One of the most discouraging symptoms I began experiencing before receiving my Hashimoto’s diagnosis was that I began losing my memory. In school, I always had a strong memory, and prided myself on my ability to recall obscure facts and details from experiences I’d had many years earlier.
Once my Hashimoto’s symptoms increased, however, my brain became “fuzzy”… and I frequently had a hard time remembering even common words mid-sentence (“You know, that animal with the fur? Yes, a cat!”).
It was a really scary feeling, and it got so bad that I took an assessment to rule out dementia. It was also exhausting trying to hide my embarrassing memory problems from the people in my life. Keep in mind, I was in my twenties when all this happened. I was supposed to be in my prime, but I felt old and tired.
It turns out, I was experiencing a common symptom of Hashimoto’s, known as brain fog.
In this article, I’d like to dive a little deeper into:
- What brain fog is
- How brain fog is related to Hashimoto’s
- The connection between the gut and brain health
- The root cause approach to addressing brain fog
What is Brain Fog?
The term “brain fog” is used to describe a collection of cognitive conditions, including memory problems, a lack of mental clarity, and an inability to focus. Sometimes described as mental fatigue or brain fatigue, brain fog itself is not a medical condition, but a symptom of another condition.
Researchers define brain fog as “a constellation of symptoms that include reduced cognition, inability to concentrate and multitask, as well as loss of short and long term memory.”
While everyone has moments of mental confusion, when they become more severe and frequent, they can become debilitating and make even simple daily tasks challenging.
Certain medical conditions that are associated with fatigue, inflammation, and blood sugar imbalances — such as hypothyroidism — often present with symptoms of brain fog. [1] Other medical conditions that commonly result in brain fog symptoms include fibromyalgia, diabetes, and multiple sclerosis.
Lifestyle factors that can result in brain fog include sleep deprivation, stress, diet, dehydration, and medication use. [2] Changes in hormones can also be a direct contributor to brain fog.
The Hashimoto’s and Brain Fog Connection
In my experience with working with Hashimoto’s patients, I have learned that brain fog is a common symptom for many people. There are four related factors that are the main drivers of brain fog for people with hypothyroidism: insufficient thyroid hormone, inflammation, blood sugar imbalances, and gut permeability.
Insufficient Thyroid Hormone
Research has shown that thyroid gland dysfunction (marked by changes in thyroid hormone concentration) can adversely impact cognitive functions, which helps to explain why so many people with Hashimoto’s are affected by symptoms of brain fog. [3]
Thyroid hormones (including T3 and T4) impact nearly every aspect of the brain, including neurogenesis (the production of neurons). A decrease in thyroid hormone, as is the case with Hashimoto’s, will naturally impact brain function. [4]
The standard of care for Hashimoto’s is to utilize a synthetic thyroid hormone replacement medication. Unfortunately, simply adding a synthetic thyroid medication to the mix will not result in full recovery for most Hashimoto’s patients. While this medication can be helpful for many people and their symptoms, it does not address the underlying root causes of the condition, and may also mask the underlying inflammation that can perpetuate the immune system imbalance and lead to other chronic conditions.
This is why many people continue to struggle with thyroid symptoms, including brain fog, even after they’ve started taking medication.
Inflammation
In Hashimoto’s, the thyroid gland is not just sluggish at putting out hormones; rather, the immune system has identified thyroid cells as foreign or harmful substances, and has developed antibodies to attack these cells. This attack leads to inflammation and damage of the cells that produce thyroid hormones.
The body then becomes stuck in a chronic state of immune system overload, adrenal hormone abnormalities, gut dysbiosis, impaired digestion, impaired detoxification, and thyroid hormone release abnormalities.
All of those conditions fuel inflammation, which not only impacts your thyroid, but also your brain. This cycle is self-sustaining and will continue to cause more symptoms… until an external factor intervenes and breaks the cycle.
Once inflammation kicks in, it can run rampant, creating oxidative stress (an overload of free radicals — unstable atoms that harm your body and brain). When chronic inflammation is present, oxidative stress is present much of the time, too.
Oxidative stress results from an imbalance in damaging free radicals and the body’s antioxidant defenses. Along with contributing to numerous health conditions, including cancer and dementia, oxidative stress can manifest in more acute situations, like brain fog, when your brain lacks the antioxidant defense. [5]
Inflammation and oxidative stress impact your brain in numerous ways beyond brain fog. For instance, inflammation triggers your brain to convert the amino acid tryptophan into anxiety-provoking chemicals rather than serotonin and melatonin. When you’re not making enough of these neurotransmitters, your mood and your sleep suffer.
Blood Sugar Imbalances
A third factor linking brain fog to Hashimoto’s is blood sugar imbalances, which are common in those with thyroid conditions. [6] When we consume large amounts of sugar — often in the form of high carbohydrate foods such as desserts, grains, and starchy vegetables — the pancreas has to release larger amounts of the hormone insulin to bring the levels of sugar in the blood back down to a normal level. These surges in insulin can cause blood sugar to drop too low, and lead to lowered levels of glucose (a simple sugar the body uses for fuel) in the brain. This reduces cognitive function by essentially “starving” the brain of its source of energy. [7]
Additionally, chronically high levels of insulin cause systemic and brain inflammation, leading to brain tissue damage and poor mental function. [8]
Gut Health
Many times, symptoms of Hashimoto’s thyroiditis, including brain fog, originate in your gut. That makes sense when you realize that every autoimmune condition is associated with intestinal permeability. [9]
More commonly called leaky gut, intestinal permeability occurs when the tight junctions within your gut that normally keep food particles confined, become loose. Food particles and toxins are able to escape the intestines and enter the bloodstream, creating an inflammatory reaction as these foreign invaders put your immune system into overdrive.
When your gut is inflamed, most likely your brain is, too.
Many factors contribute to leaky gut; however, one of the most common causes is food sensitivities. [10] The most common food sensitivities we see in people with Hashimoto’s are gluten and dairy, though a person can become sensitive to any food. Grains, soy and sugar are also major culprits.
What’s interesting is that gluten intolerance seems to affect systems and tissues predominantly outside of the gastrointestinal tract, and there is an emerging body of evidence that links gluten sensitivity to neurological and behavioral changes. [11] In fact, in my survey of 2232 readers with Hashimoto’s, 41 percent of them said that they experience brain fog after consuming gluten!
I have seen dramatic symptom improvement and remission over and over again in people with Hashimoto’s, who have eliminated triggers like gluten and healed their intestinal permeability.
Additionally, intestinal permeability may be caused by imbalances, infections and overgrowths in the gut, including overgrowth of the opportunistic yeast Candida albicans. When someone has a Candida overgrowth, a number of metabolic byproducts are produced in the gut, including uric acid, ammonia, and acetaldehyde. Acetaldehyde is particularly troublesome when it comes to brain fog, as it’s known to be a neurotoxin and potentially carcinogenic. [12] It’s the same toxin that’s responsible for symptoms of a hangover, so it’s no wonder you might be feeling foggy and tired if you have an overgrowth of Candida. Yeast overgrowth is very common with Hashimoto’s and contributes to many symptoms, including brain fog.
The microbes we have in our gut can produce either beneficial metabolites that can help us thrive, or problematic metabolites that cause us to struggle with our health.
Ammonia is a byproduct of bacterial metabolism of proteins, urea, and amino acids, and can build up if your digestion or microbiome is impaired, leading to symptoms such as brain fog, fatigue, muscle weakness, anxiety, and insomnia. [13]
Many of the potential causes of brain fog can, themselves, be caused by poor gut health, including stress, sleep quality, blood sugar imbalances, gluten intolerance, and insufficient thyroid hormone levels.
Addressing gut health and getting to the root cause of brain fog is oftentimes the best way to restore mental clarity.
