I’ve always had a passion for advocating for, and serving, vulnerable and underserved individuals. Before becoming the Thyroid Pharmacist as a result of my own Hashimoto’s journey, I was focused on helping geriatric adults, people with mental health issues, and individuals with special needs.
In high school, I assisted at a recreational program for kids with developmental disabilities. In pharmacy school, I applied a nutritional approach while completing my rotations working with adults with developmental disabilities and autism.
After pharmacy school, my favorite job was working for a case management company that served people with developmental disabilities, and I also was studying to become a geriatric pharmacist (before my Hashimoto’s diagnosis) so that I could better advocate for our elderly clients who were often overmedicated.
One common thread among my clients with developmental disabilities and psychiatric conditions, as well as the elderly and those with Hashimoto’s, has always been… constipation!
In my clients with developmental disabilities, constipation was such a huge issue that some of them had life-threatening fecal impactions, and my team asked me to put together multiple in-services to spread awareness about constipation. (My response: “Can I call it ‘Talking Sh*t with Izabella Wentz’?”)
When I was working as a clinical pharmacist, my recommendations focused on pharmaceutical options. I often recommended medications for constipation, and/or recommended reevaluating the use of other medications that can cause and/or worsen constipation.
I’ve learned a ton since that time, and I’m excited to share practical solutions that are easy to implement for safe and effective constipation relief, even if you think you’ve tried everything.
In this article, you will learn:
- What constipation is, and why it should be addressed
- The connection between constipation and Hashimoto’s
- The conventional approach to constipation
- The root cause approach to constipation
What is Constipation?
Constipation is classified as a syndrome and may include the infrequent (fewer than three a week) or difficult passage of stool, hardness of stool, and/or a feeling of incomplete evacuation. [1]
The Rome IV Diagnostic Criteria (a system developed to classify the functional gastrointestinal disorders) for chronic constipation, states that these symptoms must be present for six months or greater, and must accompany at least 25 percent of bowel movements in the last three months.
Pharmacologic studies that look at constipation define it as less than three bowel movements per week, along with the presence of at least one of the above symptoms in more than 25 percent of bowel movements. [2]
