
- Protocol: There are two hormones recommended in this case:
- Tryptophan – This sleep hormone, at a dose of 500 to 2000 mg at bedtime, is the first treatment of choice.
- Melatonin – If tryptophan does not resolve the problem, consider taking melatonin in an immediate-release form for bedtime-only insomnia, or in a delayed-release form for later-in-the-night awakenings. Start with the lowest dose and increase slowly at bedtime. I recommend taking 0.5 to 5 mg (max dose).
Sleep Issue: Individuals that have trouble relaxing, experience panic attacks, have muscle tension, feel overwhelmed, and have had success with benzodiazepine medications, may have a deficiency in GABA.
- Protocol: Supplementing with amino acids can be beneficial in these cases:
- GABA – This is an amino acid that acts as brain neurotransmitters. It can promote a calming effect and can be taken with tryptophan/melatonin.
- L-theanine – This is a natural amino acid derived from green tea, which may provide a calming and relaxing effect.
Sleep issue: Sleep that does not seem restful, or when you know you won’t be getting enough sleep.
- Protocol: Taking a glycine supplement at bedtime can help with creating a more refreshing, deeper rest. A recent study found that glycine (a non-essential amino acid) subjectively and objectively improved sleep quality in people who suffered from insomnia. The effects of glycine on daytime sleepiness, fatigue, and performances in sleep-restricted healthy subjects, were evaluated during this study. Sleep was restricted to 25 percent less than the usual sleep time, for three consecutive nights. Before bedtime, 3 grams of glycine were ingested, and sleepiness and fatigue were evaluated using the visual analog scale (VAS) and a questionnaire. In subjects given glycine, the VAS data showed a significant reduction in fatigue and a tendency toward reduced sleepiness. These observations were confirmed with the questionnaire, indicating that glycine improves daytime sleepiness and fatigue induced by acute sleep restriction. [37] I recommend Designs for Health Glycine Powder at a dose of 3 grams per day, to make sleep more efficient; add in P5P if you find it makes you more anxious.
Suggestions for Sleep Deprived Parents
For those of us parents with little kids waking us up in the middle of the night, it can be frustrating to read suggestions for sleep issues when all the blue light blocking glasses and chamomile tea in the world, won’t stop that adorable little alarm clock from crawling into bed with you at 4 am.
In my case, I read all of the baby sleep books, had my son set up in his crib, and planned for him to sleep through the night by three months. If you want a summary, most of them suggest a routine, dark room, and white noise as an intro, plus one of the following three conclusions: [38]
- Wait until your baby is ready to sleep on their own, and never leave them to cry when they wake up at night.
- Leave your baby on their own to cry so they can learn to sleep on their own.
- Feed your baby a lot during the day so he/she doesn’t wake up at night and cry.
I have had friends succeed — and not succeed — using all of the above strategies. I think parents have to use their own intuition to see what is the best fit for their child, family, parenting style, and sanity.
The third option above was the most appealing to my parenting style, but of course my sweet son had his own ideas, and did not want to eat much during the day. (We actually had a lot of feeding challenges that are a topic for another day!) I ended up bringing him to bed with me when he turned eight months old, because I was too tired to do the four times nightly pilgrimage from my bed to his crib each night, and I felt like his cries meant he needed something. While some say that co-sleeping helps children sleep through faster, that was not the case for me. He continued to wake up, but I was at least not having to get out of bed each time he woke up.
Thankfully my Dimitry started sleeping through the night, shortly before he turned three, on a reliable basis. Most sleep training books claim that if a child falls asleep independently, he/she won’t wake up at night. I don’t know how true this is, as I was always pretty good at having a bedtime routine of bath → massage → PJs → nursing → reading → singing → kisses that allowed him to get progressively more relaxed, so he could fall asleep on his own. I would stay next to him on the bed, and co-slept, but he would still wake up.
Before I worked on his blood sugar levels, Dimitry would actually wake up very hungry at night, despite sleep training books claiming children over three months don’t need night feeds. I’m glad I never ignored his cries, although I sure wish I had figured this all out a long time ago!
The approach to get him to sleep all night was multifaceted, and included supporting blood sugar and addressing histamine levels, gut health, food intake, and hydration, in addition to reading gentle night weaning books. I felt like nutrition was a big piece of his sleep. You can thank him for this deep dive article, and my newfound deep appreciation for ammonia, amino acids, nutrigenomics, and blood sugar balancing protocols.