The Gut and Brain Health Connection
There is such a strong connection between the brain and the gut, that some people refer to the gut as our “second brain.” We call this connection the brain-gut axis. [14] And, just like your gut maintains a protective barrier that prevents unwanted substances from crossing through, your brain has a blood-brain barrier. [15]
In fact, leaky gut goes hand-in-hand with leaky brain. These same particles that are not intended to slip through the gut, can make their way through the blood brain barrier. To compensate, your microglia (the brain’s “clean up crew” cells) hop into action.
As immune-supporting cells, microglia work to defend your central nervous system (CNS) by scavenging things like damaged cells, but also foreign invaders that slip through the blood-brain barrier. [16]
Microglia are extremely sensitive to potential CNS threats, and they wage an all-out assault at whatever they deem a potential problem. You want these cells to be alert, but calm, until a real threat occurs with your brain.
Typically, thyroid hormones step in and help keep those microglia calm. When you have low amounts of these thyroid hormones, however, they can’t always keep microglia in check, creating or exacerbating brain inflammation. The inflammatory response that is inherent with Hashimoto’s also contributes to this brain inflammation.
In other words, your brain suffers a double whammy: you don’t have enough thyroid hormones to keep those overzealous microglia in check, plus you have the inflammation present with Hashimoto’s, which spills over into other organs, including your brain.
Mitochondria and Brain Fog
Mitochondria are often referred to as the “powerhouse of the cell”, and for good reason – they are responsible for turning fatty acids from our diet into adenosine triphosphate (ATP), otherwise known as our body’s main source of energy! Mitochondria are also responsible for making adrenal hormones. [17]
When mitochondria are damaged, they don’t work as effectively. Adrenal hormone production can drop off significantly because of impaired or damaged mitochondria. There are many things that can potentially damage them, including inflammation, chronic stress, poor diet, nutrient deficiencies, and environmental toxins.
I think of the mitochondria as enigmatic little creatures that are delicate, yet oh so powerful. They need the optimal circumstances to do their powerful work of producing adrenal hormones and ATP, our main energy molecule. Because the body is a system, damaged mitochondria can impact our energy levels and induce feelings of brain fog. [18]
When we support mitochondria through a nutrient-dense diet, targeted supplementation (like carnitine, B vitamins, and vitamin C), and reducing inflammation, we can send safety signals clearing the way for healthy energy levels and reduced brain fog.
Hydration is also very important to support brain health and energy function, and electrolytes in particular are integral for supporting mitochondrial function. [19] Make sure you’re getting adequate electrolytes daily to support your brain and energy levels. A supplement like Rootcology’s Electrolyte Blend can be helpful, as it contains electrolytes as well as a high dose of vitamin C and D-ribose, two additional key nutrients that help with mitochondrial function.
Addressing the Root Cause of Brain Fog
To get to the root cause of brain fog in Hashimoto’s, we must start with the basics. Optimizing thyroid hormones should be the first item to check off in addressing brain fog for most people with Hashimoto’s. Next, since so many of the causes of brain fog (and Hashimoto’s itself) are rooted in poor gut health, we must eliminate food intolerances that may lead to intestinal permeability, support proper digestion of the food we eat, and address nutrient deficiencies that may be contributing to symptoms of brain fog.
The Fundamental Checklist
1. Optimize TSH Levels
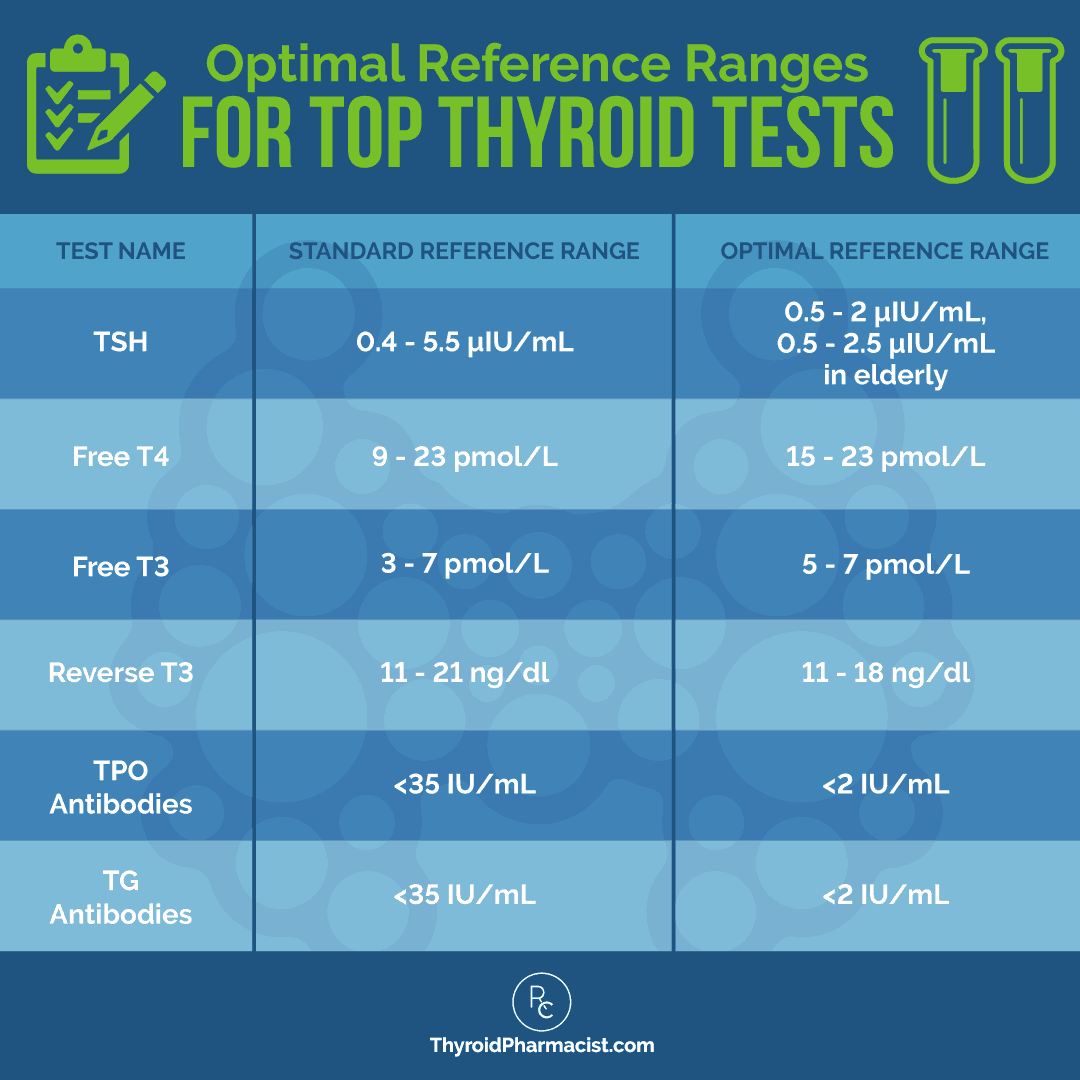
TSH (Thyroid Stimulating Hormone) is a pituitary hormone that responds to low/high amounts of circulating thyroid hormone. While the standard reference range for TSH is 0.2-8.0 μIU/mL, a new normal reference range was defined by the American College of Clinical Endocrinologists to be between 0.3-3.0 μIU/mL. Functional medicine practitioners have defined that normal reference ranges should be between 1 and 2 μIU/mL, for a healthy person not taking thyroid medications. Anecdotally, most patients feel best with a TSH between 0.5-2.0 μIU/mL.
If your TSH test shows a TSH level above 2.0 μIU/mL, even when all other thyroid tests fall within normal ranges, this is considered subclinical hypothyroidism. This means your thyroid is losing its ability to make enough thyroid hormone. At this point, you may benefit from starting on a thyroid medication (or increasing your current dose). For many, getting your TSH levels within optimal ranges will relieve many of the common hypothyroid symptoms, including brain fog.