As a pharmacist who is well-versed in functional medicine, I like to see my clients have at least one bowel movement per day, which is well-formed and easy to pass.
The Bristol Stool Chart is a helpful visual that I like to use to rate the health of one’s stool formations:
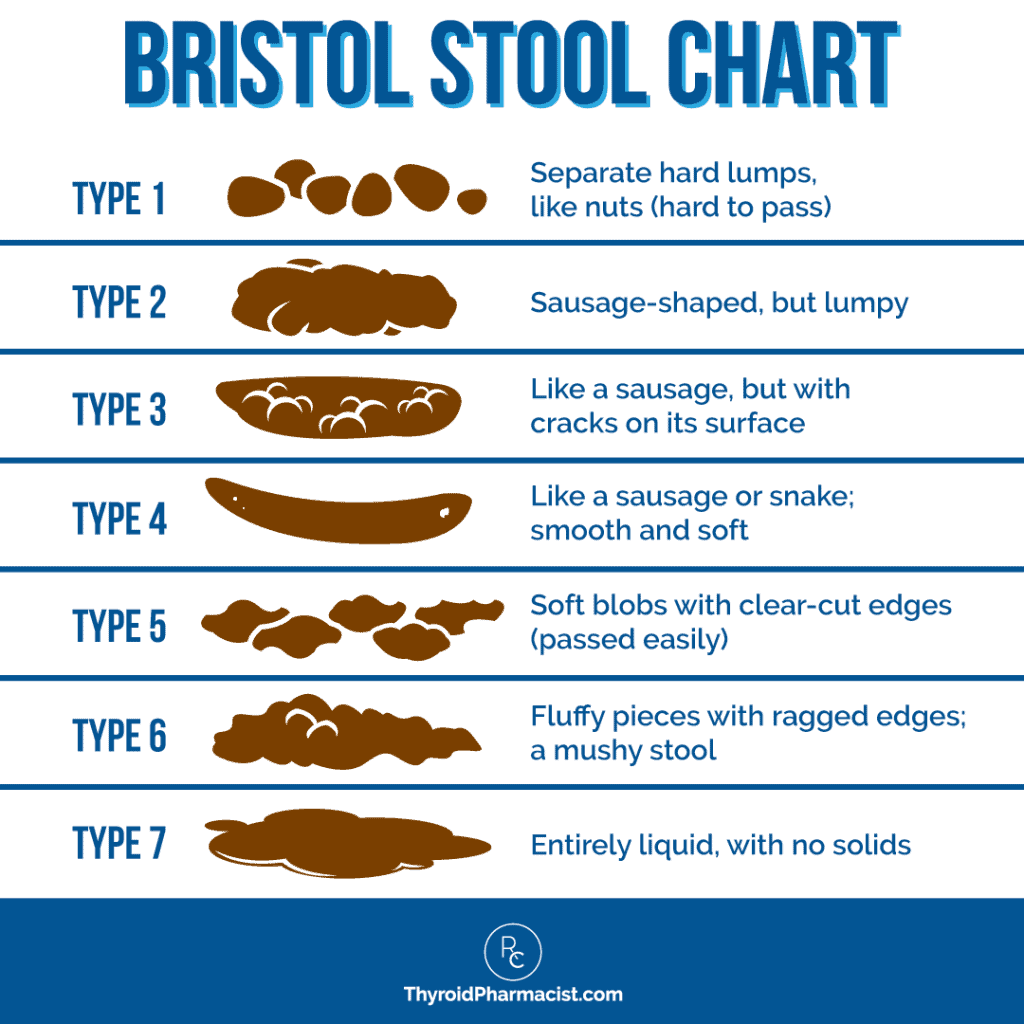
Type 4 is the ideal stool type (type 3 is well-formed as well, but may suggest dehydration), whereas types 2 and 1 suggest an increasing degree of constipation.
About 16 percent of adults experience constipation, and that number increases to 33.5 percent in adults aged 60 to 101. Prevalence is also higher in women and minorities. [3] Someone may be at risk for constipation due to factors such as lower levels of physical activity, depression, stress, and/or a history of abuse.
The Hashimoto’s and Constipation Connection
Thyroid hormones affect every cell in the body — and with hypothyroidism, a slowing-down effect is produced that can affect all body systems. [4] When it comes to digestion, this means that a hypothyroid state can slow digestive motility and transit time (the time it takes for food to move completely through the digestive system), causing constipation. [5] In fact, constipation is one of the most common symptoms that I see with my clients who have Hashimoto’s, though people don’t often bring it up.
Hypothyroidism slows down gut motility by disrupting the normal movement of the intestines, a process called peristalsis. [6] Peristalsis is a wave-like movement (composed of alternating contraction and relaxation motions) occurring in the intestinal muscles that pushes waste through the gut. [7] Similar to other movements, peristalsis requires energy (as well as an optimal balance of nutrients). In the case of hypothyroidism, there isn’t enough energy for peristalsis to occur, leading to slowed transit time. [8]
When transit time is slowed (when stool takes more than 24 hours to be excreted), the harmful bacteria contained in the stool stay in the intestines longer, which can lead to bacterial overgrowth; this further contributes to constipation. [9]
Additionally, constipation can be associated with an “official diagnosis” of constipation-predominant IBS (IBS-C). [10] There’s a big overlap in IBS and Hashimoto’s, and I have found that the two conditions often have underlying root causes.
One 2018 study found that among 80 people with IBS, 19 percent had undiagnosed thyroid dysfunction. [11] It also has been reported that more than half of people with hypothyroidism have small intestinal bacterial overgrowth (SIBO), a condition that’s also a common root cause of IBS. [12] Constipation can be both a cause and a consequence of SIBO – when food sits too long in the intestines, bacterial overgrowth is more likely to occur.
