May 25th marks World Thyroid Day! This day helps bring awareness to thyroid conditions, and acknowledges those who have thyroid disease, those who study it, and the treatments that surround it. At the end of May, I’m always looking at ways to increase thyroid awareness.
Did you know? Thyroid disease is prevalent throughout the world. The American Thyroid Association estimates that some 20 million Americans have some form of thyroid disease. The vast majority (over 95 percent) of those diagnosed with hypothyroidism have Hashimoto’s thyroiditis, an autoimmune disease.
A research review paper published in 2019 reports that, per results from a large-scale Danish study, the most common subtype of hypothyroidism is spontaneous hypothyroidism (presumably due to an autoimmune component), found in about 84.4 percent of people. Other common causes include postpartum-induced hypothyroidism (4.7 percent), hypothyroidism caused by the medication amiodarone (4 percent), and pregnancy-related immune changes (about 0.09 percent of women per year). [1]
My interest in Hashimoto’s was prompted by my own diagnosis, which came when I was just 27… almost a decade after visiting doctors who said my chronic cough, IBS, anxiety, leg cramps, muscle pain, carpal tunnel, hair loss, bloating, and new food sensitivities were just part of “getting older.”
After much crying to my family and doing what I could to “cover up” my symptoms (hello blonde hair to help cover my thinning hair), I sat down and thought about my clients. They were happy, despite their challenges, and I wanted to be like that too — so I decided to be the healthiest person possible with Hashimoto’s.
Overcoming Hashimoto’s became my personal life mission. Fast forward to today, and here I am: the Thyroid Pharmacist. I want to share the knowledge that I now have about Hashimoto’s, with the world!
In this article, you are going to become knowledgeable in many facts about Hashimoto’s and the thyroid. You’ll also learn:
- Lab tests that everyone who displays symptoms should get
- Why Hashimoto’s is commonly misdiagnosed
- Common nutrient deficiencies that those with Hashimoto’s may have
- Common symptoms associated with Hashimoto’s
Top 10 Facts About Hashimoto’s
My readers are constantly astonished about new facts that they learn regarding Hashimoto’s, so I’ve compiled a list of the top 10 to share with you today. Many facts that you are going to read below, are based on the insights shared by over 2000 of my clients and readers, whom I surveyed back in 2015. (You can read about that survey here.)
1. If you take Synthroid/levothyroxine or have hypothyroidism, low thyroid levels, or a sluggish thyroid, you likely have Hashimoto’s.
Hashimoto’s and hypothyroidism are NOT always the same. While Hashimoto’s is the leading cause of hypothyroidism, there is a difference between Hashimoto’s and hypothyroidism. A person can have one, and not the other.
Most cases of pure hypothyroidism can be remedied by taking thyroid hormones. However, as some 90-97 percent of cases of hypothyroidism are due to advanced Hashimoto’s (autoimmune thyroiditis), Hashimoto’s and the autoimmune attack will remain, even when proper levels of thyroid hormone are restored with medications (unless we find and treat the root cause). [2]
The definition of hypothyroid is a thyroid that doesn’t produce enough thyroid hormone for the body, which is usually made evident by a high TSH and/or low Free T4 and Free T3. Some doctors refer to that as a “sluggish” thyroid.
Hypothyroidism is a clinical state that can occur as a result of different factors, such as iodine deficiency, surgical removal of the thyroid, radioactive iodine treatment, not taking enough thyroid hormone, taking thyroid suppressing medications, or damage to the thyroid from an infection, an accident, or a condition like Hashimoto’s.
Hashimoto’s, on the other hand, is a progressive autoimmune condition that involves the body attacking its own thyroid gland, eventually leading to hypothyroidism. A person in the early stages of Hashimoto’s may not yet have hypothyroidism, just the attack on the thyroid gland. This autoimmune attack on the thyroid can cause symptoms, be triggered by various factors, and be responsive to lifestyle changes. I’ll discuss this further below.
The autoimmune attack on the thyroid develops decades before a person becomes hypothyroid, so catching the condition early allows us to prevent its progression. One may suffer from symptoms of Hashimoto’s for years before they are finally diagnosed with hypothyroidism and given thyroid medications.
Some common symptoms of Hashimoto’s include: anxiety, depression, weight gain, mood swings, fatigue, brain fog, cold hands and feet, and gastrointestinal issues.
Another common symptom is having multiple food sensitivities, especially to gluten, dairy, and soy, which may not show up on a standard blood test, but can manifest as delayed symptoms after consuming these foods. (You can read more about food sensitivities and Hashimoto’s here.)
Hashimoto’s symptoms can be a spectrum: some people feel just fine, yet others may feel debilitated by their symptoms.
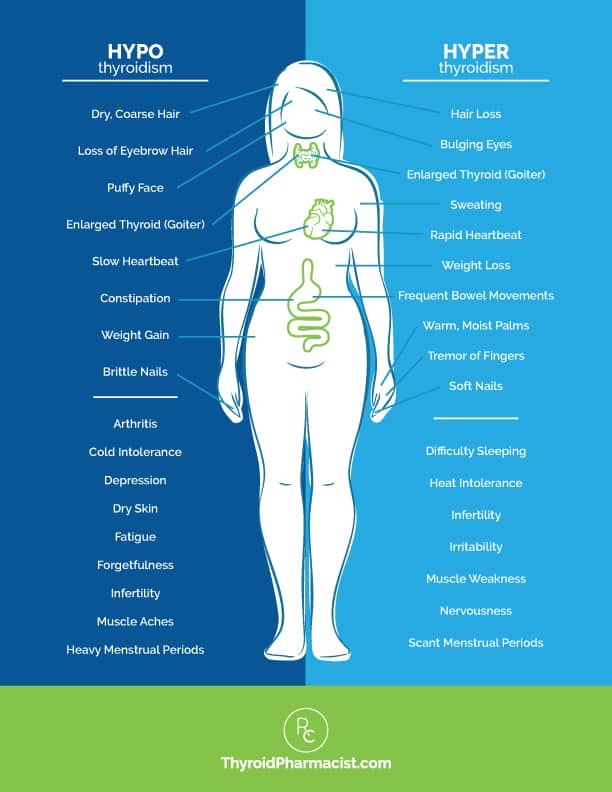
Some common symptoms of Hashimoto’s, based off of hypothyroidism, include:
- Slower metabolism, leading to weight gain
- Forgetfulness
- Feeling cold or cold intolerance
- Depression
- Fatigue
- Dry skin
- Constipation
- Loss of ambition
- Dry, coarse hair
- Muscle cramps
- Stiffness
- Joint pain
- A loss of the outer third eyebrow
- Heavy menstrual periods
- Infertility
- Muscle aches
- Puffy face
- Slow heartbeat
- Brittle nails
- Arthritis
At the other end of the spectrum, when our body is in a hyperthyroid state, symptoms include:
- Weight loss
- Palpitations
- Anxiety
- Eye bulging
- Tremors
- Irritability
- Infrequent menstrual periods
- Fatigue
- Heat intolerance
- Increased appetite
- Hair loss
- Enlarged thyroid gland
- Sweating
- Frequent bowel movements
- Infertility
- Soft nails
- Warm, moist palms
- Finger tremors
- Insomnia
- Muscle weakness
- Nervousness
As you can see in the graphic below, one may experience symptoms of both hypo- and hyperthyroidism.
I personally experienced irritable bowel syndrome, anxiety, and advanced carpal tunnel in both hands, which required me to wear wrist braces. Despite my symptoms, however, I looked fine (except for some bloating). I had hair on my head (despite losing much of it) and I didn’t need crutches (although I experienced leg and muscle pain). When I came home from work, all I could do was eat, watch TV, and fall asleep on the couch.
I was living proof that thyroid symptoms may affect someone, even though they may look fine on the outside!
2. Hashimoto’s can affect fertility and libido.
Women with Hashimoto’s may experience fertility struggles, such as having trouble conceiving and having miscarriages. [3]
In the past, researchers speculated that women with thyroid disease may have a higher risk of having children with birth defects, but later research shows that this is not the case. [4]
However, those who are planning to conceive should note that there are still risks involved when it comes to pregnancy, if hypothyroidism is not treated. Babies born to mothers with untreated hypothyroidism may be at a higher risk for being born with a low birth weight, and there is a higher likelihood that they will be born preterm. [5] Possible additional risks include a lower IQ and neonatal respiratory distress syndrome. [6] (Note that these risks are not tied to Hashimoto’s antibodies specifically.)
Female hormones, such as estrogen, are thought to play a role in the development of autoimmune thyroid conditions. There are also three common periods of major hormonal changes in a woman’s life, where the onset of the disease can occur – puberty, pregnancy, and perimenopause. Estrogen and prolactin have an important role in modulating the immune system, and may impact autoimmune disease. Estrogen can also change the requirements for thyroid hormone, and this may result in an autoimmune condition, especially in the presence of nutrient deficiencies. [7]
Prolactin, released by breastfeeding women to promote milk production, may also become elevated in women with Hashimoto’s (even when they’re not breastfeeding), and has been tied to both increased thyroid antibodies and infertility.