2. Optimize T3
Some people may not properly convert T4 to T3 (the active thyroid hormone). There are many factors that may contribute to a person not being able to properly convert thyroid hormone, including liver congestion, stress, low zinc levels, and other nutrient deficiencies… which are all common in those with Hashimoto’s! [20] This is why many people continue to struggle with thyroid symptoms such as hair loss, brain fog, weight gain, depression, and fatigue, even after they’ve started taking thyroid medication.
Studies have suggested that T4-only therapy might not be enough to address the symptoms of hypothyroid patients, especially those related to mental well-being, such as brain fog and depression; and people who continue to have thyroid symptoms despite having normal TSH levels may benefit from a trial of T3, in addition to T4 medication. [21]
If this sounds like something you may benefit from, you do have a few options when it comes to T3-containing medications:
- T3 medications: These contain liothyronine and include the brand names Cytomel and Armour. They offer the active, albeit short-acting, T3 thyroid hormone. These medications are generally not recommended to be used as a sole therapy for hypothyroidism, as their short half-life may put a person on a thyroid hormone roller coaster. However, they can be used as an add-on to T4-only medications.
- NDT: One T4/T3 medication option is Natural Desiccated Thyroid (NDT, sometimes called desiccated thyroid extract, or DTE) hormones. These medications are derived from the thyroid glands of pigs, and are considered bio-identical to the hormones produced by our thyroid glands. Many patients who did not feel well on conventional treatments have reported feeling much better after switching to a NDT medication like Armour. When surveying my readers, I discovered that 59 percent did feel better after switching to Armour, 57 percent felt better on Nature-Throid, and 32 percent reported improvement with WP Thyroid(please note that Nature-Throid and WP Thyroid are not available at the time of publication of this article).
- Compounded medications: If NDT medications do not seem like a good fit for you, compounded T4/T3 products offer another alternative. Thyroid compounds are usually prepared in the same physiological ratio that is found in NDT products. However, physicians can elect to change the amount of T3 and T4, as compounding pharmacists must make the medications from scratch. This can be a huge advantage for patients who did not feel well on conventional treatments or natural desiccated thyroid treatments.
If you are unable to modify your thyroid medication, you may consider a supplement like Rootcology’s Thyroid Conversion Support, which provides a specialized blend of nutrients and herbs designed to promote healthy biosynthesis of thyroid hormone, including the conversion of T4 to T3.* You may also be interested in this podcast episode, where I discuss how to support the T4 to T3 conversion. (Note: This episode will be released on June 20th – the link may not work until then.)
I encourage you to read my article on which thyroid medication is best to help you find the combination that works best to optimize your thyroid hormones and reduce symptoms.
Whatever option you choose, be sure that your thyroid labs stay within the optimal reference ranges, and work with your practitioner to monitor them on an ongoing basis.
3. Eliminate Food Intolerances
I have found that most people with Hashimoto’s will need to give up gluten, dairy, and soy, as they are the primary food sensitivities affecting people with thyroid disorders. However, undergoing an elimination diet and food sensitivity testing will help you to pinpoint the foods that are problematic for you and lead to intestinal permeability.
4. Address the Adrenals
Healthy adrenal hormones tame inflammation (including inflammation in the brain), and the most important strategy for combating adrenal hormone dysfunction is stress reduction. In the early stages of adrenal fatigue, the adrenals secrete excessive levels of cortisol; in the later stages, they secrete less and less, leading to inadequate levels of the anti-inflammatory hormone in the body. [22] This can be a major contributing factor to brain fog.
Stress reduction, adequate sleep, and taking the ABC’s (adaptogenic herbs, B vitamins and vitamin C) are great starting points for addressing adrenal hormone imbalances. Rootcology Adrenal Support is a formulation of adaptogenic herbs and nutrients that is designed to support a healthy stress response and brain health, by helping to maintain normal cortisol levels, promoting healthy function of the hypothalamic-pituitary-adrenal (HPA) axis, and supporting normal neurotransmitter and hormone production.* Taking three capsules per day can help with brain fog due to adrenal issues.
My program Fatigue and Brain Fog Fix in Six: Thyroid & Adrenal Edition (formerly the Adrenal Transformation Program) has helped thousands of my clients and readers reverse their symptoms of brain fog. In fact, 92 percent of participants reported reduced brain fog after the program. It has been so successful in helping people reclaim their health that I decided to write a book about it! Adrenal Transformation Protocol is the book version of this program, outlining a simple 4-week program to help identify your adrenal triggers, balance your stress response, and gradually build up your resilience to prevent excess stress from overwhelming your adrenals.
For additional ideas on how to reduce stress and support your adrenals, please take a look at my article on adrenal health.
5. Support Digestive Enzymes
A lack of digestive enzymes and stomach acid are common in Hashimoto’s, and can allow undigested food particles to enter the bloodstream through a leaky gut. [23] This can often be the cause of food sensitivities and nutrient depletions, which can lead to brain fog (among other symptoms). I recommend using betaine with pepsin and digestive enzymes, to help your body break down the foods you consume, so that they can be readily utilized by your body and reduce damage to your gut.
Excess fatigue and brain fog were some of the most challenging symptoms I dealt with early in my Hashimoto’s journey. I was chronically exhausted, needed 12 hours of sleep every night, and had a hard time coming up with simple words at times.
After I started taking betaine with pepsin, I immediately began feeling more rested and energetic. I even became more outgoing and talkative, and felt like I had all the time and energy in the world. A few weeks later, I woke up one morning and started writing what would become my first book! It was then that I realized how much my lack of stomach acid and poor digestive function were contributing to my fatigue and mental state. My theory is that my body was focused on the backlog of undigested foods, instead of on creating luxuries like, you know, brain power and energy.
6. Address Nutrient Deficiencies
Nutrient deficiencies can occur as a result of eating nutrient-poor foods, having inflammation from infections or food sensitivities, taking certain medications, or having an imbalance of gut bacteria. A lack of sufficient thyroid hormones can also lead to nutrient deficiencies, as it makes nutrient extraction from food more difficult and less efficient.
The nutrient deficiencies that we see with Hashimoto’s that can lead to brain fog include:
- Iron: Ferritin is our iron storage protein. Low levels are commonly associated with Hashimoto’s and may lead to fatigue, difficulty breathing, hair loss, and poor cognitive function. [24] Ferritin levels should always be tested prior to supplementation, as iron can build up in the body and become toxic at elevated levels. Ferritin level tests can be ordered by your doctor, or you can self-order one via Ulta Lab Tests. Normal ferritin levels for women are between 12-150 ng/mL. According to some experts, ferritin levels of at least 40 ng/mL are required to stop hair loss, while levels of at least 70 ng/mL are needed for hair regrowth. The optimal ferritin level for thyroid function is between 90-110 ng/mL. I recommend OptiFerin-C by Pure Encapsulations at a dose of 1-3 capsules per day, in divided doses, taken with meals.
- Folate: Vitamin B9 is a necessary nutrient that naturally presents itself as folate, which plays a vital role in the formation of DNA and cell growth. However, a MTHFR gene variation that is common for many with Hashimoto’s, can impact how well your body metabolizes folate. [25] Both folate and folic acid are forms of vitamin B9, required for numerous critical bodily functions. However, folic acid is synthetic, while folate occurs naturally in foods, such as broccoli, lamb, beets, and quinoa. Some people have a MTHFR gene variation that prevents them from properly processing the folic acid that may be present in certain supplements and processed foods. Some professionals claim this type of folic acid may even cause a build-up in the body, leading to toxicity, of which brain fog is a symptom. Likewise, the MTHFR gene produces an enzyme necessary to process vitamin B9 properly. This enzyme is also important for converting homocysteine to methionine, which the body needs for proper muscle growth, energy, and mental function. I recommend supplementing with MTHFR Pathways, which contains the natural form of folate, at a dose of two capsules per day.