Optimizing thyroid hormones is an important first step for many in restoring proper bowel movements. However, some people continue to struggle with constipation, even with optimal thyroid hormones.
I’d love to share some additional strategies to help you discover and address potential root causes of your constipation (and oftentimes, addressing the underlying causes of constipation may help other Hashimoto’s symptoms as well as the autoimmune attack on the thyroid).
Why Constipation is Important to Address
Constipation isn’t only important as a complication that co-occurs with conditions such as hypothyroidism and/or IBS — on its own, constipation has negative effects on an individual’s health.
In a healthy individual, waste such as metabolized hormones and bacteria is excreted through stool. [13] When an individual is constipated, this waste is not properly excreted and often re-enters the body through re-circulation. Additionally, having unnecessary bacteria sit around in the intestines for an extended period of time allows for bacterial overgrowth to occur, and this can result in gut dysbiosis and SIBO. [14]
Altogether, this can result in…
- Increased toxins [15]
- Hormonal imbalance [16]
- Inflammation [17]
- Gut dysbiosis [18]
- Low or improper immune function (due to bacterial overgrowth and inflammation) [19]
- Disturbances in organ function [20]
- Skin reactions [21]
Constipation is a reflection of an individual’s gut health and affects the gut’s vital role in hormone balance, mood regulation, and immune health. It is also a reflection of improper digestion, which is why nutrient deficiencies are commonly seen in those who are constipated. [22]
Having regular, healthy bowel movements is incredibly important for our overall health, and it’s something I don’t take lightly when working with clients. Many doctors will just suggest a laxative and move on, but this is a temporary fix that doesn’t get to the root cause of why we’re experiencing constipation in the first place.
Hemorrhoids, a Very Strange Predictor for Hashimoto’s
I wanted to share some random research about hemorrhoids, and how they relate to constipation and Hashimoto’s.
According to a 2020 study, there seems to be a connection between hemorrhoids and Hashimoto’s. [23] In this study, patients with hemorrhoids were deemed to be at an increased risk of Hashimoto’s. More specifically, the risk of developing Hashimoto’s was 2.06 times higher in patients with hemorrhoids than in patients without hemorrhoids, making hemorrhoids a surprising predictor for Hashimoto’s. [24]
This study caught my attention, because I had the worst hemorrhoids a few years before my Hashimoto’s diagnosis!
In pharmacy school, I learned that hemorrhoids can result from a lack of fiber in the diet, constipation and diarrhea, as well as sitting on the toilet for too long. 🙂
It could be that Hashimoto’s may slow down or even speed up digestion, leading to hemorrhoids; I personally believe that they’re driven by dysbiosis and gut infections, which make digesting fiber more difficult. Nonetheless, the hemorrhoid example offers another study supporting the gut-thyroid connection and the need to focus on the gut in healing Hashimoto’s. So let’s focus on the gut!
The Conventional Approach to Addressing Constipation
Before we dive into the root cause approach to addressing constipation, let’s briefly review the conventional ways people address a backlog.
The conventional approach to constipation often involves giving over-the-counter or prescription laxatives that help trigger the movement of the intestinal muscles — the mechanism by which the movement is triggered, depends on the type of laxative:
- Over-the-counter (OTC) laxatives: OTC laxatives, as the name suggests, are laxatives that can be found in pharmacies and drug stores. An OTC can either work as an osmotic, stool softener, or lubricant laxative. [25]
- Osmotic laxatives: Osmotic is a derivative of the word “osmosis,” meaning water — as the name suggests, osmotic laxatives, often given in oral form, encourage the intestinal wall to hold in more water via osmosis, which stretches these muscles and helps trigger a defecation reflex. [26] Miralax is a well-known osmotic laxative.