Research has also shown that both women and men with thyroid disease experience a higher prevalence of low libido at some point in their lives.
An estimated 59 to 63 percent of hypothyroid men suffer from sexual function issues including low libido, erectile dysfunction, delayed ejaculation, and sperm abnormalities. Both hypo- and hyperthyroidism are associated with reduced sperm morphology (changes in size or shape which make it less effective), low semen volume and density, as well as reduced motility. [8]
A low sex drive can also be caused by a number of co-occurring chronic health conditions, including other autoimmune diseases. For example, many women who have Polycystic Ovarian Syndrome (PCOS) have shared with me their own challenges with having a low sex drive. Read more about low libido and thyroid conditions here. [9]
Adrenal dysfunction and an impaired cortisol response can also significantly impact libido. When adrenal dysfunction occurs, the body may think it’s in survival mode instead of thriving mode, which means that the adrenal glands can divert the production of “nice to have” hormones (sex hormones like estrogen and progesterone) from seemingly unneeded systems such as the body’s reproductive system, to fuel the production of hormones required for survival, such as cortisol. Basically, if we’re in a state of constant stress, our bodies will be focused on “survival” and not procreation.
In some cases, restoring adrenal function may also be key to restoring the balance of sex hormones in the body, thus helping libido.
Low libido, along with other symptoms including stress, exhaustion, mood swings, blood sugar imbalances, depression, and food cravings, can all be signs that your cortisol production is out of balance. This can, in turn, impact your other hormone systems further.
After struggling with adrenal dysfunction myself, and learning that a lot of people with Hashimoto’s also struggle, I developed a program called the Fatigue and Brain Fog Fix in Six: Thyroid Adrenal Edition (formerly the Adrenal Transformation Program) — 81 percent of course participants reported an improved libido!
Since I saw so much success with this program, I wanted to share it with more people… and that’s how my book, Adrenal Transformation Protocol, came to life. It outlines a four-week program to help identify your adrenal triggers, balance your stress response, and gradually build up your resilience to prevent excess stress from overwhelming your adrenals in the future.
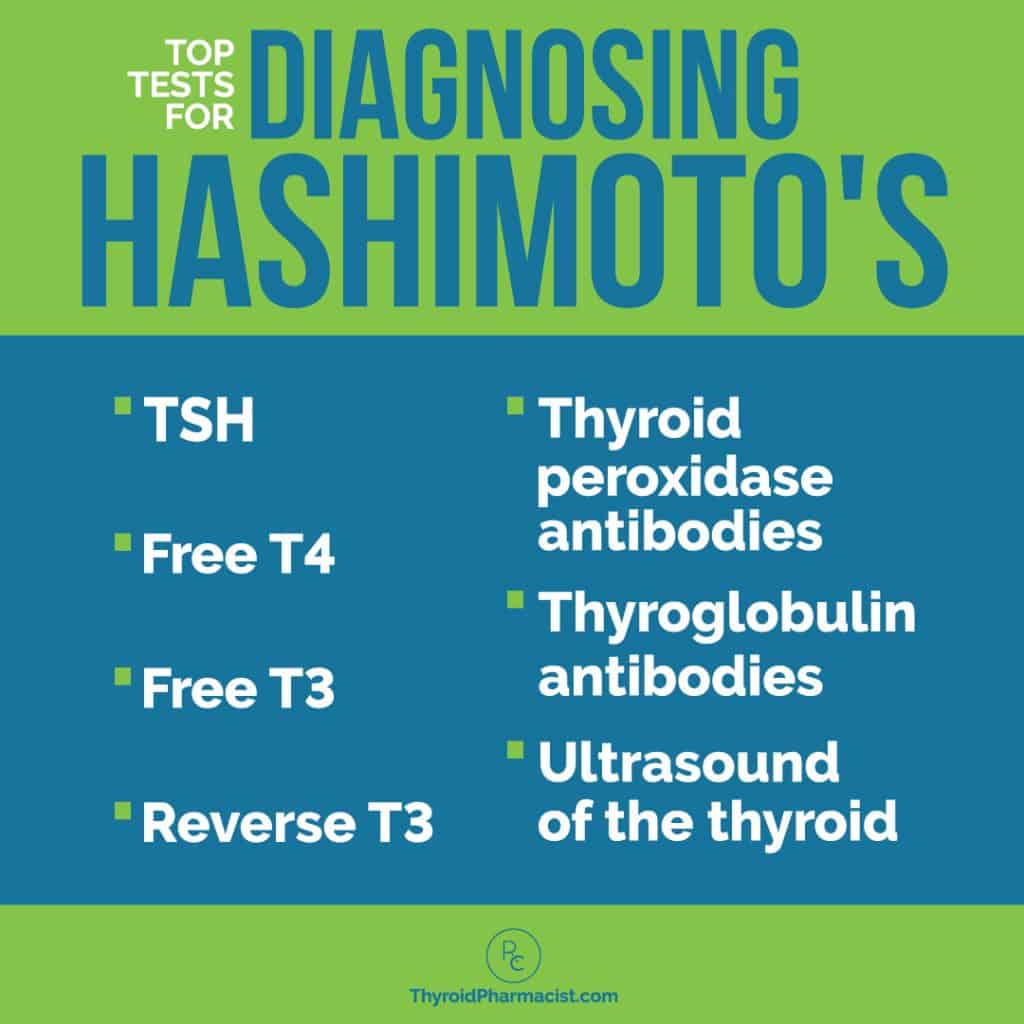
3. Missing a Hashimoto’s diagnosis is more common than you think.
Through my own experience as a patient, from the mouths of many with Hashimoto’s, and due to the outdated guidelines for diagnosing thyroid conditions, I have learned that many doctors don’t test for Hashimoto’s, despite having their patients present with symptoms of thyroid disease.
Many conventional doctors simply test one’s TSH (thyroid stimulating hormone) and T4 levels (the amount of thyroid hormone circulating in your blood), because these values are tested for a general diagnosis of “thyroid disease.” However, these tests don’t decipher between hypothyroidism and Hashimoto’s, and often don’t flag Hashimoto’s or hypothyroidism until a later stage. But this is absurd, as thyroid antibodies can be elevated for as long as 10 years, before a change in TSH is seen! [10]
For this reason, it’s important to have a full thyroid panel done, which includes not only TSH and T4, but also T3, TPO, and TG antibodies (whose presence can show how strong the autoimmune attack on the thyroid is).
Additionally, an ultrasound test can help to diagnose Hashimoto’s, as well as reveal what’s happening with your thyroid and see if there are any nodules present.
I’ll discuss more on how to get a proper diagnosis further on in this article.
4. Getting on the right thyroid medications can be a game-changer.
The conventional medical model treats autoimmune thyroid disorders in the same way as it would treat someone with a nutrient-deficiency-induced thyroid disorder, someone with a congenital defect of the thyroid gland, someone born without a thyroid, or someone who had their thyroid removed and treated with radioactive iodine. To treat these symptoms, synthetic thyroid hormones are often used.
The standard of care is to prescribe levothyroxine (known as T4), which can work wonders for some people’s symptoms. However, this same medication may be completely worthless for other people’s thyroid symptoms.
One reason could be due to poor absorption. Fortunately, Tirosint® (a gluten and dairy-free synthetic T4 hormone medication, free from harmful fillers) became available in 2017. In my survey of over 2000 people with Hashimoto’s, those that switched to Tirosint® experienced a 68 percent improvement in labs. Fifty percent saw an improvement in mood, 62 percent saw an improvement in their energy levels, and 32 percent, an improvement in hair loss. (Read more on this topic in my article, Is your T4 medication working for you?)
Additionally, T4 is a pro-drug, and needs to be turned into the more active T3 in the body, to exert most of its benefits. This conversion happens perfectly on paper and in a petri-dish, but as a pharmacist, I can tell you that it doesn’t always happen that way in every person’s body. Some people may not convert T4 to T3 properly. This could be due to various reasons — including genetics, nutrients, co-occurring conditions, and sometimes even stress.
Of the readers I’ve surveyed, up to 59 percent have felt better taking a combination T4/T3 medication, while up to 43 percent have felt better on a synthetic T4 medication. While 69 percent saw an improvement in their thyroid lab results with the T4-only medication Synthroid® (69 percent), improvements to mood and overall energy were reported in 63 percent of people after switching to a T3/T4 combination medication like Nature-Throid® (which at the time of publication of this article, is not currently available).
Natural Desiccated Thyroid (NDT) is another T4/T3 medication option. This is also sometimes called Desiccated Thyroid Extract (DTE). These medications are derived from the thyroid gland of pigs and are considered to be bioidentical hormones.