- Vitamin B12: Low levels of B12 are commonly associated with Hashimoto’s and may lead to fatigue, depression, neurological issues, impaired digestion, brain fog, tingling extremities, nerve damage, seizures, and anemia. [26] You can’t really overdose on B12, as it’s water-soluble, but I always recommend doing the initial test and retesting three months later to track and monitor your progress. You can test your B12 (cobalamin) levels through your healthcare provider or through Ulta Labs. Optimal B12 levels should be between 700-900 pg/mL. Please note: most labs will not flag low B12 levels unless they are under 200 pg/mL. I recommend supplementing with B12 5000 Liquid (methylcobalamin) by Pure Encapsulations, at a dose of 5000 mcg, sublingually, daily for 10 days; then 5000 mcg, once per week, for 4 weeks; then 5000 mcg monthly for maintenance. Be sure to use the sublingual version — swallowing B12 may result in inadequate absorption.
- Thiamine: Thiamine is one of the B vitamins, known as B1. Its main responsibility is to change carbohydrates into energy, and it also helps with the digestion of proteins and fats. [27] Thiamine is necessary for proper release of hydrochloric acid in our stomachs, which is required for proper protein digestion. Most people with Hashimoto’s have low stomach acid or do not release any stomach acid. [28] Symptoms of milder forms of thiamine deficiency include fatigue, irritability, depression, and brain fog. Long-term thiamine deficiencies in those who consume any carbohydrates (even fruit) can lead to a buildup of pyruvic acid, which is a by-product of glucose metabolism, and can lead to mental fog. I had one reader who wrote in to tell me that she was on disability, unable to work because of fatigue and brain fog. She began taking a thiamine supplement. After a few weeks, she was able to go back to work part-time, and eventually full-time, when her fatigue and brain fog lifted! I recommend Rootcology Benfotiamine or BenfoMax by Pure Encapsulations, taken in doses of 600 mg per day, to increase energy and mental clarity (especially for those who consume alcohol).
Tackling these steps will likely bring improvement — or even complete relief — of brain fog for many of you. As a reminder, please consult with your practitioner to determine which supplements and dosages are appropriate for you.
If you find that you are still experiencing symptoms, I recommend a few additional supplements that have been shown to support brain function.
7. Balance Your Microbiome
Gut infections and altered gut microbiomes that don’t have enough good bacteria to crowd out the pathogenic bacteria, can cause the bugs in our gut to produce toxic byproducts such as ammonia, which is produced by bacterial metabolism of proteins, urea, and amino acids. [29] Over time, ammonia can build up in our systems and contribute to brain fog.
H. pylori, a common gut infection in those with Hashimoto’s, is one of the infections that can cause excess ammonia to build up in the body. [30] Candida, a yeast overgrowth common in those with Hashimoto’s, can also contribute to high ammonia levels. [31]
I’ve found that the following nutrients can help clear excess ammonia from the gut and improve brain fog:
- L-carnitine: An overpopulation of opportunistic (bad) bacteria in the gut can lead to the production of ammonia. Studies have shown that taking L-carnitine can clear ammonia from the body. It does this by increasing the production of ATP, which is needed for the conversion of ammonia to urea, and by increasing production of N-acetylglutamine, which stimulates the urea cycle. [32]
- In a 2016 study, 60 hypothyroid patients who were experiencing fatigue, were given L-carnitine for 12 weeks. After 12 weeks, the researchers noted that the group receiving L-carnitine showed improvements in fatigue, with the most significant improvements seen in brain fatigue. [33] The most significant results were in those younger than 50, those over the age of 50 with high levels of free T3, and those who had hypothyroidism due to a thyroidectomy (who were taking relatively high doses of thyroid hormone). Researchers concluded that these populations were more active metabolically (and therefore had relative carnitine deficiency).
- This critical amino acid is concentrated in the body’s most metabolically active organs — the brain, heart, and muscles — and transports fatty acids into the mitochondria, where they’re burned for energy. It also helps in the production of acetylcholine, which is the neurotransmitter most associated with memory function. Studies have shown that acetyl-L-carnitine is helpful in slowing brain-related aging and decline. [34]
- I recommend taking one capsule per day of Rootcology’s Carnitine Blend, which contains the acetyl-L-carnitine form, for its unique properties in supporting brain function and reducing mental fatigue.
- S. boulardii: Another supplement that can help clear excess ammonia from the body is the yeast S. boulardii. It does this by promoting a healthy microbial balance in the gut and supporting the clearance of ammonia-producing microbes, including Candida and H. pylori. [35] It has the additional benefits of supporting a healthy gut lining and balancing levels of opportunistic yeast and bacteria in the gut, which can be root causes of leaky gut and brain fog.* Therapeutic doses of up to 8 capsules a day may be helpful, though I recommend slowly working up to that dose with 1-2 capsules per day.
- Magnesium Citrate: This form of magnesium promotes bowel movements and can be helpful for constipation. [36] Ensuring you’re having daily bowel movements can support the clearing of ammonia. Additionally, it’s believed that accumulation of ammonia in the brain is the result of increased manganese concentrations. Magnesium treatment has been shown to reduce blood levels of ammonia by increasing fecal manganese excretion, thereby decreasing manganese concentrations in the brain. [37]
- Probiotics: Additionally, taking a high quality probiotic supplement can help restore the balance of bacteria in the gut and help prevent leaky gut, which will help prevent the root causes of ammonia excess – infections and pathogenic bacteria.[38] ProB50 is a good option for broad spectrum, high-dose probiotic. I also like Ther-Biotic Complete by Klaire Labs (it’s available via Fullscript; if you don’t have a Fullscript account, you can sign up with my credentials here).
8. Support Your Mitochondria
In my book, Adrenal Transformation Protocol, I talk about a commonly missed root cause of brain fog – the health of our mitochondria. When our mitochondria are damaged, they don’t function properly, and this can lead to a host of different symptoms, including brain fog. [39] We utilize various ways to support our mitochondria throughout the protocol, including: replenishing with key nutrients to reduce oxidative stress and inflammation, providing the mitochondria with the nutrients they need to make energy, eating lots of healthy fats, and incorporating adaptogens.
There are two specific nutrients that I’d like to highlight, as I’ve found them to be superstars in supporting mitochondrial function. Carnitine has been a game-changer for many of my clients with fatigue – I’ve personally seen people awaken from a brain-foggy “sloth mode” with carnitine supplementation, and my own postpartum muscle weakness, aches, and pains were reversed with carnitine! Research backs up my observations and experience, finding supplementation with L-carnitine can indeed improve fatigue. [40] In one study, the most significant improvements were seen in “brain fatigue.”
Carnitine optimizes the body’s ability to burn fat for energy by transporting fatty acids into the mitochondria, where they can be burned and used. This can be so helpful for blood sugar. Carnitine also removes toxic brain fog-inducing by-products like ammonia from the gut, and promotes gut motility. All of this means more energy and less fatigue, less brain fog, less constipation, fewer digestive issues, and less muscle weakness and aches.
Even with a balanced, carnitine-rich diet, people with imbalanced adrenals or Hashimoto’s may find it difficult to retain and/or synthesize healthy levels of carnitine. This is why supplementation with carnitine can be so helpful. I recommend Rootcology’s Carnitine Blend, which combines L-carnitine and acetyl-L-carnitine, two active forms of carnitine. I recommend a dose of 1,000 mg of carnitine (ideally, a combination of the two active forms), twice per day.