- Lubricants: These agents, as the name suggests, provide lubrication to the intestines to help stool pass through more easily. [27] Laxative lubricants are typically consumed orally.
- Stool softeners: Stool softeners are a specific type of lubricant. Like osmotic laxatives, stool softeners make use of drawing in water to help the stool pass. Unlike osmotic laxatives, which draw water out of the stool, these agents push water into the stool and soften it, which helps it to move through the colon. [28]
- Suppositories: Suppositories are round- or cone-shaped tablets that are inserted into the rectum. Some suppositories work by softening the stool, others provide lubrication and/or stimulation to promote peristalsis. [29]
- Prescription laxatives: These may be prescribed by your doctor and include: [30]
- Linaclotide: This is often recommended by the American College of Gastroenterology (ACG) for symptomatic improvement in IBS-C patients. This medication stimulates intestinal fluid secretion and increases transit time.
- Plecanatide: This is one of the newest medications for IBS-C that has been approved by the FDA. Plecanatide is recommended by the ACG for overall symptomatic improvement in IBS-C patients.
- Lubiprostone: This medication is often recommended for symptomatic improvement in IBS-C patients. It enhances intestinal fluid secretion, thus aiding in constipation.
- Tenapanor: Tenapanor was approved by the FDA in September of 2019 for IBS-C. It works by reducing the absorption of sodium from the small intestine and colon, resulting in an increase in water secretion into the intestinal lumen, resulting in an increase in bowel movements and a decrease in abdominal pain in patients with IBS-C.
- Tegaserod: This medication was approved for IBS-C in 2002, but removed from the market in 2007 due to an increased risk of cardiovascular events. Later that year, it was made available for use in emergency situations, typically in women under age 65.
While these laxatives and medications can provide relief in some cases, I don’t recommend them as a long-term solution, as they generally do not target and resolve the root cause of an individual’s constipation.
Potential Root Causes of Constipation
There are a number of potential root causes of constipation. Keep in mind that root causes can vary from person to person, and some people may have multiple root causes!
Thyroid Hormone Imbalance
As mentioned above, thyroid hormones influence the digestive system, so any thyroid hormone imbalances can affect digestion and how quickly or slowly food is moving through the digestive tract. [31] Hypothyroidism or Hashimoto’s is most likely to cause constipation (while hyperthyroidism can cause diarrhea).
Diet
What we eat (or don’t eat) has a major impact on digestion. When it comes to constipation, food sensitivities, lack of fiber and prebiotics, or lack of healthy fats could be the culprit. [32] What we drink matters too! Not drinking enough water or a lack of essential electrolytes can also result in dry and hard-to-pass stool. [33] Remember that the way many laxatives work is by pulling water into the digestive system and/or stool.
Nutrient Deficiencies
Certain nutrients play a key role in promoting peristalsis and supporting muscle function in the gut. Magnesium, for instance, helps relax intestinal muscles and draws water into the stool, making it easier to pass. [34] Fiber is essential for stimulating peristalsis and adding bulk to the stool, while electrolytes like potassium and sodium are needed for proper muscle contractions. [35] A deficiency in these nutrients can slow down gut motility, making the stool harder and leading to constipation. Ensuring adequate intake of these nutrients can support regular bowel movements and overall gut health.
Slow GI Motility
Slow GI motility, also known as sluggish digestion, occurs when the muscles of the digestive tract don’t move food through the system as efficiently as they should. This delay in peristalsis can lead to symptoms like bloating, constipation, and discomfort. [36]
Muscle Tone
Low muscle tone in the gut, often tied to mitochondrial dysfunction, can lead to constipation because the muscles in the intestines aren’t able to contract efficiently. Mitochondria provide the energy needed for these muscles to perform peristalsis — the movement that pushes food through the digestive tract. When mitochondrial function is impaired, muscle contractions slow down or become weak, leading to sluggish bowel movements and constipation. [37]
Dysbiosis
Dysbiosis, an imbalance in gut bacteria, can contribute to constipation by disrupting normal gut function. Healthy gut bacteria help break down fiber, produce short-chain fatty acids, and support regular bowel movements. When the balance shifts toward harmful bacteria, it can slow gut motility, increase inflammation, and make the stool harder to pass. [38] Restoring a healthy balance through probiotics, prebiotics, and a fiber-rich diet can help improve gut motility and relieve constipation.