Furthermore, I am a believer in getting him outside for most of the day, and letting him sleep in a dark room. 🙂
Probably the most impactful thing for Dimitry’s sleep, however, was moving from living in the mountains, to living at sea level. He is now sleeping from 8:30 pm to 8 am most nights. Studies show that living at high altitudes can cause sleep issues (especially at elevations over 8000 ft), [39] and I recently came across a room oxygenator that may be able to help.
I don’t personally have any experience with this, but will consider trying it if we ever move back to our beloved Boulder, CO. 🙂
Lifestyle changes I tried that weren’t super helpful (but may help others), included a heating pad in his crib, a lovey, taking his pacifier away at six months (I would NEVER do this again if I have a second baby, lol), baby tea, baths, various swaddles, music devices, etc.
Integrative medicine suggestions I came across and tried for him, that were not relevant nor helpful for his sleep (but may be relevant for others), included homeopathy, supplementing with iron, addressing food sensitivities, using essential oils, taking fish oil, taking probiotics (except S. boulardii), craniosacral therapy, chiropractic therapy, taking magnesium, addressing tongue ties, and treating reflux. I came across some studies regarding butyrate produced by Bifidobacteria probiotics, as well as fish oil, helping children sleep better, but these didn’t seem to be relevant for him. [40]
I also came across another, lesser known method for getting children to sleep through the night, called “scheduled wakening,” where parents proactively wake up their babies a little later and later each night to feed them, so that their little bodies gradually adjust to going for longer stretches of sleep without eating. My son started refusing bottles around the age of two months, but if I have another baby that is willing to take bottles, I will consider this method.
While there are some variables we just can’t change, I have discovered some helpful interventions for maximizing the quality of sleep that we do get, and boosting our energy levels throughout the day. Always check with your doctor and watch your baby, but the following are generally considered to be safe for nursing moms: [41]
- Getting lots of bright light in the morning. If you can, try to get yourself and the baby outside, as soon as you wake up. Some parents love early morning stroller walks. I like having coffee on the patio. 🙂
- Grandparents — enough said!
- Thiamine: Thiamine is one of the B vitamins, known as B1. Its main responsibility is to change carbohydrates into energy, and it also helps with the digestion of proteins and fats. Thiamine is necessary for the proper release of hydrochloric acid in our stomachs, which is required for proper protein digestion. Most people with Hashimoto’s tend to have low stomach acid. Symptoms of milder forms of thiamine deficiency include fatigue, irritability, depression, and brain fog. Long-term thiamine deficiencies in those who consume any carbohydrates (even fruit), can lead to a buildup of pyruvic acid, which is a by-product of glucose metabolism, and can lead to mental fog. [42] I recommend benfotiamine at doses of 600 mg per day to increase energy and mental clarity — both Rootcology Benfotiamine and BenfoMax by Pure Encapsulations are high-quality supplement options.
- Fish Oil: Recent studies have found that omega-3 fatty acids, found in fish oil, may be beneficial for achieving a good night’s sleep. A diet deficient in omega-3 fatty acids has been shown to lower melatonin production and weaken the function of the circadian rhythm. [43] Fish oil, which is rich in omega-3s, can enhance the secretion of melatonin, which regulates sleep and wake cycles. I recommend Pure Encapsulations EPA/DHA Essentials at a dose of 1 to 3 grams per day (work up to your target dose).
- Choline: One of the lesser-known functions of acetylcholine is helping to maintain sleep. Acetylcholine controls the amount of sensory input that we take in around us. It works by strengthening the so-called stimulus barrier, making it possible to sleep through minor noises and other disturbances. As we age, we tend to become “light sleepers,” easily roused from sleep. As such, supplementing with choline may help us get better quality sleep. I recommend Vital Nutrients Citicoline at a daily dose of 500 to 2000 mg.
- Rhodiola: This adaptogen, sometimes referred to as Golden Root, not only helps us maintain a healthy stress response, but has also been found to improve depressive symptoms, insomnia, low mood, and mood instability.[44] It has a stimulatory effect on people in a state of fatigue. I think of rhodiola as the adaptogen focused on our nervous system health. In particular, I have found rhodiola to be helpful for my clients with depressed cortisol levels. One of the main chemicals in rhodiola is salidroside, found to have neuroprotective effects that reduce the impact of stress on the immune system and the neuro-endocrine system. Studies have found an anti-fatigue effect along with cognitive function improvements, such as improved memory (during stressful conditions), when people took rhodiola. I recommend Rhodiola Rosea by Pure Encapsulations.