I also find that supplementing with electrolytes and D-ribose can be helpful in supporting the mitochondria. D-ribose, a natural sugar, supports our hydration status and exercise recovery. Studies in athletes doing high-intensity training revealed significant improvements in performance, reduced muscle damage, and a lowered perceived exertion. [41] While I don’t recommend intense training with adrenal dysfunction, I do recommend D-ribose, as it can help with fatigue and exertion caused by day-to-day life tasks. (After all, running errands can feel like a major athletic endeavor for many with adrenal dysfunction!)
In addition to being wonderful for hydration, the D-ribose in Rootcology’s Electrolyte Blend also helps support ATP production. (If you are using an electrolyte blend that does not contain D-ribose, you can get a stand-alone D-ribose supplement.)
9. Consider Nootropic Supplements
You may have heard of the term “nootropics,” which refers to a broad range of drugs, supplements and other substances that are taken to improve cognitive performance. Sometimes referred to as “smart drugs” or “cognitive enhancers,” these substances can range from caffeine and adaptogens, to amphetamines. While the list of nootropics is long, there are few that I like that are science-backed for improving brain fog, and are safe for those of us with Hashimoto’s.
These include:
- Fish Oil: Essential fatty acids (EFAs) are naturally-occurring fats that the body cannot produce, and are therefore essential. They must be derived from either whole foods (like fish), or supplements. EFAs help manage inflammation and autoimmunity, promote blood vessel health, support healthy skin growth, provide the precursors to balance hormones, and support healthy brain and nervous system function. [42] They are considered essential because they are crucial to our health in so many ways. Omega-3 fatty acids, found in fish oil, provide powerful anti-inflammatory support for the brain. Supplementing regularly can improve cognitive performance, including memory, concentration, and learning abilities. [43] Look for a professional quality fish oil supplement that has been molecularly distilled and filtered, such as EPA/DHA Essentials by Pure Encapsulations or OmegAvail™ Synergy by Designs for Health. This process ensures purity and helps eliminate the chance of your supplement containing contaminants, including heavy metals, pesticides, solvents, and PCBs (polychlorinated biphenyls). I recommend 1-4 grams of fish oil per day, taken with a meal that contains quality fats.
- Trimethylglycine: Also known as TMG, trimethylglycine is a compound found in beetroot (and other plants and animal foods). It was originally known as betaine because it was first discovered in sugar beets. However, TMG is just one of many betaines that have since been identified. One of the main functions of TMG is to protect cells from stress, and it has many health benefits – it protects the liver, heart, and kidneys, and can enhance physical performance. [44] Studies have shown that participants who were given cobalamin supplementation (which increases TMG levels), experienced better reaction time, memory, and brain function. [45] A dose of 2.5 grams of trimethylglycine per day is recommended to reduce brain fog.
- L-Tyrosine: The amino acid tyrosine is a precursor of the thyroid hormone thyroxine and neurotransmitters, enhancing mood and cognitive function, especially under situations involving stress or when dopamine, epinephrine or norepinephrine levels require additional support. [46] I recommend taking 1-4 capsules per day, in divided doses.
- Choline: Choline is an essential nutrient that can be found in beef liver and egg yolks, but is deficient in many diets. Citicoline is a bioavailable version of choline that has been well studied to be less toxic and more effective than other versions. Numerous clinical studies have shown that citicoline boosts mental energy by improving cerebral blood flow and protecting brain cells from free radical damage. [47] In fact, its effects on the brain are so powerful that it’s used to enhance cognitive function in patients damaged by neurological disorders or brain trauma. Choline boosts acetylcholine levels, a neurotransmitter closely involved in learning and memory. It also contains CDP choline, an active component of phosphatidylcholine, which comprises 30 percent of brain tissue and preserves brain cell membranes, protects memory, and facilitates neural communication. One study investigated the effects of choline on memory disturbances and working memory, and found that citicoline can mitigate the effects of mental fatigue by increasing frontal lobe activity and brain energy reserves. [48] Additional studies have shown choline to improve cognitive speed and attention in young adults, stroke patients, and elderly individuals with dementia. [49] I recommend Vital Nutrients Citicoline. The usual daily therapeutic dosage of citicoline is 500-2,000 mg, taken daily.
- Glycine: If you find that your sleep is not restful, you might want to try taking a glycine supplement at bedtime for more refreshing, deeper rest. A recent study found that glycine (a non-essential amino acid) subjectively and objectively improved sleep quality in people who suffered from insomnia. [50] The effects of glycine on daytime sleepiness, fatigue, and performances in sleep-restricted healthy subjects were evaluated during this study. Sleep was restricted to 25 percent less than the usual sleep time for three consecutive nights. Before bedtime, 3 grams of glycine were ingested, and sleepiness and fatigue were evaluated using the visual analog scale (VAS) and a questionnaire. In subjects given glycine, the VAS data showed a significant reduction in fatigue and a tendency toward reduced sleepiness. These observations were confirmed with the questionnaire, indicating that glycine improves daytime sleepiness and fatigue induced by acute sleep restriction.
- L-theanine: You’ve probably heard about this amino acid for the mood-supporting properties it lends to green tea. It occurs naturally in black and green teas, and some mushrooms, but can also be taken as a supplement. It has been found to relieve stress and anxiety, without causing drowsiness. [51] When paired with caffeine, L-theanine may help increase focus and attention. One small study found that the combination of L-theanine and caffeine helped a group of young adults focus better on demanding tasks. [52] While a typical cup of coffee contains 95 mg of caffeine, and a cup of tea usually contains around 40 mg, the addition of L-theanine may make the tea more effective for boosting memory and concentration. L-theanine’s ability to increase focus, enhance relaxation, and even help with sleep make it a great tool for fighting brain fog.
- Methylene Blue: Initially developed as a dye for use in textile manufacturing, methylene blue has since been found to possess a number of health benefits, including helping with brain fog! It works on our mitochondria by increasing ATP production and reducing oxidative stress. It can help with mood and focus by boosting neurotransmitter production. Recently, I noticed biohackers using it for its nootropic effects, so I thought I’d give it a try! It turns out the hype is real – it has been incredible for increasing my focus and concentration. It may be another good option to help banish brain fog. In addition to the cognitive boost, I experienced the unexpected benefit of longer and stronger fingernails! Troscriptions makes high-quality methylene blue products, with several different varieties that each offer different benefits. I personally use their Just Blue product. I love Troscriptions because it’s physician-formulated and pharmaceutical-grade. They come as lozenges that are scored and easy to break, so you can take a precise dose. Please note, you can take it as a lozenge for the signature “blue tongue effect”, as well as swallow it whole. Please note, your urine will turn an interesting blue color. (You can use the code DRWENTZ for 10% off your order.)
Additional Steps to Relieve Brain Fog
If you are still experiencing brain fog after tackling the fundamental strategies I’ve outlined above, you may want to dig a little bit further and incorporate one or more additional steps to uncover your root causes.
- Try a ketogenic diet: Some people find that eating a high-fat, low-carb ketogenic diet — where the body breaks down fats for fuel instead of relying on carbohydrates — can help stabilize blood sugar and keep insulin levels low, while providing your brain an alternate fuel source that also lowers inflammation. [53] A well-designed ketogenic diet would include healthy high-fat foods, including wild-caught seafood, avocado, flax and chia seeds, and raw organic nuts. You also want to include plenty of gut-supporting foods, including fiber-rich leafy and cruciferous vegetables, as well as probiotic-rich foods like sauerkraut and kimchi.
- Eliminate mold toxicity: If your symptoms started around the time that you moved into your home, there’s a high potential that mold or toxic exposure may be the root cause of your condition. Potential symptoms can include brain fog, despite thyroid medications. You can read more about mold toxicity and how to protect yourself in my mold article.