NDT medications also contain the thyroid hormones T1 and T2, which may have some physiological activity as well.
Many of my patients who did not feel well on conventional treatments report feeling much better after switching to an NDT medication like Armour®, Nature-Throid®, NP Thyroid® or WP Thyroid® (please note that there have been numerous shortages and recalls of various NDT medications over the last several years, and some of these may not be available). When surveying my readers, I discovered that 59 percent did feel better after switching to Armour®, 57 percent felt better on Nature-Throid®, and 32 percent reported improvement with WP Thyroid® (NP Thyroid® was not readily available when I created the survey). (Note: While Armour does not have any gluten-containing ingredients, it is not tested for gluten content, and as such, is not “certified gluten-free.”) [11]
For those who don’t have access to T3-containing medications, I recommend looking into a better absorbed form of T4, such as Tirosint®. You can also check out my article on thyroid medications for a comprehensive overview of the other available medication options out there, and how you can be sure to get the best outcomes from each of them.
5. Your doctor’s lab reference ranges may be outdated.
The TSH level conventionally considered to be “normal” has been skewed for years. Researchers have shown that, when scientists first determined the reference range for thyroid hormones, they looked at people within the “normal” reference range who were actually hypothyroid, or had naturally higher TSH levels due to being elderly. This caused the normal reference range to be inflated, where a TSH of up to 10 μIU/mL was considered normal. The reference ranges have fortunately been refined in the last few years, with most labs now having 4.5 μIU/mL or 5 μIU/mL as the upper limit of “normal.” However, as a side note, when my TSH was at 4.5 μIU/mL, I felt like a sloth.
In recent years, the National Academy of Clinical Biochemists indicated 95 percent of individuals without thyroid disease have TSH concentrations below 2.5 μIU/L, and a new normal reference range was defined by the American College of Clinical Endocrinologists to be between 0.3 and 3.0 μIU/mL for people taking thyroid medications. However, functional medicine practitioners have found, based on clinical experience, that normal reference ranges should be between 1 to 2 μIU/mL, for a healthy person not taking thyroid medications. Anecdotally, I’ve found that most patients feel best with a TSH between 0.5-2 μIU/mL. [12]
Thus, the goal is to have your thyroid medications help your labs fall into the optimal reference ranges (as noted in the graphic below).
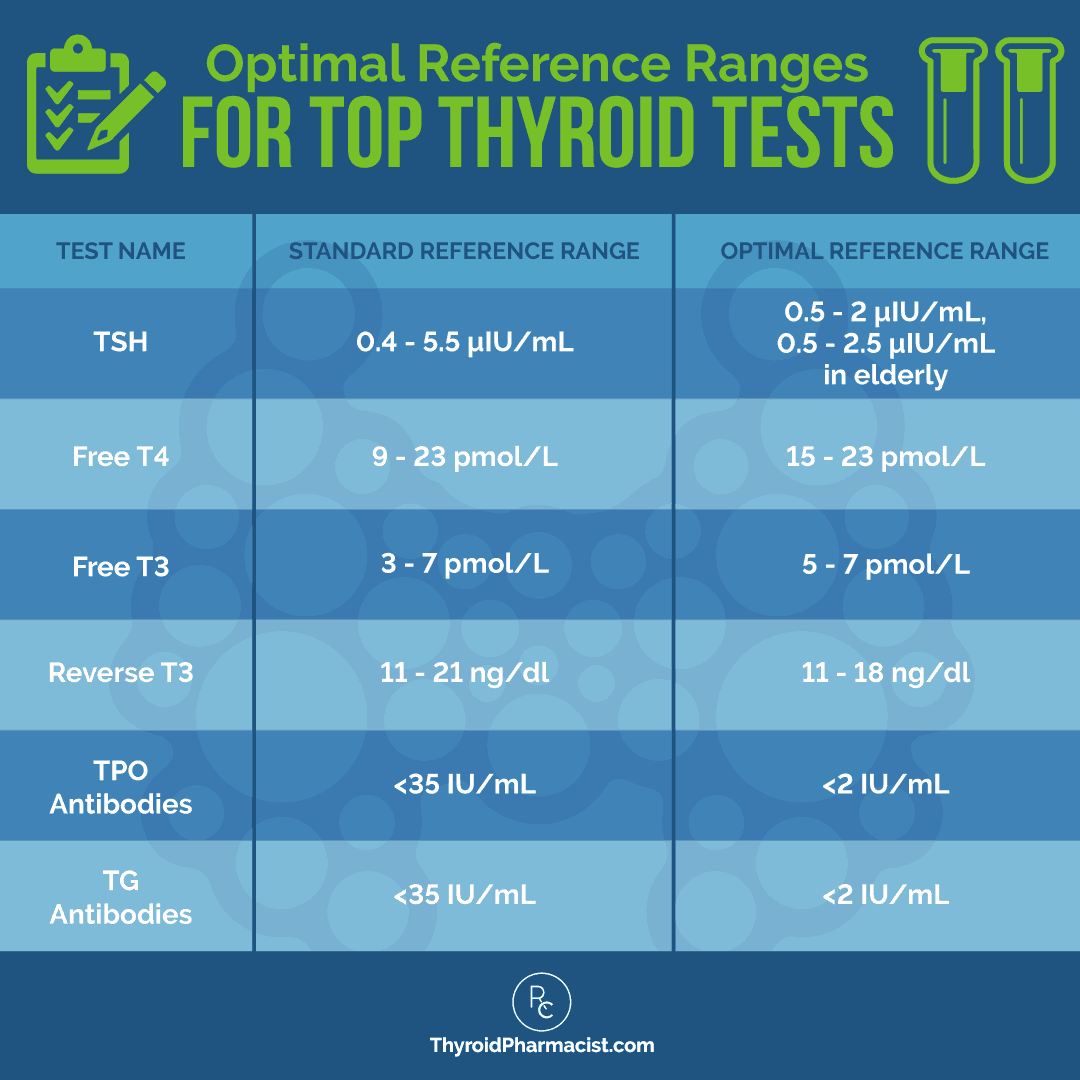
(Although there is an updated range, many conventional doctors have been slow to join in. This is why I encourage you to work with a functional medicine doctor who will treat you, and not just your labs.)
When your thyroid labs are optimal, you may see a reduction in your symptoms.
However, everyone is unique, so the most important thing is that you feel well. If your TSH range is slightly out of the optimal range, but you are feeling better than ever, then I wouldn’t focus so much on the number on your labs. What matters is the absence of symptoms.