Gut Infections
Speaking of gut infections, one could be at the root of your constipation. H. pylori is a common one I see that can cause constipation, but others may be present and impact your digestion.
SIBO
Small intestinal bacterial overgrowth (SIBO), in particular methane dominant SIBO, sometimes called intestinal methanogen overgrowth (IMO), contributes to constipation by interfering with normal digestion and gut motility. [39] In IMO, excess bacteria in the small intestine produce methane gas, which has been shown to slow peristalsis — the muscular contractions that move food through the digestive tract. This reduced motility causes food and waste to move more slowly, leading to harder stools and constipation. Additionally, IMO can cause nutrient malabsorption, which further disrupts gut function and contributes to digestive symptoms like constipation. Addressing SIBO through appropriate treatment can help restore normal motility and relieve constipation.
Diabetic Neuropathy
Diabetic neuropathy, a common complication of long-term high blood sugar and insulin resistance, can cause constipation. Damage to the nerves in the digestive system may disrupt normal food movement, leading to constipation. [40] Additionally, some diabetes medications can contribute to this issue.
Medications
Did you know that constipation is a side effect of many common medications? While it’s not always possible to change or go off medications, addressing these other root causes is often helpful for medication-induced constipation. Some examples of medications that may cause constipation include:
- Opiates (morphine, for example): When increased consumption of opiates results in constipation, it is referred to as opiate-induced constipation. Opiate-induced constipation occurs due to inhibited peristalsis and hardening of stools. [41]
- Nonsteroidal anti-inflammatory agents (NSAIDs): Common NSAIDs such as ibuprofen, aspirin, and naproxen can result in hard stools and straining during bowel movements. Research has also shown that constipation is one of the most common side effects and the reason many individuals stop taking NSAIDs. [42]
- Tricyclic antidepressants: Tricyclic antidepressants disrupt the normal movement of the intestines (peristalsis) of the GI tract. [43] With slowed peristalsis, movement of stool will slow down, leading to constipation.
- Antihistamines: Antihistamines can bind to and alter the function of histamine receptors in the gut that play a role in digestion and the formation of stools. By altering the function of these receptors, antihistamines can reduce optimal gut function and result in constipation. [44]
- Antihypertensives: Antihypertensives such as clonidine, verapamil, and various ganglionic blockers can reduce the action of a specific type of muscle tissue called smooth muscles. [45] As the intestines are made of smooth muscles, a reduction in the action of these muscles can slow down digestion and cause constipation.
- Chemotherapy agents: Chemotherapy agents can lead to constipation in a variety of ways such as slowing the movements of the intestinal tract or creating inflammation that disrupts digestive function. The chemotherapy agents commonly known to do this include gemcitabine (Gemzar), oxaliplatin (Eloxatin), thalidomide (Contergan), vinblastine (Velban), and vincristine (Oncovin). [46]
- Certain supplements: Supplements such as calcium carbonate can cause constipation — calcium contracts the intestinal muscles, making it harder to pass stool. [47] Iron is another example of a supplement that can lead to constipation, as it is difficult for the digestive system to break down and utilize properly. [48] Too much vitamin D can lead to excessive calcium levels in the blood, which can lead to gastrointestinal issues, including constipation. [49] Vitamin D deficiency is common, and many people supplement with it, but there can be too much of a good thing! Be sure to work with your doctor or practitioner to determine the right supplements and dosages for you.
If you suspect that one of these medications or supplements is at the root of your constipation, speak to your healthcare provider about switching to an alternative.