- Look into EMF sensitivity: Another type of sensitivity that some people with Hashimoto’s can have is to electromagnetic fields (EMFs), such as those emitted by fluorescent lights, mobile phones, Wi-Fi, cordless phones, and power lines. Symptoms of EMF sensitivity include sleep disturbances, stress, fatigue, headaches, and brain fog, any and all of which may be exacerbated with increased exposure to EMFs. [54] You can take a look at the World Health Organization’s guidelines for safe levels of EMF exposure, but this is a topic that I’d like to explore more in an upcoming article!
- Eliminate mercury exposure: Mercury from dietary sources, including high-mercury fish like tuna and swordfish, can disrupt thyroid function. [55] This leads to numerous symptoms including brain fog. You can read more about uncovering, testing, and avoiding mercury exposure in my recent article.
Takeaway
Brain fog is an incredibly common symptom in Hashimoto’s and can leave a person feeling unable to function in their day-to-day life. Confusion, lack of focus, memory loss… these can all sap a person’s self-confidence and greatly impact their quality of life. I know this to be true, as it was my own experience!
The good news is that, by making sure our thyroid hormones are optimized, and by addressing gut health, we can eliminate most of the root causes of brain fog, and regain mental clarity. It might take some work; after all, healing from Hashimoto’s involves some detective work to get to the bottom of each individual’s root causes. But I have no doubt that you can get there. When brain fog is eliminated, there is no limit to what you can accomplish!
Have you experienced brain fog? What has helped you the most?
Wishing you all the best on your journey!
P.S. I love interacting with my readers on social media, and I encourage you to join my Facebook, Instagram, TikTok, and Pinterest community pages to stay on top of thyroid health updates and meet others who are following similar health journeys. For recipes, a FREE Thyroid Diet Quick Start Guide, and notifications about upcoming events, be sure to sign up for my email list!
References
[1] Ettleson MD, Raine A, Batistuzzo A, et al. Brain Fog in Hypothyroidism: Understanding the Patient’s Perspective. Endocr Pract. 2022;28(3):257-264. doi:10.1016/j.eprac.2021.12.003
[2] Kverno K. Brain Fog: A Bit of Clarity Regarding Etiology, Prognosis, and Treatment. J Psychosoc Nurs Ment Health Serv. 2021;59(11):9-13. doi:10.3928/02793695-20211013-01
[3] Ransing RS, Mishra KK, Sarkar D. Neuropsychiatric Manifestation of Hashimoto’s Encephalopathy in an Adolescent and Treatment. Indian Journal of Psychological Medicine. 2016 Jul-Aug;38(4):357-60.; Canelo-Ayba C, David Loja-Oropeza D, Cuadra-Urteaga J, Romani-Romani F. Hashimoto’s Encephalopathy Presenting with Neurocognitive Symptoms: A Case Report. Journal of Medical Case Reports. 2010;4:337.
[4] Bernal J. Thyroid Hormones in Brain Development and Function. In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext. South Dartmouth (MA): MDText.com, Inc.; January 14, 2022.
[5] Pizzino G, Irrera N, Cucinotta M, et al. Oxidative Stress: Harms and Benefits for Human Health. Oxid Med Cell Longev. 2017;2017:8416763. doi:10.1155/2017/8416763
[6] Gierach M, Gierach J, Skowrońska A, Rutkowska E, Spychalska M, Pujanek M, Junik R. Hashimoto’s Thyroiditis and Carbohydrate Metabolism Disorders in Patients Hospitalised in the Department of Endocrinology and Diabetology of Ludwik Rydygier Collegium Medicum in Bydgoszcz between 2001 and 2010. Endokrynologia Polska. 2012;63(1):14-7.
[7] Moheet A, Mangia S, Seaquist ER. Impact of diabetes on cognitive function and brain structure. Ann N Y Acad Sci. 2015;1353:60-71. doi:10.1111/nyas.12807
[8] Bahniwal M, Little JP, Klegeris A. High Glucose Enhances Neurotoxicity and Inflammatory Cytokine Secretion by Stimulated Human Astrocytes. Curr Alzheimer Res. 2017;14(7):731-741. doi:10.2174/1567205014666170117104053
[9] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
[10] Ventura MT, Polimeno L, Amoruso AC, et al. Intestinal permeability in patients with adverse reactions to food. Dig Liver Dis. 2006;38(10):732-736. doi:10.1016/j.dld.2006.06.012
[11] Jackson JR, Eaton WW, Cascella NG, Fasano A, Kelly DL. Neurologic and psychiatric manifestations of celiac disease and gluten sensitivity. Psychiatr Q. 2012;83(1):91-102. doi:10.1007/s11126-011-9186-y
[12] Gainza-Cirauqui ML, Nieminen MT, Novak Frazer L, Aguirre-Urizar JM, Moragues MD, Rautemaa R. Production of carcinogenic acetaldehyde by Candida albicans from patients with potentially malignant oral mucosal disorders. J Oral Pathol Med. 2013;42(3):243-249. doi:10.1111/j.1600-0714.2012.01203.x
[13] Auron A, Brophy PD. Hyperammonemia in review: pathophysiology, diagnosis, and treatment. Pediatr Nephrol. 2012;27(2):207-222. doi:10.1007/s00467-011-1838-5
[14] Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203-209.
[15] Banks WA. The Blood-Brain Barrier: Connecting the Gut and the Brain. Regulatory Peptides. 2008 Aug 7; 149(1-3): 11–14.
[16] Dissing-Olesen L, Ladeby R, Nielsen HH, Toft-Hansen H, Dalmau I, Finsen B. Axonal lesion-induced microglial proliferation and microglial cluster formation in the mouse. Neuroscience. 2007 Oct 12;149(1):112-22.
[17] Javadov S, Kozlov AV, Camara AKS. Mitochondria in Health and Diseases. Cells. 2020;9(5):1177. Published 2020 May 9. doi:10.3390/cells9051177
[18] Khacho M, Clark A, Svoboda DS, et al. Mitochondrial dysfunction underlies cognitive defects as a result of neural stem cell depletion and impaired neurogenesis. Hum Mol Genet. 2017;26(17):3327-3341. doi:10.1093/hmg/ddx217
[19] Adan A. Cognitive performance and dehydration. J Am Coll Nutr. 2012;31(2):71-78. doi:10.1080/07315724.2012.10720011; Parikh S, Saneto R, Falk MJ, et al. A modern approach to the treatment of mitochondrial disease. Curr Treat Options Neurol. 2009;11(6):414-430. doi:10.1007/s11940-009-0046-0
[20] Shimada T. Nihon Naibunpi Gakkai Zasshi. 1984;60(3):195-206. doi:10.1507/endocrine1927.60.3_195
[21] Ettleson MD, Bianco AC. Individualized Therapy for Hypothyroidism: Is T4 Enough for Everyone?. J Clin Endocrinol Metab. 2020;105(9):e3090-e3104. doi:10.1210/clinem/dgaa430
[22] Hahner S, Ross RJ, Arlt W, et al. Adrenal insufficiency. Nat Rev Dis Primers. 2021;7(1):19. Published 2021 Mar 11. doi:10.1038/s41572-021-00252-7
[23] Daher R, Yazbeck T, Jaoude JB, Abboud B. Consequences of dysthyroidism on the digestive tract and viscera. World J Gastroenterol. 2009;15(23):2834-2838. doi:10.3748/wjg.15.2834; Riccio P, Rossano R. Undigested Food and Gut Microbiota May Cooperate in the Pathogenesis of Neuroinflammatory Diseases: A Matter of Barriers and a Proposal on the Origin of Organ Specificity. Nutrients. 2019;11(11):2714. Published 2019 Nov 9. doi:10.3390/nu11112714
[24] R V, Dhiman P, Kollipaka R, P S, V H. Association of Hypothyroidism With Low Serum Ferritin Levels and Iron-Deficiency Anemia During the First Trimester of Pregnancy. Cureus. 2022;14(8):e28307. Published 2022 Aug 23. doi:10.7759/cureus.28307
[25] Yang R, Pu D, Tan R, Wu J. Association of methylenetetrahydrofolate reductase (MTHFR) gene polymorphisms (C677T and A1298C) with thyroid dysfunction: A meta-analysis and trial sequential analysis. Arch Endocrinol Metab. 2022;66(4):551-581. doi:10.20945/2359-3997000000471
[26] Jabbar A, Yawar A, Waseem S, et al. Vitamin B12 deficiency common in primary hypothyroidism [published correction appears in J Pak Med Assoc. 2009 Feb;59(2):126. Wasim, Sabeha [corrected to Waseem, Sabiha]]. J Pak Med Assoc. 2008;58(5):258-261.