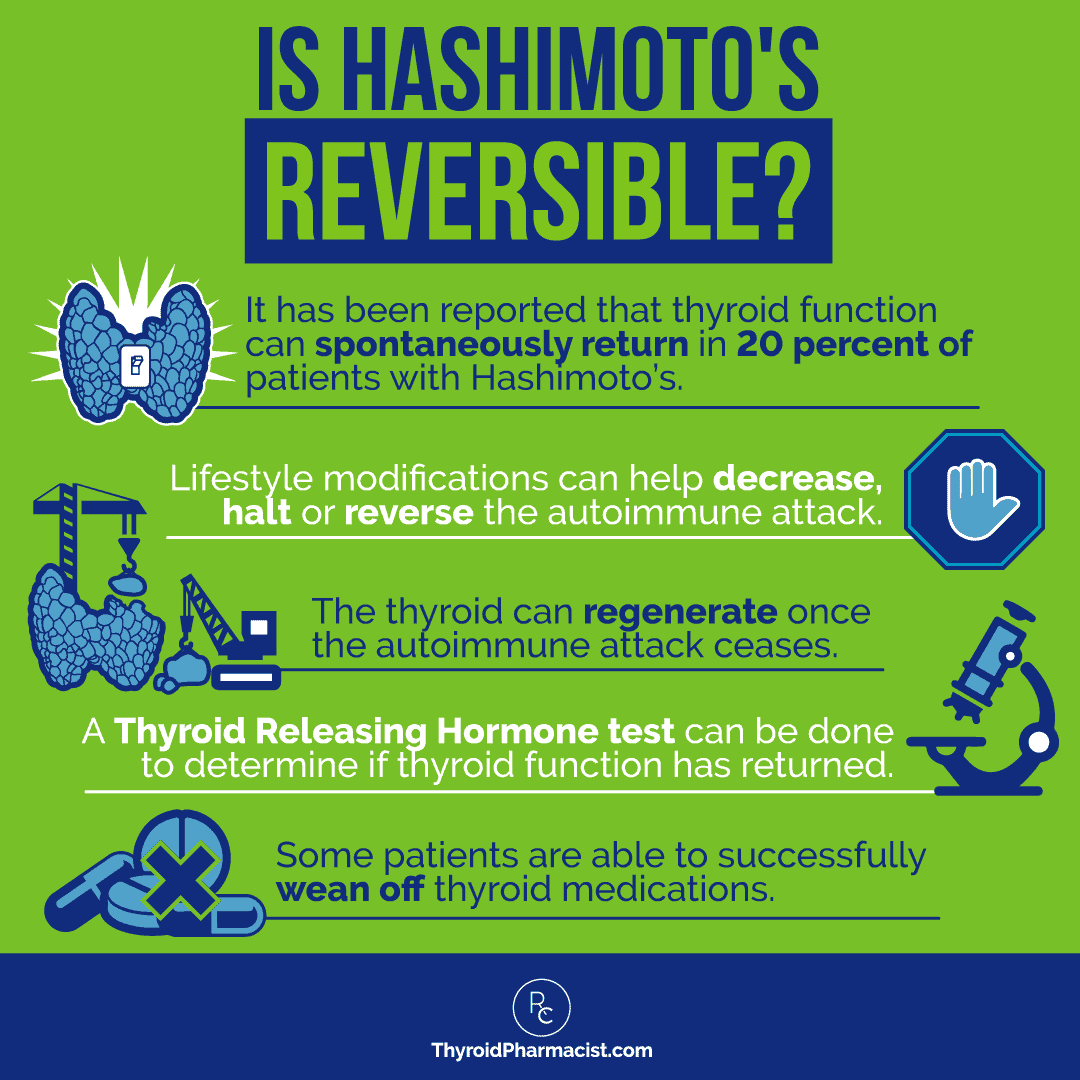
6. Hashimoto’s can be reversed!
Once diagnosed with Hashimoto’s, most people are told that they will be fine as long as they take their synthetic thyroid hormone medication. However, patients don’t get an explanation as to why they have Hashimoto’s, what the autoimmune disease means for their future, and what actions they can do to support their thyroid and autoimmune disease… other than taking medication.
Most doctors dismiss autoimmune conditions as the result of certain genes and believe that once present, they cannot be reversed. However, leading researcher, Dr. Alessio Fasano, has proven otherwise. He has uncovered the three-legged stool of autoimmunity.
According to his research, three factors need to be present for an autoimmune condition to develop:
- A genetic predisposition
- An external trigger
- Intestinal permeability, also known as leaky gut (a condition that involves “holes” in the intestinal lining, which allows toxins and food particles to pass through and further damage our gut)
Dr. Fasano found that, upon removing the intestinal permeability and/or trigger, an autoimmune condition will go into remission. For this reason, I believe in addressing the root causes of Hashimoto’s symptoms to reverse the condition. (And yes, remission is possible with Hashimoto’s!) [13]
7. Many people share common underlying root causes of thyroid disease.
Beyond optimizing thyroid hormones, those who have Hashimoto’s often share these similar root causes.
Food Sensitivities
I’ve found that the most common food sensitivities in people with Hashimoto’s are gluten, dairy, soy, grains (corn, in particular), nightshades (potatoes, tomatoes, and peppers), nuts, and seeds. When someone is first setting out to change their diet, I always recommend completely removing gluten, dairy, and soy.
- In surveying my readers and clients, I’ve found that about 93 percent have felt better on a gluten-free diet.
- Another 75 percent reported feeling better on a dairy-free diet, 73 percent felt better grain-free, and another 60 percent said they felt better soy-free.
- Egg and nightshade-free diets were helpful 40 percent and 35 percent of the time, respectively.
Nutrient Deficiencies
Nutrient depletions contribute to the development of Hashimoto’s, as well as many of its symptoms, and are common in people with Hashimoto’s. They may be caused or exacerbated by symptoms such as low hormone levels and leaky gut. Hypothyroidism makes nutrient extraction from food more difficult and less efficient. [14]
Nutrient deficiencies can also occur as a result of eating nutrient-poor foods, following a calorie-restricted diet, having inflammation from infections or food sensitivities, taking certain medications, or having an imbalance of gut bacteria. Restoring one’s nutrient levels through nutrient-dense foods, supplementation, and optimizing digestion, are some of the fastest ways to feel better with Hashimoto’s and begin to restore the body!
Adrenal Dysfunction and Impaired Stress Response
An impaired stress response is typically the result of cortisol imbalance and adrenal dysfunction.
Stress affects so many different bodily functions, including metabolism, hormone production, immune system regulation, and emotional response. Thyroid function is also decreased when in a stressful situation. The body wants to preserve energy to deal with whatever issue is at hand — whether you are being chased by a bear or stuck in traffic — the adrenal glands cannot decipher what is happening when in a “fight or flight” response, so it reacts the same way. “Fight or flight” mode can save us from danger and help us tackle the challenging situations in life.
However, problems arise when this type of stress is ongoing and the body is constantly suppressing thyroid function to preserve its resources. Additionally, high or low cortisol levels, caused by chronic stress to the adrenal glands, can cause hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar). If left unmanaged, these blood sugar imbalances can lead to hypothyroid symptoms. An increase in cortisol will also disrupt the balance of the HPT (hypothalamic-pituitary-thyroid) axis, which the body relies on to keep thyroid levels steady. [15]
I struggled with exhaustion and an over-reliance on caffeine off and on for years… until I discovered the root cause of this, which was adrenal dysfunction. I developed an effective protocol for myself, which was based on sending safety signals to my body, so that it was able to rest and recover from the chronic cortisol production (this article discusses my safety theory, if you want to learn more).
I started to offer it as the Fatigue and Brain Fog Fix in Six: Thyroid Adrenal Edition (formerly the Adrenal Transformation Program). Participants in the program reported improvements in mental fog (92 percent), fatigue (89 percent), anxiety (86 percent)… and this is just the tip of the iceberg! My book, Adrenal Transformation Protocol, also outlines the protocol! I highly recommend picking up a copy if you are interested in tackling symptoms like mood swings, blood sugar imbalance, food cravings, or depression.
Toxins
Toxins are everywhere in our environment — cosmetics, skin products, pesticides, exhaust fumes… the list goes on! Whatever we inhale, ingest, and absorb into our skin, eventually ends up circulating in our body.
We are frequently exposed to xenoestrogens (found in BPA, soy, phthalates, parabens, etc.), which may increase TSH and perpetuate the autoimmune attack on the thyroid. Some other forms of toxins are halogens (bromide, chloride, and fluoride), which can compete with receptor sites in the thyroid gland and build up in our thyroid tissue, leading to inflammation and thyroid cell death, as they are structurally similar to iodine.
The Environmental Protection Agency (E.P.A) estimates that consumer products used in the U.S. may contain some 40,000 chemicals, but less than one percent have been tested and proven safe for human use. [16] Read more about how to reduce and eliminate toxins in your home in my articles on indoor air quality and flame retardants.
Fluoride
Fluoride is a common toxin that can wreak havoc on the thyroid. It can be found in products like bottled beverages, toothpaste, black and red tea, certain medications, and drinking (tap) water! Fluoride was used to treat hyperthyroidism up until the 1950s, as it is an effective thyroid suppressor at daily doses of 0.9 to 4.2 mg. However, studies confirm that most adults in fluoridated communities ingest between 1.6 and 6.6 mg of fluoride a day, effectively suppressing their thyroid function. A 2015 study out of England reported that people in an area with fluoridated drinking water were twice as likely as those in a non-fluoridated area to report hypothyroidism. [17]
Infections
Bacterial, fungal, and parasitic infections are chronic infections which I often see in those with Hashimoto’s.
Small intestinal bacterial overgrowth or SIBO, Blastocystis hominis, Candida overgrowth, and H. pylori are the triggers of Hashimoto’s that get the least amount of attention, yet identifying and treating them can result in complete remission. There are protocols designed to eradicate them. In 2015, 80 percent of my clients who hit a plateau with nutrition and took the gut tests I recommended, tested positive for at least one gut infection.
Leaky Gut
Leaky gut or Intestinal permeability is one of the factors that must be present for autoimmunity to occur. A leaky gut has gaps in the gut lining that allow irritating molecules and substances to escape from the digestive system, and enter into the bloodstream. In a leaky gut, infections, viruses, and food particles that are able to find their way into the body through the intestinal wall, can cause food sensitivities and a host of other symptoms. This irritation can interrupt the immune system’s ability to regulate itself and put the body into a perpetual “attack mode” that is counterproductive to healing. Even those who have no apparent gastrointestinal symptoms may have a leaky gut, and addressing gut function might be the best place to start to bring healing to the body. If we can reverse leaky gut, we can prevent or reverse autoimmunity altogether.
You can read more about the top root causes of Hashimoto’s, and the dietary and lifestyle interventions that I recommend to address them, in this article. You can also check out my article on the conventional versus root cause approach to learn more about digging for your root cause. [18]
8. Too much iodine can cause Hashimoto’s.
Iodine deficiency can cause hypothyroidism, as iodine is needed for the thyroid to function.