The good news is that over the years, I’ve learned of many dietary, supplement, and lifestyle interventions that are hugely helpful for constipation — and more importantly, they’re more than a quick fix.
Effective Strategies for Managing Constipation
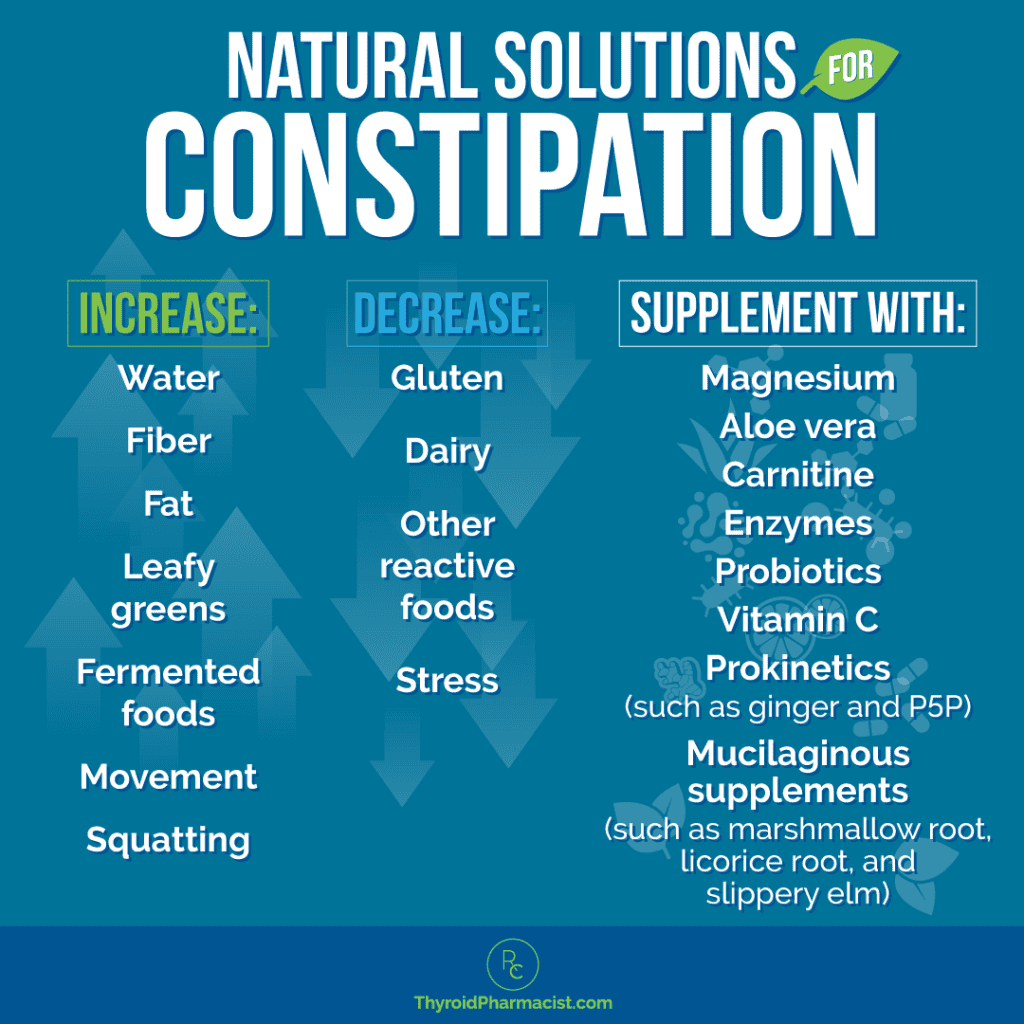
While constipation is common with hypothyroidism, there are many solutions to improve one’s bowel function, beyond conventional laxatives, that work on addressing the underlying root causes of one’s bowel backlog. Not every solution is going to work for everyone — you may need to try several options to see what works best for you. Consider trying a combination of diet, supplement, and lifestyle strategies.