- Tulsi Tea: As an adaptogen, preclinical studies have demonstrated that tulsi (or holy basil) provided anti-stress effects comparable to antidepressant drugs. [45] Some two dozen studies have found it has favorable clinical effects across multiple areas, including metabolic disorders, mood conditions, immunity, and infections. I love drinking tulsi tea to support my overall stress levels. This has become my go-to adaptogen during lactation, as it is also a galactagogue (which means it increases lactation) and can help raise cortisol levels when needed.
- Reishi and Lion’s Mane: These adaptogenic mushrooms have been studied for their ability to reduce stress levels, balance the adrenals, and combat fatigue.[46] Reishi is often promoted for its calming effects, while lion’s mane can help relieve brain fog and provide a mental boost. I like using Four Sigmatic‘s adaptogenic products — their Lion’s Mane Coffee is a great sleepy-parent pick-me-up, and I love their Reishi Elixir!
- Rasa Coffee Alternative: These yummy adaptogenic blends are packed with herbs that provide lasting energy, while nourishing the adrenals. They have a variety of options, including coffee blends, caffeine-free blends, and even an AIP-friendly version! Rasa was developed by a Boulder-based mom while she was sleep-deprived and breastfeeding her firstborn. (Use code IZABELLAWENTZPHARMD to get 15% off!)
The Takeaway
Sleep can be problematic for many people with Hashimoto’s, and there isn’t a one-size-fits-all approach when it comes to healing your circadian rhythm and achieving consistent, quality sleep.
I struggled with my own sleep for a long time before I realized that one key factor was my adrenal health. When I worked on healing my adrenals, this really helped me sleep better, which in turn dramatically improved my energy, focus, and productivity!
Participants in my Adrenal Transformation Program have seen amazing results as well. It’s a simple six-week program designed to help identify your adrenal triggers, balance your stress response, and gradually build up your resilience to prevent excess stress from overwhelming your adrenals. It has helped many reduce fatigue, improve mood and blood sugar balance, eliminate brain fog, improve energy levels, and more!
This can work wonders when it comes to reducing fatigue, improving mood and blood sugar balance, eliminating brain fog, improving energy, and more!
It’s important to gather data, experiment, and find what works best for you. My hope is that this article, as well as my books, offer you some clear and actionable solutions to get the rest you need, because sleep is so fundamental to good health.
Through lifestyle changes, dietary adjustments, addressing your adrenal health, and taking the supplements recommended above, you should see your sleep patterns shifting. You should soon be having an easier time falling and staying asleep, as well as feeling more refreshed and energetic throughout the day.
I hope you are able to use these hacks to improve your sleep cycle and accelerate your healing!
I love interacting with my readers on social media, and I encourage you to join my Facebook, Instagram, TikTok, and Pinterest community pages to stay on top of thyroid health updates and meet others who are following similar health journeys. For recipes, a FREE Thyroid Diet start guide, and notifications about upcoming events, be sure to sign up for my email list!
References
[1] Grandner MA, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: The evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14(3):191-203. doi:10.1016/j.smrv.2009.07.006; Yoshiike T, Utsumi T, Matsui K, et al. Mortality associated with nonrestorative short sleep or nonrestorative long time-in-bed in middle-aged and older adults. Sci Rep. 2022;12(1):189. Published 2022 Jan 7. doi:10.1038/s41598-021-03997-z
[2] Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Sci. 2015;8(3):143-152. doi:10.1016/j.slsci.2015.09.002; Wondisford FE. A direct role for thyroid hormone in development of the adrenal cortex. Endocrinology. 2015;156(6):1939-1940. doi:10.1210/en.2015-1351
[3] Rasch B, Born J. About sleep’s role in memory. Physiol Rev. 2013;93(2):681-766. doi:10.1152/physrev.00032.2012
[4] Morris CJ, Aeschbach D, Scheer FA. Circadian system, sleep and endocrinology. Mol Cell Endocrinol. 2012;349(1):91-104. doi:10.1016/j.mce.2011.09.003
[5] Kim W, Lee J, Ha J, Jo K, Lim DJ, Lee JM, Chang SA, Kang MI, Kim MH. Association between sleep duration and subclinical thyroid dysfunction based on nationally representative data. J Clin Med. 2019;8(11):2010. doi:10.3390/jcm8112010.