Through the 1900s, iodine deficiency became recognized as a major health concern in certain areas of the U.S. (and worldwide). To address this issue, global health organizations began adding iodine to salt and other foods, and the iodine status of the world’s countries increased. As of 2014, reports from the Centers for Disease Control suggest that the U.S. population has both sufficient and stable iodine intake. [19]
Today, iodine deficiency is rare, and iodine excess is now recognized as a risk factor for developing autoimmune thyroid disease. Most cases of hypothyroidism in the United States, and other countries that add iodine to their salt supply, are caused by Hashimoto’s. [20]
For more information, please read my article about iodine and Hashimoto’s.
9. Diet can be a game-changer for Hashimoto’s.
Using food as medicine (food pharmacology) is one of the most powerful tools you can use to bring your autoimmune condition into remission. I experienced the most healing when I removed the foods I was reacting to from my diet, and addressed my nutrient deficiencies.
Food sensitivities can be a root cause of Hashimoto’s, and can result from a leaky gut that is always present with autoimmunity. In my experience, removing these reactive foods (either permanently or for a period of time) will often alleviate many of the symptoms associated with Hashimoto’s.
Many of my readers and clients have experienced noticeable benefits from removing the following foods:
- 88 percent reported feeling better on a gluten-free diet
- 87 percent reported feeling better on a sugar-free diet
- 81 percent reported feeling better on a grain-free or Paleo diet
- 79 percent reported feeling better on a dairy-free diet
- 63 percent said they felt better on a soy-free diet
- 48 percent felt better when they eliminated eggs from their diet
- 47 percent felt better on nightshade-free diets (nightshades are vegetables like tomatoes, potatoes, peppers, and eggplants)
- 15 percent of people saw improvement with a nut-free diet
- 7 percent reported feeling better off seeds
- 63 to 79 percent of people felt better overall on the Autoimmune Paleo diet, which excludes all of the above-listed foods
Nutrient deficiencies are another common root cause of Hashimoto’s, and can be caused by infections, low stomach acid, fat malabsorption, a deficiency in digestive enzymes, eating nutrient-poor foods, following a calorie-restricted diet, ingesting food sensitivities, taking certain medications, or having an imbalance of gut bacteria.
The most common nutrient deficiencies that I’ve seen in Hashimoto’s are selenium, vitamin D, B12, ferritin (the iron storage protein), thiamine, zinc, and magnesium. Read more about the 7 most common deficiencies of those with Hashimoto’s.
To learn more about the best diet for Hashimoto’s, please take a look at the linked article.
10. Low-dose naltrexone can be helpful for Hashimoto’s.
Naltrexone is an FDA-approved medication used for opioid withdrawal at a dose of 50 mg per day. However, low doses of 1.5 to 4.5 mg per day of this medication have been found to tweak the immune system. They have also shown promise in improving cases of autoimmune disease, including Crohn’s, MS, and Hashimoto’s, as well as other immune system-related conditions such as cancer and HIV/AIDS. Naltrexone has also been reported to enhance immune function by increasing our endogenous endorphin production, reducing inflammation, promoting DNA synthesis, and slowing down motility in the GI tract to facilitate healing.
Low-dose naltrexone (LDN) balances the immune system by increasing the amount of T-regulatory cytokines and modulating TGF-B, leading to a reduction of Th-17 — the promoter of autoimmunity. This means that it turns off the cells that cause autoimmunity! [21]
This medication is available only as a prescription and can be compounded into lower doses by special professional compounding pharmacies. Luckily, even without insurance coverage, this medication is available in generic form and is very affordable, usually costing between $15 to 40 USD per month.
Do You Think (or Know) You Have Hashimoto’s? Here Are Your Next Steps
If you are experiencing symptoms that you have read in this article and think that you may have Hashimoto’s or a thyroid disorder, there are some common tests that you can ask for that can help with a possible diagnosis. If your doctor refuses to order the tests for you, or you don’t have coverage, you can order them through my Ulta Lab test portal, which offers discounted lab tests.
If you do have health insurance, I encourage you to call your insurance company to see if they will cover the tests.
I’ve listed the tests individually below; however, you can also order my Root Cause Thyroid Panel, which bundles all of them together.
- TSH – This stands for “Thyroid Stimulating Hormone.” This test is used to screen for thyroid disease. It is a pituitary gland hormone and responds to high and low amounts of circulating thyroid hormone in the body. In advanced cases of thyroid disease, the test will reveal high or low readings. Following the research, recent recommendations from the American College of Clinical Endocrinologists, and my clinical experience, I’ve found that the optimal reference range is 0.5-2 μIU/mL, and that most people report feeling at their best around 1 μIU/mL.
- Free T4 – This test measures the amount of inactive thyroid hormone circulating in the body. T4 converts into T3, the active version of thyroid hormone. The optimal reference range is 15-23 pmol/L.
- Free T3 – This test measures the active thyroid hormone circulating in the body. The optimal reference range is 5-7 pmol/L.
- TPO & TG Antibodies – Most people with Hashimoto’s will have at least one of these antibodies elevated, and if test results show elevated numbers, this is an indication that the thyroid is essentially attacking itself. The optimal reference range for both TPO and TG antibodies is under 2 IU/mL.
- Thyroid Ultrasound – Some people who have symptoms of thyroid disease or Hashimoto’s, may not have abnormal results on the lab tests mentioned above, which can lead to a misdiagnosis of Hashimoto’s or hypothyroidism. This is where I recommend a thyroid ultrasound to check for any abnormalities of the thyroid. Ideally, I recommend at least one ultrasound, especially for women of childbearing age. Some indications that can be found on an ultrasound include a rubbery thyroid, shrunken thyroid, enlarged thyroid, or abnormal growths in the thyroid. (Read more about nodules and ultrasound tests)
For more information, check out my article on the top 10 thyroid tests!
The Takeaway
I hope that this article has shed some light on how Hashimoto’s and thyroid disease can affect a person, aside from lab results being abnormal. There are so many factors that are involved when one is diagnosed with thyroid disease, and conventional medicine, unfortunately, does not provide the necessary information for proper healing. However, with the Root Cause approach, putting autoimmune thyroiditis into remission is truly possible!
Please share this article with your friends and loved ones via social media to help spread thyroid awareness, in honor of World Thyroid Day!
By spreading this good news, my hope is that all doctors, pharmacists, and other practitioners will understand that the goal of Hashimoto’s and hypothyroidism treatment is not to simply feed the thyroid with synthetic hormone, but to treat each patient as the unique individual they are — as we all are — and to dig deep to discover and address each root cause of their symptoms.
Those of us who have been through misdiagnoses, and have been told by doctors that we are “fine” when we did not feel that way, understand how thyroid disease can seem overwhelming. I want you to know that, although you may have Hashimoto’s, hypothyroidism, or another thyroid disease, you can put your condition into remission and still live life to your fullest potential! I — along with hundreds of my patients — are living proof that it can happen.
While this information may seem daunting, there are people and resources to support you.
For example, you can find a support group for people with Hashimoto’s, like Living with Hashimoto’s Disease. The comfort I received from knowing that there were others going through the same challenges as I, was enormous… and I highly recommend that you join such a group.
I also recommend finding practitioners who are knowledgeable in treating Hashimoto’s from a Root Cause approach. To help get you started, here’s a directory of recommended doctors.
As a final note, I want you to know that support is all around if you or a loved one is diagnosed with Hashimoto’s — you don’t have to battle this on your own. You’ve come to the right place.
Here are some resources that I hope will help you or a loved one on your healing journey:
- Where Do I Start With Hashimoto’s
- Getting Support in Hashimoto’s
- Tasty Thyroid-Friendly Meals
- Top 9 Things to Say to a Friend Diagnosed with Hashimoto’s
- How to Eat for Thyroid Health on a Budget
Ready to dig even deeper? My books Hashimoto’s Protocol: A 90-Day Plan for Reversing Thyroid Symptoms and Getting Your Life Back and Hashimoto’s Thyroiditis: Lifestyle Interventions for Finding and Treating The Root Cause, can help you take those next steps.
Additionally, my cookbook, Hashimoto’s Food Pharmacology: Nutrition Protocols and Healing Recipes to Take Charge of Your Thyroid Health, provides you with over 125 delicious, healing recipes, as well as nutrition protocols, to help take charge of your (or a loved one’s) thyroid.
My newest book, Adrenal Transformation Protocol, is based on a four-week program that I’ve run several times. In it, participants have seen amazing improvements in anxiety, depression, sleep, stress and more. The book is designed to help you recover from the impact of adrenal dysfunction and chronic cortisol production, and I highly suggest that you check it out if you’re struggling with symptoms.
You can also download a Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free! You will also receive occasional updates about new research, resources, giveaways, and helpful information.
I love interacting with my readers on social media, and I encourage you to join my Facebook, Instagram, TikTok, and Pinterest community pages to stay on top of thyroid health updates and meet others who are following similar health journeys. For recipes, a FREE Thyroid Diet start guide, and notifications about upcoming events, be sure to sign up for my email list!