[27] Frank LL. Thiamin in Clinical Practice. JPEN J Parenter Enteral Nutr. 2015;39(5):503-520. doi:10.1177/0148607114565245
[28] Ebert EC. The thyroid and the gut. J Clin Gastroenterol. 2010;44(6):402-406. doi:10.1097/MCG.0b013e3181d6bc3e
[29] Romero-Gómez M, Jover M, Galán JJ, Ruiz A. Gut ammonia production and its modulation. Metab Brain Dis. 2009;24(1):147-157. doi:10.1007/s11011-008-9124-3
[30] Chittajallu RS, Neithercut WD, Macdonald AM, McColl KE. Effect of increasing Helicobacter pylori ammonia production by urea infusion on plasma gastrin concentrations. Gut. 1991;32(1):21-24. doi:10.1136/gut.32.1.21
[31] Holmes AR, Collings A, Farnden KJ, Shepherd MG. Ammonium assimilation by Candida albicans and other yeasts: evidence for activity of glutamate synthase. J Gen Microbiol. 1989;135(6):1423-1430. doi:10.1099/00221287-135-6-1423
[32] Nojiri S, Fujiwara K, Matsuura K, et al. L-carnitine reduces ammonia levels and alleviates covert encephalopathy: A randomized trial. https://www.oatext.com/L-carnitine-reduces-ammonia-levels-and- alleviates-covert-encephalopathy-A-randomized-trial.php. Published March 2018. Accessed December 14, 2022.
[33] An JH, Kim YJ, Kim KJ, et al. L-carnitine supplementation for the management of fatigue in patients with hypothyroidism on levothyroxine treatment: a randomized, double-blind, placebo-controlled trial. Endocr J. 2016 Oct 29;63(10):885-895. Epub 2016 Jul 16.
[34] Pennisi M, Lanza G, Cantone M, et al. Acetyl-L-Carnitine in Dementia and Other Cognitive Disorders: A Critical Update. Nutrients. 2020;12(5):1389. Published 2020 May 12. doi:10.3390/nu12051389
[35] Terciolo C, Dapoigny M, Andre F. Beneficial effects of Saccharomyces boulardii CNCM I-745 on clinical disorders associated with intestinal barrier disruption. Clin Exp Gastroenterol. 2019;12:67-82. Published 2019 Feb 11. doi:10.2147/CEG.S181590
[36] Siegel JD, Di Palma JA. Medical treatment of constipation. Clin Colon Rectal Surg. 2005;18(2):76-80. doi:10.1055/s-2005-870887
[37] Li Y, Ji CX, Mei LH, Qiang JW, Ju S. Oral administration of trace element magnesium significantly improving the cognition and locomotion in hepatic encephalopathy rats. Sci Rep. 2017;7(1):1817. Published 2017 May 12. doi:10.1038/s41598-017-02101-8
[38] Shi LH, Balakrishnan K, Thiagarajah K, Mohd Ismail NI, Yin OS. Beneficial Properties of Probiotics. Trop Life Sci Res. 2016;27(2):73-90. doi:10.21315/tlsr2016.27.2.6
[39] Khacho M, Clark A, Svoboda DS, et al. Mitochondrial dysfunction underlies cognitive defects as a result of neural stem cell depletion and impaired neurogenesis. Hum Mol Genet. 2017;26(17):3327-3341. doi:10.1093/hmg/ddx217
[40] Malaguarnera M, Cammalleri L, Gargante MP, Vacante M, Colonna V, Motta M. L-Carnitine treatment reduces severity of physical and mental fatigue and increases cognitive functions in centenarians: a randomized and controlled clinical trial. Am J Clin Nutr. 2007;86(6):1738-1744. doi:10.1093/ajcn/86.5.1738
[41] Seifert JG, Brumet A, St Cyr JA. The influence of D-ribose ingestion and fitness level on performance and recovery. J Int Soc Sports Nutr. 2017;14:47. Published 2017 Dec 20. doi:10.1186/s12970-017-0205-8
[42] Di Pasquale MG. The essentials of essential fatty acids. J Diet Suppl. 2009;6(2):143-161. doi:10.1080/19390210902861841
[43] Bauer I, Hughes M, Rowsell R, et al. Omega-3 supplementation improves cognition and modifies brain activation in young adults. Hum Psychopharmacol. 2014;29(2):133-144. doi:10.1002/hup.2379
[44] Arumugam MK, Paal MC, Donohue TM Jr, Ganesan M, Osna NA, Kharbanda KK. Beneficial Effects of Betaine: A Comprehensive Review. Biology (Basel). 2021;10(6):456. Published 2021 May 22. doi:10.3390/biology10060456
[45] van Asselt DZ, Pasman JW, van Lier HJ, et al. Cobalamin supplementation improves cognitive and cerebral function in older, cobalamin-deficient persons. J Gerontol A Biol Sci Med Sci. 2001;56(12):M775-M779. doi:10.1093/gerona/56.12.m775; Eussen SJ, Ueland PM, Clarke R, Blom HJ, Hoefnagels WH, van Staveren WA, et al. The association of betaine, homocysteine and related metabolites with cognitive function in Dutch elderly people. Br J Nutr. 2007 Nov;98(5):960-8. Epub 2007 May 31.
[46] Steenbergen L, Sellaro R, Hommel B, Colzato LS. Tyrosine promotes cognitive flexibility: evidence from proactive vs. reactive control during task switching performance. Neuropsychologia. 2015;69:50-55. doi:10.1016/j.neuropsychologia.2015.01.022
[47] Silveri MM, et al. Citicoline enhances frontal lobe bioenergetics as measured by phosphorus magnetic resonance spectroscopy. NMR in Biomedicine. 24 Sep 2008. https://doi.org/10.1002/nbm.1281
[48] Bruce SE, Werner KB, Preston BF, Baker LM. Improvements in concentration, working memory and sustained attention following consumption of a natural citicoline-caffeine beverage. Int J Food Sci Nutr. 2014;65(8):1003-1007. doi:10.3109/09637486.2014.940286
[49] Jasielski P, Piędel F, Piwek M, Rocka A, Petit V, Rejdak K. Application of Citicoline in Neurological Disorders: A Systematic Review. Nutrients. 2020;12(10):3113. Published 2020 Oct 12. doi:10.3390/nu12103113
[50] Bannai M, Kawai N, Ono K, Nakahara K, Murakami N. The Effects of Glycine on Subjective Daytime Performance in Partially Sleep-Restricted Healthy Volunteers. Front Neurol. 2012; 3: 61. doi: 10.3389/fneur.2012.00061
[51] Nobre AC, Rao A, Owen GN. L-theanine, a natural constituent in tea, and its effect on mental state. Asia Pac J Clin Nutr. 2008;17 Suppl 1:167-168.