[6] Steiger A. Thyroid gland and sleep. Acta Med Austriaca. 1999;26(4):132-3.
[7] Magrini A, Pietroiusti A, Coppeta L, et al. Shift work and autoimmune thyroid disorders. Int J Immunopathol Pharmacol. 2006;19(4 Suppl):31-36; Leso V, Vetrani I, Sicignano A, Romano R, Iavicoli I. The Impact of Shift-Work and Night Shift-Work on Thyroid: A Systematic Review. Int J Environ Res Public Health. 2020;17(5):1527. Published 2020 Feb 27. doi:10.3390/ijerph17051527
[8] Green ME, Bernet V, Cheung J. Thyroid Dysfunction and Sleep Disorders. Front Endocrinol (Lausanne). 2021;12:725829. Published 2021 Aug 24. doi:10.3389/fendo.2021.725829
[9] Skene DJ, Lockley SW, Arendt J. Melatonin in circadian sleep disorders in the blind. Biol Signals Recept. 1999;8(1-2):90-95. doi:10.1159/000014575
[10] Komagata N, Latifi B, Rusterholz T, Bassetti CLA, Adamantidis A, Schmidt MH. Dynamic REM Sleep Modulation by Ambient Temperature and the Critical Role of the Melanin-Concentrating Hormone System. Current Biology. DOI:https://doi.org/10.1016/j.cub.2019.05.009. Published May 30, 2019. Accessed March 22, 2021; Harding EC, Franks NP, Wisden W. The Temperature Dependence of Sleep. Front Neurosci. 2019;13:336. Published 2019 Apr 24. doi:10.3389/fnins.2019.00336.
[11] Okamoto-Mizuno K, Mizuno K. Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol. 2012;31(1):14. Published 2012 May 31. doi:10.1186/1880-6805-31-14
[12] The Best Temperature for Sleep. Sleep Foundation. September 29, 2022. Accessed December 12, 2022. https://www.sleepfoundation.org/bedroom-environment/best-temperature-for-sleep
[13] Lee KB, Cho E, Kang YS. Changes in 5-hydroxytryptamine and cortisol plasma levels in menopausal women after inhalation of clary sage oil [published correction appears in Phytother Res. 2014 Dec;28(12):1897]. Phytother Res. 2014;28(11):1599-1605. doi:10.1002/ptr.5163; Zamanifar S, Bagheri-Saveh MI, Nezakati A, Mohammadi R, Seidi J. The Effect of Music Therapy and Aromatherapy with Chamomile-Lavender Essential Oil on the Anxiety of Clinical Nurses: A Randomized and Double-Blind Clinical Trial. J Med Life. 2020;13(1):87-93. doi:10.25122/jml-2019-0105; Takeda A, Watanuki E, Koyama S. Effects of Inhalation Aromatherapy on Symptoms of Sleep Disturbance in the Elderly with Dementia. Evid Based Complement Alternat Med. 2017;2017:1902807. doi:10.1155/2017/1902807; Chandharakool S, Koomhin P, Sinlapasorn J, et al. Effects of Tangerine Essential Oil on Brain Waves, Moods, and Sleep Onset Latency. Molecules. 2020;25(20):4865. Published 2020 Oct 21. doi:10.3390/molecules25204865; Lillehei AS, Halcón LL, Savik K, Reis R. Effect of Inhaled Lavender and Sleep Hygiene on Self-Reported Sleep Issues: A Randomized Controlled Trial. J Altern Complement Med. 2015;21(7):430-438. doi:10.1089/acm.2014.0327.