References
[1] Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We’ve Been and Where We’re Going. Adv Ther. 2019;36(Suppl 2):47-58. doi:10.1007/s12325-019-01080-8; Hashimoto’s Disease. National Institute of Diabetes and Digestive and Kidney Diseases. U.S. Department of Health and Human Services. June, 2021. Accessed May 11, 2022. https://www.niddk.nih.gov/health-information/endocrine-diseases/hashimotos-disease
[2] Amino N. Autoimmunity and hypothyroidism. Baillieres Clin Endocrinol Metab. 1988;2(3):591-617. doi:10.1016/s0950-351x(88)80055-7
[3] Koyyada A, Orsu P. Role of hypothyroidism and associated pathways in pregnancy and infertility: Clinical insights. Tzu Chi Med J. 2020;32(4):312-317. Published 2020 Apr 10. doi:10.4103/tcmj.tcmj_255_19; Allam MM, El-Zawawy HT, Barakat SS, Ahmed SM, Saleh RNM. A hidden cause of infertility in hypothyroid patients. Clin Case Rep. 2020;8(2):374-378. Published 2020 Jan 14. doi:10.1002/ccr3.2654
[4] American Thyroid Association. Risk of birth defects in the babies of women with thyroid disease. Feb. 11, 2022. https://www.thyroid.org/risk-of-birth-defects-in-the-babies-of-women-with-thyroid-disease/; Khoury MJ, Becerra JE, d’Almada PJ. Maternal thyroid disease and risk of birth defects in offspring: a population-based case-control study. Paediatr Perinat Epidemiol. 1989;3(4):402-420. doi:10.1111/j.1365-3016.1989.tb00528.x
[5] Andersen SL, Olsen J, Wu CS, Laurberg P. Low Birth Weight in Children Born to Mothers with Hyperthyroidism and High Birth Weight in Hypothyroidism, whereas Preterm Birth Is Common in Both Conditions: A Danish National Hospital Register Study. Eur Thyroid J. 2013;2(2):135-144. doi:10.1159/000350513; Derakhshan A, Peeters RP, Taylor PN, et al. Association of maternal thyroid function with birthweight: a systematic review and individual-participant data meta-analysis. Lancet Diabetes Endocrinol. 2020;8(6):501-510. doi:10.1016/S2213-8587(20)30061-9
[6] Lee SY, Cabral HJ, Aschengrau A, Pearce EN. Associations Between Maternal Thyroid Function in Pregnancy and Obstetric and Perinatal Outcomes. J Clin Endocrinol Metab. 2020;105(5):e2015-e2023. doi:10.1210/clinem/dgz275; Smallridge RC, Ladenson PW. Hypothyroidism in pregnancy: consequences to neonatal health. J Clin Endocrinol Metab. 2001;86(6):2349-2353. doi:10.1210/jcem.86.6.7577
[7] Moulton VR. Sex Hormones in Acquired Immunity and Autoimmune Disease. Front Immunol. 2018;9:2279. Published 2018 Oct 4. doi:10.3389/fimmu.2018.02279; Santin AP, Furlanetto TW. Role of estrogen in thyroid function and growth regulation. J Thyroid Res. 2011;2011:875125. doi:10.4061/2011/875125; Ansari MS, Almalki MH. Primary Hypothyroidism with Markedly High Prolactin. Front Endocrinol (Lausanne). 2016;7:35. Published 2016 Apr 26. doi:10.3389/fendo.2016.00035
[8] Gabrielson AT, Sartor RA, Hellstrom WJG. The Impact of Thyroid Disease on Sexual Dysfunction in Men and Women. Sex Med Rev. 2019;7(1):57-70. doi:10.1016/j.sxmr.2018.05.002; La Vignera S, Vita R. Thyroid dysfunction and semen quality. Int J Immunopathol Pharmacol. 2018;32:2058738418775241. doi:10.1177/2058738418775241
[9] Arduc A, Aycicek Dogan B, Bilmez S, et al. High prevalence of Hashimoto’s thyroiditis in patients with polycystic ovary syndrome: does the imbalance between estradiol and progesterone play a role?. Endocr Res. 2015;40(4):204-210. doi:10.3109/07435800.2015.1015730; Manole D, Schildknecht B, Gosnell B, Adams E, Derwahl M. Estrogen promotes growth of human thyroid tumor cells by different molecular mechanisms. J Clin Endocrinol Metab. 2001;86(3):1072-1077. doi:10.1210/jcem.86.3.7283
[10] Hutfless S, Matos P, Talor MV, Caturegli P, Rose NR. Significance of prediagnostic thyroid antibodies in women with autoimmune thyroid disease. J Clin Endocrinol Metab. 2011;96(9):E1466-E1471. doi:10.1210/jc.2011-0228
[11] Dayan C, Panicker V. Management of hypothyroidism with combination thyroxine (T4) and triiodothyronine (T3) hormone replacement in clinical practice: a review of suggested guidance. Thyroid Res. 2018;11:1
[12] Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association [published correction appears in Endocr Pract. 2013 Jan-Feb;19(1):175]. Endocr Pract. 2012;18(6):988-1028. doi:10.4158/EP12280.GL; Kratzsch J, Fiedler GM, Leichtle A, et al. New reference intervals for thyrotropin and thyroid hormones based on National Academy of Clinical Biochemistry criteria and regular ultrasonography of the thyroid. Clin Chem. 2005;51(8):1480-1486. doi:10.1373/clinchem.2004.047399; Esfandiari NH, Papaleontiou M. Biochemical Testing in Thyroid Disorders. Endocrinol Metab Clin North Am. 2017;46(3):631-648. doi:10.1016/j.ecl.2017.04.002
[13] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x.
[14] Hu S, Rayman MP. Multiple Nutritional Factors and the Risk of Hashimoto’s Thyroiditis. Thyroid. 2017;27(5):597-610. doi:10.1089/thy.2016.0635; Bargiel P, Szczuko M, Stachowska L, et al. Microbiome Metabolites and Thyroid Dysfunction. J Clin Med. 2021;10(16):3609. Published 2021 Aug 16. doi:10.3390/jcm10163609
[15] Helmreich DL, Parfitt DB, Lu XY, Akil H, Watson SJ. Relation between the hypothalamic-pituitary-thyroid (HPT) axis and the hypothalamic-pituitary-adrenal (HPA) axis during repeated stress. Neuroendocrinology. 2005;81(3):183-192. doi:10.1159/000087001; Cortisol Imbalance Can Cause Different Issues – DUTCH Test. Dutchtest.com. 2018. https://dutchtest.com/2016/08/23/cortisol-imbalance-can-cause-different-issues/. Accessed February 25, 2018; Cook SB. Current Controversy: Does Adrenal Fatigue Exist? Defending an integrative approach to HPA axis dysfunction. Natural Medicine Journal. October 4, 2017. Accessed May 11, 2022. https://www.naturalmedicinejournal.com/journal/current-controversy-does-adrenal-fatigue-exist
[16] De Coster S, van Larebeke N. Endocrine-disrupting chemicals: associated disorders and mechanisms of action. J Environ Public Health. 2012;2012:713696. doi:10.1155/2012/713696; Zanolli, L. and Oliver, M. Explained: the toxic threat in everyday products, from toys to plastic. The Guardian. May 22, 2019. Accessed May 11, 2022. https://www.theguardian.com/us-news/2019/may/22/toxic-chemicals-everyday-items-us-pesticides-bpa
[17] Connett, M. Fluoride’s Impact on Thyroid Hormones. Fluoride Action Network. January, 2016. Accessed May 11, 2022. https://fluoridealert.org/studies/thyroid03/
[18] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x; Cayres LCF, de Salis LVV, Rodrigues GSP, et al. Detection of Alterations in the Gut Microbiota and Intestinal Permeability in Patients With Hashimoto Thyroiditis. Front Immunol. 2021;12:579140. Published 2021 Mar 5. doi:10.3389/fimmu.2021.579140
[19] Iodine. Fact Sheet for Health Professionals. National Institutes of Health Office of Dietary Supplements. Updated April 28, 2022. Accessed January 5, 2023. https://ods.od.nih.gov/factsheets/Iodine-HealthProfessional/
[20] Hashimoto’s Disease. National Institute of Diabetes and Digestive and Kidney Diseases. U.S. Department of Health and Human Services. June 2021. Accessed May 11, 2022. https://www.niddk.nih.gov/health-information/endocrine-diseases/hashimotos-disease
[21] Li Z, You Y, Griffin N, Feng J, Shan F. Low-dose naltrexone (LDN): A promising treatment in immune-related diseases and cancer therapy. Int Immunopharmacol. 2018;61:178-184. doi:10.1016/j.intimp.2018.05.020; Younger J, Parkitny L, McLain D. The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain. Clinical Rheumatology. 2014;33(4):451-9. doi: 10.1007/s10067-014-2517-2.