[52] Giesbrecht T, Rycroft JA, Rowson MJ, De Bruin EA. The combination of L-theanine and caffeine improves cognitive performance and increases subjective alertness. Nutr Neurosci. 2010;13(6):283-290. doi:10.1179/147683010X12611460764840
[53] Xu Y, Jiang C, Wu J, et al. Ketogenic diet ameliorates cognitive impairment and neuroinflammation in a mouse model of Alzheimer’s disease. CNS Neurosci Ther. 2022;28(4):580-592. doi:10.1111/cns.13779
[54] Stein Y, Udasin IG. Electromagnetic hypersensitivity (EHS, microwave syndrome) – Review of mechanisms. Environ Res. 2020;186:109445. doi:10.1016/j.envres.2020.109445
[55] Pamphlett R, Doble PA, Bishop DP. Mercury in the human thyroid gland: Potential implications for thyroid cancer, autoimmune thyroiditis, and hypothyroidism. PLoS One. 2021;16(2):e0246748. Published 2021 Feb 9. doi:10.1371/journal.pone.0246748
Please note: Originally published in November 2019, this article has been updated for accuracy and thoroughness.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
I know i need all of the above! As a single mom with only a pt job cuz i am too sick to work full time, i cant afford them. Are there free samples or trials or any way to get these? My insurance covers all my expensive drugs at 100%. But nothing to fix me. Just to control symptoms. Help
Angela – thank you so much for reaching out and sharing. I understand how hard this can all be. At this time we do not offer samples or trials. I suggest that you join one of the Hashimoto’s groups that are out there. Being able to share ideas of what has worked with one another and offer support for each other can be very helpful. A couple of years after my diagnosis, I found Hashimoto’s 411, a closed Facebook group run by Alice Berry McDonnell. This group is amazing! It is comprised of an army of highly motivated, smart, supportive women and men (now 45,000+ strong), and each of them sharing ideas of what worked for them, things they were planning to try, and offering support to one another. The comfort I received from knowing that there were others going through the same challenges as I, was enormous. Here is a link if you would like to check it out:
https://www.facebook.com/groups/hashimotos411/
I live in Scranton Pa. What chance do I have. Can’t even get thru to my primary Dr nif I don’t feel well. Then they tell me to go to thr midi center then they tell e to go to thr emergency room and they tell me I have vertigo.. I have no hope. I had breast implant over 40 years ago. They both ruptured had them removed still after all this time I still have all these symptonsv. Chronic fatigue brain fog etc.. Now I found out the capsules may still be intact an they cannot find my records So what chance do I have to ever have any quality of life. I am now 75 getting tired of the battle. No one cares about us oldsters. Things are cut back msorry just had to unload. What do I do now??
Mary – thank you so much for reaching out and sharing your journey. I am so sorry you have had to go through all of this. <3 My heart goes out to you. Hang in there! I recommend that you join one of the Hashimoto’s groups that are out there. Being able to share ideas of what has worked with one another and offer support for each other can be very helpful. A couple of years after my diagnosis, I found Hashimoto’s 411, a closed Facebook group run by Alice Berry McDonnell. This group is amazing! It is comprised of an army of highly motivated, smart, supportive women and men (now 45,000+ strong), and each of them sharing ideas of what worked for them, things they were planning to try, and offering support to one another. The comfort I received from knowing that there were others going through the same challenges as I, was enormous. Here is a link if you would like to check it out.
https://www.facebook.com/groups/hashimotos411/
I also highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
what if a person thyroid is at 89.0 so they they are now taking 250 mcg .synthroid
Michele – thank you for following this page. <3 Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication which you are looking for, ask your local pharmacist for doctors in your area who prescribe the medication you are looking to try. Have you read these articles?
WHICH THYROID MEDICATION IS BEST?
https://thyroidpharmacist.com/articles/which-thyroid-medication-is-best/
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
Hi, I need some help.
I was diagnosed with Hashimotos in 2015, but I wonder if that’s what I have. All my thyroid numbers are coming back normal except for TPO, which just came back at 90 IU/mL. I’ve been diagnosed with wheat and dairy sensitivity and have been off those foods completely for months prior to this lab work. Sugar has also been drastically reduced and I avoid most soy, just to be on the safe side, even though a sensitivity to these things was not detected. Antigliadin is negative. Also diagnosed with leaky gut. I have a candida infection that is slowly going away. My ADH and MSH are low. My MMP-9 is 614 ng/mL. VEGF is on the high side of normal. Hormone levels are all normal (testosterone on the low side of normal, but still in range). I’m on a natural anti-inflammatory and inflammation is completely non-existent in my bloodwork.
What should I do? I’ve been pretty sick for about 8 months–lots of abdominal pain and bloating. I lost 55 lbs–it just fell off me. I’ve seen so many doctors who don’t know how to help. Any advice you can offer would be much appreciated.
Heather – thank you so much for reaching out and sharing your journey. <3 I am so sorry to hear you are struggling with all of this. I know how overwhelming everything can be. Gut healing is a journey; you may need various interventions like removing reactive foods and infections, taking enzymes and probiotics, and balancing nutrients. Remember, be kind to yourself and learn to listen to your body so that you can support and feed it properly! You are worth it! You may find this article helpful as well!
WHAT'S CAUSING YOUR LEAKY GUT
https://thyroidpharmacist.com/articles/whats-causing-your-leaky-gut/
SUPPLEMENTS ACTUALLY HELP HASHIMOTO’S
https://thyroidpharmacist.com/articles/which-supplements-actually-help-hashimotos/
What is the difference between trimythylglycine and Betaine HCl? how much glycine would TMG be made available in the body? (I already take about 4 Tbsp. of collagen per day and I know that my glycine needs are high/obvious because when I started taking magnesium glycinate several years ago it was one of my miracles. If I stopped taking my 3 doses of mag glycinate, I would not be myself anymore–agitation, irritation and anger would go way up).
Rachel – thank you for reaching out. <3 TMG is similar chemically to betaine hydrochloride, but it has entirely different actions. I recommend discussing the addition of any supplements with your practitioner who familiar with your healthcare history.
Hello dr.Wentz, first of all thank you so much for all the information and tips! Recent blood test showed a raised anti TPO, i havent done a full thyroid panel yet, but i am experiencing so many symptoms and have been so sick and weak, that i suspect my thyroid to be the issue, as i experienced pain in that area over the last year and now it feels my throat was a little swollen. My question though, i experience huge panic attacks and mostly in the evenings i feel so sick. My legs start to shake when so exhausted, i feel dizzy and my brain feels weird. Like it is tingling or at times i feel some pressure on my temples. Can those things be present too? I am so worried all the time, as i never felt this bad in my whole life. I started a gluten, dairy, soy and sugar free diet, i am using also selenium, but i did use lately also 150mcg iodine.(which i stopped immediately) Can you tell me if those brain symptoms can fit thyroid issues? Thank you very much!!
Ingrid – thank you so much for sharing your journey. 💕 I’m so sorry you are struggling with all of this. Anxiety symptoms are very common in people with thyroid disorders. Here are a couple articles I hope you find helpful:
AUTOIMMUNE THYROID DISEASE AND ANXIETY
https://thyroidpharmacist.com/articles/autoimmune-thyroid-disease-and-anxiety
ARE YOU GOING CRAZY OR IS IT JUST YOUR THYROID
https://thyroidpharmacist.com/articles/are-you-going-crazy-or-is-it-just-your-thyroid
Thank you so much for this article, Gave me a better insight on a few symptoms I have that what seems like the doctors don’t taker serious. I have been on this health roller coaster for the past 8 months and its very overwhelming but reading this information proves-I’m not crazy and it’s not just anxiety. I was told I have Hypothyroidism and Hashimoto’s waiting on labs to see if I have any other AI. Thanks again.
Love – my pleasure! I’m so glad you are taking charge of your health and have found this article helpful! You’re not crazy! Pleae keep me posted on your progress.
Do you have a recommended dose of phosphatidylcholine?