[14] So BCL, Kwok SC, Lee PH. Effect of Aquatic Exercise on Sleep Efficiency of Adults With Chronic Musculoskeletal Pain. J Phys Act Health. 2021;18(9):1037-1045. Published 2021 Jun 30. doi:10.1123/jpah.2020-0476
[15] Fitzgerald T, Vietri J. Residual Effects of Sleep Medications Are Commonly Reported and Associated with Impaired Patient-Reported Outcomes among Insomnia Patients in the United States. Sleep Disord. 2015;2015:607148. doi:10.1155/2015/607148
[16] Thakkar MM. Histamine in the regulation of wakefulness. Sleep Med Rev. 2011;15(1):65-74. doi:10.1016/j.smrv.2010.06.004
[17] Riza E, Linos A, Petralias A, de Martinis L, Duntas L, Linos D. The effect of Greek herbal tea consumption on thyroid cancer: a case control study. Eur J Public Health. 2015;25(6):1001-5. doi: 10.1093/eurpub/ckv063.
[18] Zomorodian K, Saharkhiz MJ, Shariati S, Pakshir K, Rahimi MJ, Khashei R. Chemical Composition and Antimicrobial Activities of Essential Oils from Nepeta cataria L. against Common Causes of Food-Borne Infections. ISRN Pharm. 2012;2012:591953. doi:10.5402/2012/591953
[19] Ngan A, Conduit R. A double-blind, placebo-controlled investigation of the effects of Passiflora incarnata (passionflower) herbal tea on subjective sleep quality. Phytother Res. 2011 Aug;25(8):1153-9. doi: 10.1002/ptr.3400. Epub 2011 Feb 3. PMID: 21294203.
[20] Cohen MM. Tulsi – Ocimum sanctum: A herb for all reasons. J Ayurveda Integr Med. 2014;5(4):251-259. doi:10.4103/0975-9476.146554
[21] Djokic G, Vojvodić P, Korcok D, et al. The Effects of Magnesium – Melatonin – Vit B Complex Supplementation in Treatment of Insomnia. Open Access Maced J Med Sci. 2019;7(18):3101-3105. Published 2019 Aug 30. doi:10.3889/oamjms.2019.771
[22] Wang K, Wei H, Zhang W, et al. Severely low serum magnesium is associated with increased risks of positive anti-thyroglobulin antibody and hypothyroidism: A cross-sectional study. Sci Rep. 2018;8(1):9904. Published 2018 Jul 2. doi:10.1038/s41598-018-28362-5
[23] Seck-Gassama, Ndoye O, Mbodj M, et al. Variations de la cortisolémie au cours des dysthyroidies [Serum cortisol level variations in thyroid diseases]. Dakar Med. 2000;45(1):30-33.
[24] Xia L, Chen GH, Li ZH, Jiang S, Shen J. Alterations in hypothalamus-pituitary-adrenal/thyroid axes and gonadotropin-releasing hormone in the patients with primary insomnia: a clinical research. PLoS One. 2013;8(8):e71065. doi: 10.1371/journal.pone.0071065.
[25] Inutsuka A, Yamanaka A. The physiological role of orexin/hypocretin neurons in the regulation of sleep/wakefulness and neuroendocrine functions. Front Endocrinol (Lausanne). 2013;4:18. Published 2013 Mar 6. doi:10.3389/fendo.2013.00018.
[26] Restless legs syndrome: detection and management in primary care. National Heart, Lung, and Blood Institute Working Group on Restless Legs Syndrome. Am Fam Physician. 2000 Jul 1;62(1):108-14. Erratum in: Am Fam Physician 2000 Aug 15;62(4):736; Schulte EC, Kaffe M, Schormair B, Winkelmann J. Iron in Restless Legs Syndrome. Mov Disord Clin Pract. 2014;1(3):161-172. Published 2014 Jun 12. doi:10.1002/mdc3.12047
[27] Okawa M, Mishima K, Nanami T, Shimizu T, Iijima S, Hishikawa Y, Takahashi K. Vitamin B12 treatment for sleep-wake rhythm disorders. Sleep. 1990 Feb;13(1):15-23. doi: 10.1093/sleep/13.1.15. PMID: 2305167.
[28] Beydoun MA, Gamaldo AA, Canas JA, et al. Serum nutritional biomarkers and their associations with sleep among US adults in recent national surveys. PLoS One. 2014;9(8):e103490. Published 2014 Aug 19. doi:10.1371/journal.pone.0103490
[29] Alpert, JE, and Fava, M. Nutrition and Depression: The Role of Folate. Medscape. January 1997. Accessed January 25, 2023. https://www.medscape.com/viewarticle/431514_2
[30] Kennedy DO. B Vitamins and the Brain: Mechanisms, Dose and Efficacy–A Review. Nutrients. 2016;8(2):68. Published 2016 Jan 27. doi:10.3390/nu8020068
[31] Folkers K, Shizukuishi S, Willis R, Scudder SL, Takemura K, Longenecker JB. The biochemistry of vitamin B6 is basic to the cause of the Chinese restaurant syndrome. Hoppe Seylers Z Physiol Chem. 1984 Mar;365(3):405-14. doi: 10.1515/bchm2.1984.365.1.405.