Originally published in May of 2019, this article has been revised and updated for accuracy and thoroughness.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Thank you so much Izabella! I was so blessed the day I discovered you and your work. You have the biggest heart!
Patty – thank you so much for your kind words and support. <3
I am looking for a dr in nyc. When I hit the directory list it did not download.
Thanks
Kathy – thank you for reaching out. I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
Kathy, I go to John Salerno. He has an office in NYC and an office in CT. He’s awesome! He is the dr that diagnosed me after 5 years of going to doctors to figure out what was wrong! After our first appt, he diagnosed me. Did bloodwork and the TRH/TSH test and he was spot on! No other doctor was thorough!
Patricia, thank you so much for sharing! <3 I would love it if you would share your doctor you have had great success with to our Recommended Practitioners database. It could make all the difference for someone who has been unable to find a good practitioner. Follow the link below and scroll to the bottom, then once you click "Accept" you'll then be able to see the lists and icons for each country: https://thyroidpharmacist.com/database-submit-your-thyroid-clinican-recommendation/
This shocked me a bit ” 20 million Americans have some form of thyroid disease. Estimates are that between 90 and 97 percent of those diagnosed with hypothyroidism in the United States actually have Hashimoto’s” that’s a quite a lot of people :O Anyhow, amazing and informative post, thank you very very much for writing it!
Titus – you are very welcome! <3 I hope you will keep me posted on your progress.
Thanks for all the work you do and the info you provide on this site, free of charge.
Do you have an opinion on nigella seeds as a supplement for Hashi symptoms?
Izabel – you are very welcome! Black Cumin Seed (Nigella Sativa) is a spice which can be used as a seasoning for food and has been used for medicinal purposes for thousands of years. Here is an article you might find helpful:
BLOOD SUGAR IMBALANCES AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/blood-sugar-imbalances-and-hashimotos/
Hi Izabella,
How exactly does corn effect the thyroid with Hashimoto’s?
Thank you.
Dave
Dave – thank you for reaching out. <3 The most common food sensitivities found in people with Hashimoto’s are gluten, dairy, soy, grains (corn, in particular), nightshades (potatoes, tomatoes, and peppers), nuts, and seeds. Did you know that reactive foods trigger an inflammatory response in the GI tract, leading to malabsorption of nutrients (gluten sensitivity, in particular, has been implicated in causing a Selenium deficiency, a well-known risk factor for Hashimoto's), and can also produce intestinal permeability whenever they are eaten? Most people will see a dramatic reduction in gut symptoms, brain symptoms, skin breakouts, and pain by eliminating the foods they are sensitive to. Some will also see a significant reduction in thyroid antibodies! An additional subset of people will actually be able to get their Hashimoto's into complete remission just by getting off the foods they react to, normalizing their thyroid antibodies, and some even normalizing their thyroid function! Here are a couple of articles you may find helpful.
FOOD SENSITIVITIES AND HASHIMOTO'S
https://thyroidpharmacist.com/articles/food-sensitivities-and-hashimotos
AUTOIMMUNE PALEO DIET
https://thyroidpharmacist.com/articles/autoimmune-paleo-diet
Do you know anyone who can provide similar information/help to someone who has hyperthyroidism? My endocrinologist has been trying to get me to “nuke” my thyroid since I was diagnosed with hyperthryroidism ~12 months ago and I won’t do it.
Thanks!
Michelle – thank you so much for reaching out. <3 I understand how frustrating this can be. My protocols are designed to help those with thyroid autoimmune disease heal by focusing on gut health, nutrient deficiencies, and root cause discovery and treatment. Graves and Hashimoto's are both autoimmune conditions that affect the thyroid. They are thought to be closely related. Sometimes one turns into the other. The difference is the site of the antibody attack. In Hashimoto's, the antibodies are found to thyroglobulin (in 80%) and thyroid peroxidase (TPO) enzyme (in 95% of people) Hashimoto's results in hypothyroidism and is usually treated with Synthroid and replacement hormone.
The same antibodies may be present in a smaller percentage of people who have Graves, but the main antibody is to the TSH Receptor (TSHR-Ab). Usually, people with Graves have hyperthyroidism, and they are treated conventionally with thyroid suppressing drugs (methimazole) or radioactive iodine to destroy the thyroid. At that point, the thyroid will no longer produce hormones on its own, and these people end up on Synthroid as well.
Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target. I hope this helps! You may find these resources helpful as well.
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Hi Isabella, thank you for your excellent help & very informative articles on Hashimotos.
I would so appreciate your comment on my sister’s case.
Female age 54. Diagnosed Hashimotos in 2011. Been on Armour med. since then. Recent blood tests showed:
TSH is 6.6 mIU/L, T4 is 12.0pmol/L and T3 is 5.1 pmol/L,
ferritin is 105ug/L, neutrophils are 1.6 x10e9/L, WBC are 4.3 x10e9/L.
Liver function shows low total protein 65g/L. B12 is 252pmol/L.
A new development has now occurred, in that, her PTH is 14.0 and calcium is high at 2.63mmol/L and adjusted calcium is 2.64 mmol/L.
Test showed low Vit D. Renal function tests all within range. It has been suggested that she could have a parathyroid tumour, but is at present “being monitored” and given high Vit D. supplements.
Bone density scan shows osteopenia and osteoporosis. Eclasta has also been suggested, but she is not keen on this, because of the side effects. She seeing an endocrinologist in 4 months time for further tests.
Can hypercalcaemia be reversed naturally? I read that the stats for hyperparathyroidism in the US and parathyroid tumours are also high. What do you think is the cause of this? Glyphosates?
I have sent my sister your articles on dietary advice and she is following this…no gluten, etc.
Should she change the Armour meds ? She is on no other medication, but is experiencing heart palpitations, feels dizzy, nervous & anxious, very emotional, tired. Has had a stressful life in the last 10 years. Has to go to bed early to be able to work. Gets chest infections at least once a year. Would Ashwaganda and NAC be good option for her, plus B12 & “ABC’s” you suggested. Should she have K2 and selenium?
Thank you for your help once again
Lorraine – thank you so much for your support and for sharing my research with our sister. <3 Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Hashimoto’s is a complicated condition with many layers that need to be unraveled. While conventional medicine only looks at each body system as a separate category and is only concerned with the thyroid’s ability to produce thyroid hormone, Hashimoto’s is more than just hypothyroidism, it's an autoimmune disease that needs to be managed. Whether you have all, part or no thyroid, the autoimmunity still persists in most cases. We need to re-balance the immune system which begins in the gut. With the exception of discussing proper thyroid medication dosing, the majority of my website and book's focuses on balancing the immune system. The info I present is based on my own research and journey overcoming my autoimmune thyroid condition.
Here are some articles I think you might find helpful:
IMPORTANCE OF GUT HEALTH
https://thyroidpharmacist.com/articles/importance-gut-health/
WHERE DO I START WITH HASHIMOTO’S
https://thyroidpharmacist.com/articles/where-do-i-start-with-hashimotos/
Doctor Izabella,
My TSH recently tested in at 9.37. At this time, I began taking 15mg of Armour Thyroid daily. Fast-forward 30 days later and my TSH is showing 11.74! This is certainly not the result I had expected, and I’m wondering if Armour thyroid could be harming more than helping. I have been beaten down by my Hashimoto’s for over 15 years and I am desperate for answers.
Thank you,
Emily
Emily – thank you for reaching out. <3 I understand how frustrating this can all be! There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. Have you read these articles?
WHICH THYROID MEDICATION IS BEST?
https://thyroidpharmacist.com/articles/which-thyroid-medication-is-best/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
HOW THE DOSE OF YOUR THYROID MEDICATION CAN UNCOVER YOUR ROOT CAUSE
https://thyroidpharmacist.com/articles/the-dose-of-your-thyroid-medication-can-uncover-your-root-cause/
HOW TO GET ACCURATE LAB TESTING WHEN TAKING MEDICATIONS
https://thyroidpharmacist.com/articles/how-to-get-accurate-lab-tests-when-taking-thyroid-medications/
When a patient goes on LDN, how long are they likely to be on it? For life? Or can a relatively brief course of LDN reset the body so that, providing other factors such as stress and diet are addressed, long-term LDN is no more beneficial than a brief course?
Does the stock-standard doctor prescribe LDN for hashimotos or does a patient need to find a functional/integrative doctor?
Are there side-effects and risks from LDN?
Tanya – thank you for reaching out. Here is an article you may find helpful:
LOW DOSE NALTREXONE AND HASHIMOTOS
https://thyroidpharmacist.com/articles/low-dose-naltrexone-and-hashimotos
Hi all my labs are good optimal except free t3 lower end of range and total low T3 doctors won’t treat they say it’s stress n have food sensitivities n chemical . Also hair shedding for 6 years after my second son also recently stop breastfeeding my 3 rd at 2 1/2 years . Having low essential fatty acids levels ? Thks Y.T.