I always recommend trying natural solutions before trying laxatives, as they can be harsh and have GI side effects of their own. Although medication may be helpful initially, it won’t address the root causes of constipation, and you might find yourself developing a dependency instead of healing the underlying factors.
Medications
- Optimize thyroid hormones: As I mentioned earlier, a sluggish thyroid can slow down peristalsis (or contractions in the GI tract), leading to constipation. Optimizing thyroid hormones is a key step in helping to resolve constipation. In my clinical experience, the optimal range for TSH is between 0.5-2 μIU/mL, the optimal T4 reference range is 15-23 pmol/L, and the optimal T3 reference range is 5-7 pmol/L.
If you’re on thyroid medication (and you’ve incorporated the right root cause solutions for you), yet your thyroid hormones are not in the optimal range, it may be time to adjust your thyroid medication or switch to a different type of thyroid medication. Consult with your doctor, and check out my articles on different types of thyroid medications and things to know about thyroid medications for more information.
- Request a medication review with your pharmacist: If you’re experiencing constipation, it’s important to talk to your pharmacist about any medications you’re taking that could be contributing to the issue. Common medications like pain relievers (opioids), certain antidepressants, and antacids containing calcium or aluminum, can slow down gut motility. Your pharmacist can help identify these medications and discuss potential alternatives or adjustments with your healthcare team. Together, they can explore options such as switching to medications with fewer digestive side effects, or adding supplements or strategies to manage constipation effectively while still addressing your other health needs.
- October is Pharmacist Month, a time to celebrate the essential role pharmacists play in healthcare. Pharmacists, especially those trained in Medication Therapy Management (MTM), are highly skilled in optimizing medication use, identifying potential drug interactions, and helping patients manage chronic conditions. MTM-trained pharmacists can work closely with healthcare teams to ensure that medications are safe, effective, and tailored to individual needs, improving overall health outcomes. Take this month to recognize their expertise and the valuable support they provide in patient care!
Dietary Changes
Unsurprisingly, diet has a significant influence on our digestion and whether or not we’re constipated! Here are some of the biggest dietary considerations to improve constipation.
- Proper hydration: Insufficient consumption of water results in our bodies becoming dehydrated. When the intestines are dehydrated, there isn’t enough water to add to the stools, resulting in dry, hard lumps (referred to as type 1 stools in the Bristol Stool Chart). [50]
To determine the precise amount of water your body needs, there is a simple calculation that you can do: you should aim for half your body weight (pounds) in ounces. For example, a 150-pound person would aim to drink 75 ounces of water per day. It’s a good idea to keep track of how much water you’re drinking, either by recording the amount in a handy pocket-sized journal or on your phone. You can also invest in a water bottle that has measurements so you can be sure you’re drinking enough water for you. Lastly, please keep in mind you may need more water if you’re drinking caffeine or engaging in exercise.
Drink warm water first thing in the morning on an empty stomach. This stimulates the gastro-colic reflex in the large intestine. One of my favorite combinations if I’m feeling a little backed up is to add ¼ tsp of sea salt to the water, and consume it along with liquid cod liver or fish oil and a probiotic.
Electrolytes are also helpful for staying hydrated, and may even be helpful for constipation. For example, potassium helps retain water in the stool while magnesium supports muscle relaxation (necessary for bowel movements). Rootcology’s Electrolyte Blend is a great daily electrolyte supplement to help you maximize your hydration.
In addition to water, there are some juices that I have found to be wonderful for aiding in constipation. Because of its high sorbitol (a sugar alcohol) content, pear juice helps to draw water into the stool and soften it, making it easier to pass. [51] Cucumber juice can also be helpful because of its high water content, which hydrates and softens the stool, easing constipation. You can make these at home with a juicer or find them fresh in health food stores or juice bars.