[32] Walker V. Severe hyperammonaemia in adults not explained by liver disease. Ann Clin Biochem. 2012;49(Pt 3):214-228. doi:10.1258/acb.2011.011206
[33] Lim MM, Elkind J, Xiong G, et al. Dietary therapy mitigates persistent wake deficits caused by mild traumatic brain injury. Sci Transl Med. 2013;5(215):215ra173. doi:10.1126/scitranslmed.3007092.
[34] Ciotta L, Stracquadanio M, Pagano I, Carbonaro A, Palumbo M, Gulino F. Effects of myo-inositol supplementation on oocyte’s quality in PCOS patients: a double blind trial. Eur Rev Med Pharmacol Sci. 2011 May;15(5):509-14. PMID: 21744744.
[35] Hong KB, Park Y, Suh HJ. Two combined amino acids promote sleep activity in caffeine-induced sleepless model systems. Nutr Res Pract. 2018;12(3):208-214. doi:10.4162/nrp.2018.12.3.208
[36] Greenblatt J. Integrative Approach to Treating Fatigue and Insomnia. The Great Plains Laboratory. https://vimeo.com/114923599. Accessed March 22, 2021.
[37] Bannai M, Kawai N, Ono K, Nakahara K, Murakami N. The effects of glycine on subjective daytime performance in partially sleep-restricted healthy volunteers. Front Neurol. 2012;3:61. Published 2012 Apr 18. doi:10.3389/fneur.2012.00061
[38] Korownyk C, Lindblad AJ. Infant sleep training: rest easy?. Can Fam Physician. 2018;64(1):41; Karraker KH, Young M. Night Waking in 6-Month-Old Infants and Maternal Depressive Symptoms. J Appl Dev Psychol. 2007;28(5-6):493-498. doi:10.1016/j.appdev.2007.06.002; Hiscock H, Wake M. Infant sleep problems and postnatal depression: a community-based study. Pediatrics. 2001;107(6):1317-1322. doi:10.1542/peds.107.6.1317
[39] Bian SZ, Zhang L, Jin J, et al. The onset of sleep disturbances and their associations with anxiety after acute high-altitude exposure at 3700 m. Transl Psychiatry. 2019;9(1):175. Published 2019 Jul 22. doi:10.1038/s41398-019-0510-x
[40] Szentirmai É, Millican NS, Massie AR, et al. Butyrate, a metabolite of intestinal bacteria, enhances sleep. Sci Rep. 2019:9(7035). https://doi.org/10.1038/s41598-019-43502-1.
[41] Jacobsen H. Mother Food: A Breastfeeding Diet Guide with Lactogenic Foods and Herbs – Build Milk Supply, Boost Immunity, Lift Depression, Detox, Lose Weight, Optimize a Baby’s IQ, and Reduce Colic and Allergies. Rosalind Press; 2004.
[42] Castiglioni C, Verrigni D, Okuma C, et al. Pyruvate dehydrogenase deficiency presenting as isolated paroxysmal exercise induced dystonia successfully reversed with thiamine supplementation. Case report and mini-review. Eur J Paediatr Neurol. 2015;19(5):497-503. doi:10.1016/j.ejpn.2015.04.008
[43] Patan MJ, Kennedy DO, Husberg C, et al. Differential Effects of DHA- and EPA-Rich Oils on Sleep in Healthy Young Adults: A Randomized Controlled Trial. Nutrients. 2021;13(1):248. Published 2021 Jan 16. doi:10.3390/nu13010248
[44] Ivanova Stojcheva E, Quintela JC. The Effectiveness of Rhodiola rosea L. Preparations in Alleviating Various Aspects of Life-Stress Symptoms and Stress-Induced Conditions-Encouraging Clinical Evidence. Molecules. 2022;27(12):3902. Published 2022 Jun 17. doi:10.3390/molecules27123902
[45] Jamshidi N, Cohen MM. The Clinical Efficacy and Safety of Tulsi in Humans: A Systematic Review of the Literature. Evid Based Complement Alternat Med. 2017;2017:9217567. doi:10.1155/2017/9217567
[46] Pazzi F, Adsuar JC, Domínguez-Muñoz FJ, García-Gordillo MA, Gusi N, Collado-Mateo D. Ganoderma lucidum Effects on Mood and Health-Related Quality of Life in Women with Fibromyalgia. Healthcare (Basel). 2020;8(4):520. Published 2020 Nov 30. doi:10.3390/healthcare8040520; Docherty S, Doughty FL, Smith EF. The Acute and Chronic Effects of Lion’s Mane Mushroom Supplementation on Cognitive Function, Stress and Mood in Young Adults: A Double-Blind, Parallel Groups, Pilot Study. Nutrients. 2023;15(22):4842. Published 2023 Nov 20. doi:10.3390/nu15224842
Note: Originally published in April 2021, this article has been revised and updated for accuracy and thoroughness.