Yessy – thank you for sharing your journey. I’m so sorry you are struggling with all of this. <3 Hashimoto’s is often a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better. Hashimoto's is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission.
You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto's. Once you do, you will know what types of changes you need to implement to make yourself feel better.
If you need further support, please check out the list of lab tests inside the “Testing” chapter of my book, Hashimoto’s Root Cause. I also offer a 12-week program, Hashimoto's Self Management Program. Here are some resources I hope you find helpful as well.
BUILDING YOUR OWN HEALTH TIMELINE
https://thyroidpharmacist.com/sample-health-timeline/
Hashimoto’s Self-Management Program
https://thyroidpharmacist.com/enroll-in-hashimotos-self-management/
Hi I’m in the uk.
I’ve been getting thyroid storms. Originally diagnosed with hasimotos but this doesn’t appear to have been conveyed to my drs. Just hypothyroidism and treated with levothyroxine. I’ve been to see a specialist as the last one I went overactive and was really unwell for months. Specialist was unconcerned normal range t4 now so why are you here comments. Finally did a T3 ( for some reason this is no longer tested as standard )and a cortisol test which they lost.
Any thoughts as to what happening that I’m getting these debilitating episodes and suggestions I can put to specialist as to tests etc. Each time it’s getting worse and very difficult to live through. Severe weight loss ,high levels of anxiety and depression , mood changes,loss of appetite, heart palpitations.
Many thanks
K
Karen – thank you for reaching out. <3 I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic diseases, rather than disease symptoms. If you cannot find a Functional Medicine practitioner in your area, it is possible to work with an
overseas practitioner remotely via Skype or some other online video platform. Here's a link which might help:
https://thyroidpharmacist.com/database-recommended-clinicians/
Dr Izabella,
I am so thankful that our PCP suggested we get your book “Root Cause”. I feel like I have become an advocate for those who are diagnosed with thyroid disease, sharing as much information as I’ve learned over the past year. Last year 2019, my 23 y/o son was dx with Hashimoto’s Thyroiditis after having symptoms (which we had NO idea where they could be coming from) and resulting with a TSH of 423! Yes, that is not a typo and his TPO antibodies were in the 10,000 range. I feel like I cannot get enough information and just purchased The Thyroid Secret. My son is GF/DF and on Levythyroxine and feeling SO much better and also started taking Selenium, D3 and Curcumin. He recently visited a functional medicine physician who ordered blood, urine and stool testing (again at the request of our PCP) who is very much on board as he has thyroid disease. Our goal is to continue to get the TSH lower and the TPO antibodies lower. Would appreciate any information on those topics specifically. His recent TSH is 33 and the Free T3/Free T4 normal range, thank God. His TPO antibodies are still elevated , but doctor said they will take a while to come down.
MUCH respect and thankfulness for you. God bless you
Nancy, thank you for sharing your son’s journey! I’m so glad you have found a practitioner! Here are some articles you may find helpful:
HASHIMOTO’S AND THYROID ANTIBODIES: PART 1
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
WHAT TO DO IF YOUR TSH IS NORMAL AND YOU ARE ANYTHING BUT
https://thyroidpharmacist.com/articles/what-to-do-if-your-tsh-is-normal-and-you-are-anything-but/
5 STAGES OF HASHIMOTO’S THYROIDITIS
https://thyroidpharmacist.com/articles/5-stages-hashimotos-thyroiditis/
This was so helpful, I need to find a good doctor in my area? I am in New Jersey close to Philadelphia.
Any recommendations or are you close?
I can’t seem to find anyone with your type of knowledge.
Thank you again.
Natascha, thank you for reaching out. <3 I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It's a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
I notice that the range values for T3 & T4 are given in pmol/L, but the labs that I have tested at give their results in ug/dL. Do you have updated range numbers in that form of measurement?
Joy – thank you for reaching out. <3 Different labs will have different ranges, a good general guideline is to get your Free T4 in the top half of the range, your Free T3 in the top half to top quarter of the range and your TSH around 1.5 or below. Here is an article you might find interesting as well:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
I have had Hashimotos for 5 plus years. Prior to that I was very thin, since then I’ve gained 60lbs, am so puffy, and have no energy. I’m on synthroid and levothyrine (sp?). I live in a fog and feel hopeless. I am desperate to lose weight. I’ve been an ethical vegan for years, don’t eat completely healthy all the time though.
Meg – thank you so much for reaching out and sharing your journey. ❤️ I’m so sorry you are struggling with all of this. Hashimoto’s is often a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better.
Hashimoto’s is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission.
You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto’s. Once you do, you will know what types of changes you need to implement to make yourself feel better.
If you need further support, please check out the list of lab tests inside the “Testing” chapter of my book, Hashimoto’s Root Cause. I also offer a 12-week program, Hashimoto’s Self Management Program. Here are some resources I hope you find helpful as well. ❤️
BUILDING YOUR OWN HEALTH TIMELINE
https://thyroidpharmacist.com/sample-health-timeline/
BEST DIET FOR HASHIMOTO’S AND HYPOTHYROIDISM
http://thyroidpharmacist.com/articles/best-diet-for-hashimotos-hypothyroidism
Hashimoto’s Self-Management Program
https://thyroidpharmacist.com/enroll-in-hashimotos-self-management/
ROOT CAUSE RESET
https://thyroidpharmacist.com/enroll-in-root-cause-reset/
Thank you Dr. Wentz for this information. I was just diagnosed with Thyroid Disorder. It’s only been a few weeks. They are still trying to find out what’s wrong. It is a bit frustrating. I have not experienced any real symptoms yet. Don’t know what’s going on. I have my follow-up with my endocrinologist in a couple of weeks. My TSH on 11/11/21 was 0.15uiU/ML– too low. On 1/17/22 my doctor retested me and my TSH is now 4.37 uiU/ML. I think this is too high. I am so confused. The resources on your website, I believe will help me understand my condition.
Camille – thank you so much for following! ❤️ Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. Here are some articles I hope help you get started:
TOP 10 THYROID TESTS AND HOW TO INTERPRET THEM
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
WHERE DO I START WITH HASHIMOTO’S
https://thyroidpharmacist.com/articles/where-do-i-start-with-hashimotos/
OVERCOMING HASHIMOTO’S
https://thyroidpharmacist.com/articles/overcoming-hashimotos-in-the-new-year
Hi Dr. Isabella, thank you for your excellent explanation regarding Hashimoto. I am 18 year old male and have been diagnosed with Graves Disease. I have been on Methimazole for the past 5 months and since my test results have changed drastically –
TSH increased significantly – was 0.001 and currently 9.1
T4 was 3.0 and now 4.4
Free T4 was 1.95 and is now 0.8
T3 was 170 and now 323
I was told I have Hyperthyroidism due to Graves disease and seems like I am now leaning towards Hypothyroidism. Your advice and thoughts would be greatly appreciated.
Sanjay – thank you for reaching out and sharing. ❤️ Graves and Hashimoto’s are both autoimmune conditions that affect the thyroid. They are thought to be closely related. Sometimes one turns into the other. The difference is the site of the antibody attack. In Hashimoto’s, the antibodies are found to thyroglobulin (in 80%) and thyroid peroxidase (TPO) enzyme (in 95% of people) Hashimoto’s results in hypothyroidism and is usually treated with Synthroid and replacement hormone. The same antibodies may be present in a smaller percentage of people who have Graves, but the main antibody is to the TSH Receptor (TSHR-Ab). Usually, people with Graves have hyperthyroidism, and they are treated conventionally with thyroid suppressing drugs (methimazole) or radioactive iodine to destroy the thyroid. At that point, the thyroid will no longer produce hormones on its own, and these people end up on Synthroid as well. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target. We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here is an article you might find helpful:
GRAVES AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/graves-vs-hashimotos/
Thank you for all your hard and outstanding work! I’m so fortunate I found you! I am newly diagnosed with Hashimoto’s Thyroditis and really want to drop weight, lose the chronic inflammation and hopefully heal my Hashimotos before I need medicine (I have a few weeks left to try whatever I can before decisions need to be made). I have started the AIP diet and hopefully start healing soon.
Thank you so much for all of this!
Danielle, Thank you so much for your kind words! I’m so glad my work has been helpful to you. Starting the AIP diet is a great step in managing Hashimoto’s and reducing inflammation. As you continue this healing journey, it’s important to also focus on addressing potential triggers like stress, gut health, and nutrient deficiencies (e.g., vitamin D, selenium). Restoring thyroid function through lifestyle changes and diet can be incredibly supportive, and you’re on the right path! You’ve got this, stay patient and consistent, and I’m wishing you all the best as you work toward healing. Please keep me posted on your progress.