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Greetings
I’m a 64 year older women who had a total thyroidectomy 6 years ago. One lymph node and had radioactive iodine treatment. There are still remaining cells that are regularly monitored and have not changed. I am 133lbs and take 112 mg of synthroid. I take nascobel. I take magnesium at night. I take c in the morning. I exercise daily. I was pre pre diabetic shortly after my surgery and was put on metformin but now just take 500 in the am. Have symmetrical leg sensations at night. Have been to neurologists and had a work up. Tried different remedies. No problem falling asleep but wake up 3-4 times a night. Cold and dark room. Not sure what pieces of your suggestions are for people with cancer issues. Would love to see a doctor who could help.
Nancy – thank you so much for sharing your journey. ❤️ I understand how hard this is to navigate. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target. We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are some articles you might find helpful
IMPORTANCE OF GUT HEALTH
https://thyroidpharmacist.com/articles/importance-gut-health/
THE MANY FACES OF HASHIMOTO’S
https://thyroidpharmacist.com/articles/the-many-faces-of-hashimotos/
10 FACTS ABOUT THYROID DISEASE
https://thyroidpharmacist.com/articles/need-know-thyroid-disease/
Isabella, You are so generous with advice.
I think I am currently experiencing copper detox (associated with postpartum), resulting in terrible insomnia. One of my issues is night chills. I feel chilled (nothing can warm me up). Ginger was helping, but it isn’t now. It is possible cold showers (think Wim Hof method) might help. Do you have any thoughts of what could help this?
Thanks,
Whitney
Whitney – thank you for following! ❤️ I’m so sorry you are struggling to get warm at night. I do offer a protocol to help clear excess copper in the article above. I also recommend discussing these symptoms with your practitioner as well.
Hi Isabella
I love your advice books and blogs, they help me massively, thank you. I’ve always slept well, 7 or 8 hours a nigh. I have Hashimoto’s and in October I got Covid & due to bad symptoms (and I suspect anxiety too), I didn’t sleep (2 hours each night), for 5 nights.
Now, 2.5 months later, I still have chronic insomnia and have been on sleeping tablets the entire time (sadly the only way I can get to sleep). My circadian rhythm is out of sync & I feel permanently wired and anxious due to my sleep issues. I always take a daily high dose magnesium supplement but should I also try melatonin? If so, what dose?
Thanks so much for your advice, I really appreciate it.
Jen
Jen – thank you for sharing! ❤️ I’m so sorry! Melatonin is an option and I have recommendations in the Sleep Solutions article above. Also, have you considered getting hormonal and adrenal testing done? I am wondering where your hormones are and where your cortisol levels are. You would want to discuss with a functional medicine doctor or naturopath that is proficient in reading these tests, but this may be a great way to see if it’s hormones or cortisol that is affecting your sleep. Have you tried balancing your blood sugar, creating a comfortable sleep environment, trying to have some protein before bed, and maybe upping your magnesium before bed? Here are a couple articles you might find helpful as well:
ARE YOUR ADRENALS SABOTAGING YOUR HEALTH?
https://thyroidpharmacist.com/articles/are-your-adrenals-sabotaging-your-health
NEW STUDIES ON MAGNESIUM AND THYROID HEALTH
https://thyroidpharmacist.com/articles/new-studies-on-magnesium-and-thyroid-health
I have Hashimotos. I sleep exactly 3 hours a night and wake up with an adrenaline rush. I am unable to concentrate and getting depressed. I am freezing with chills when I eat and my tongue is swollen. I have tried everything. All the supplements. CPAP. Sleeping pills. Nothing works. I force myself to walk outside for an hour a day. No wheat. No nightshades. No coffee. No alcohol. I beg my Drs to optimize my thyroid but as long as it is “in range” they do nothing. Last test TSH was 3.08. Antibodies are high. I am desperate.
Lisa – thank you for sharing. I’m so sorry you are struggling with all of this. Hashimoto’s is often a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better. Hashimoto’s is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission. You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto’s. Once you do, you will know what types of changes you need to implement to make yourself feel better.
If you need further support, please check out the list of lab tests inside the “Testing” chapter of my book, Hashimoto’s Root Cause. I also offer a 12-week program, Hashimoto’s Self Management Program. Here are some resources I hope you find helpful as well. ❤️
BUILDING YOUR OWN HEALTH TIMELINE
https://thyroidpharmacist.com/sample-health-timeline/
Hashimoto’s Self-Management Program
https://thyroidpharmacist.com/enroll-in-hashimotos-self-management/
ROOT CAUSE RESET
https://thyroidpharmacist.com/enroll-in-root-cause-reset/
Hi Lisa, I am curious to know how you are doing now? I am experiencing the same symptoms as you mentioned in this comment and am wondering what helped? I have also tried supplements and diet changes and am still only getting 3 hours of sleep and waking up “wired”
Kelsi – thank you for sharing. Some of the most common symptoms of adrenal dysfunction include chronic fatigue, a “tired but wired” feeling, trouble falling asleep, poor sleep, brain fog, difficulty concentrating, salt or sugar cravings, depression, anxiety, blood sugar issues, digestive difficulties, low libido, and weight gain or weight that’s difficult to lose. Here is an article that I hope is helpful: https://thyroidpharmacist.com/articles/are-your-adrenals-sabotaging-your-health/
Hi Isabella, Thank you! Was diagnosed with Hashimoto’s in 2021. I had a lot of stressful things that probably helped trigger this disease. I haven’t completed your Hashimoto’s Protocol book yet. My TPO is 134, and Thyroid test were normal. Ultrasound shows stable modules that are too small for biopsy, according to my doctor. I stopped gluten, dairy, soy, a year ago, and found some relief, but would sometime cheat with gluten and soy. I am strict now. I am vegan, but I am not opposed to eating meat, preferably fish if I started your program. I want to take action and get relief from the fatigue, brain fog and very dry skin that could be a also be a histamine sensitivity. My symptoms don’t happen every day, but enough to disrupt by life. My questions is should I continue with the solutions in the book or try your Self Management program or would one of your other programs be better for me. Are there any options for consults in the programs or a way to ask questions if I need help.
Lori – thank you for reaching out. You can certainly continue to follow my program in the book. As you said I do offer my Self Management program also, the difference between the book and the program is that it’s similar to owning a textbook versus actually being in a class with the teacher. I was limited as to the information I could put into a specific amount of pages in the book; not so in the programs! I also offer a liver program, an adrenal program and a gut program. Please email my team at info@thyroidpharmacist.com and they will be happy to share more information with you on all of these programs.
Thank you for all of this info, complete with links! I’m bookmarking it.
One question: I am actually on here looking for things to help my 4yo with constant wakings with nightmares (1-3 times a night) and I see all of the things you tried with your son and that didn’t do much good (most of them look familiar!), but I missed seeing what did help – do you know why he flipped a switch and started sleeping through the night? Also (second question I guess), do you know of any reason to not give a kid a small amount of ornithine to test? Asking for speculation of course, not medical advice!
Thanks much 🙂 You have helped me more than you will ever know over the last several years.
Loni – you’re welcome! I’m so glad you are finding my research helpful. The most helpful was moving from the mountains to sea level as I said in the article there were other things we did as well. As for ornithine, I recommend discussing this with your childs practitioner.
Dr. Wentz,
Which gene variation converts glycinate to glutamate? Very curious about this – thanks!
Heather
Heather – thank you for reaching out. GAD1 gene variation. Here is an article with more info: https://thyroidpharmacist.com/articles/new-studies-on-magnesium-and-thyroid-health/