- Increase your fat intake to 50-60 percent of total caloric intake: Adding more high-quality fats to your diet will help increase digestive fluids and increase enzymes needed for nutrient absorption and healthy bowel movements. Fats can be lubricating to the digestive system, and diets too low in fat are associated with constipation. [52] Try increasing your intake of high-quality sources, including olive oil, avocado oil, avocados, coconut oil, nut and seed butters, fatty fish such as salmon, ghee, and eggs, as tolerated.
- Increase your fiber intake: Increasing both soluble and insoluble fiber can play a key role in relieving constipation. [53] Soluble fiber helps by drawing water into the gut, forming a gel-like consistency that soothes the digestive tract and softens stools. You can find soluble fiber in foods like flax seeds, avocado, brussels sprouts, apples, oats, beans, pears, and sweet potatoes. Inulin, a specific type of soluble fiber, also acts as a prebiotic, feeding the healthy bacteria in your gut. [54] It’s found in foods like onions, garlic, leeks, artichokes, chicory root, burdock root, Jerusalem artichokes, and bananas. Inulin supplements can also be helpful.
Insoluble fiber, on the other hand, adds bulk to your stool and helps speed up digestion. [55] Good sources of insoluble fiber include whole grains, apples and pears with their skin, avocado, almonds, walnuts, and berries. Chia seeds are another excellent source; you can add them to water or kombucha for an added probiotic boost. Simply mix in one to two tablespoons of chia seeds and let them sit until they gel up.
In traditional Chinese medicine, hemp butter –- a paste made by blending hemp seeds –- has been used for centuries to support digestion. Hemp seeds are rich in insoluble fiber and healthy fats, making them a great addition to your diet for constipation relief.
However, it’s important to note that increasing fiber may not be tolerated well for those with gut imbalances like SIBO. If you notice a worsening of symptoms when adding more fiber, especially insoluble fiber, you may want to cut back and address underlying gut issues first. Foods rich in insoluble fiber can also be tough on the digestive system when eaten raw, so it’s best to monitor how your body responds.
- Increase your intake of fermented foods: Fermented foods have the power to balance intestinal flora and can improve constipation. [56] Fermented coconut yogurt, fermented coconut water, fermented cabbage (sauerkraut), and beet kvass (a traditional Polish drink) are a few of my favorites. Be sure to get the kind that are kept in the fridge versus the kind that have been canned to be shelf stable, in order to get abundant live cultures. A note of caution — if your constipation is due to SIBO (or small intestinal bacterial overgrowth), you may want to avoid fermented foods, as it can worsen bloat.
- Check for food sensitivities and avoid trigger foods: Food sensitivities can be both a root cause or exacerbating factor for Hashimoto’s, and a root cause for constipation. [57] When you consume a food you are sensitive to, your gut lining can become inflamed which, as noted above, can cause constipation. Over time, this can also contribute to leaky gut, which we know is almost always a factor in the development of autoimmune disease. [58]
According to my survey of over 2000 of my readers, some of the top food sensitivities for those with Hashimoto’s are gluten, dairy, soy, and grains.
Dairy seems to be a common culprit of constipation, so that’s something to consider first. Or, consider a full elimination diet to uncover your individual sensitivities. Additionally, avoid any foods that you know cause constipation for you. If you’re just not sure, you may wish to consider a food sensitivity test, such as the Alletess IgG test.
- Prebiotic Foods: Certain types of fiber are considered prebiotics. Prebiotics are non-digestible components (usually of plants) that feed the good bacteria in the gut. They can help keep a harmonious balance of bacteria in our gut, which can support healthy bowel movements.
Foods rich in prebiotics include chicory root, Jerusalem artichoke, dandelion, garlic, leek, onion, bananas, apples, konjac root, cocoa, burdock root, flax seeds, yacon root, jicama, and asparagus.
- Consider how much caffeine you’re drinking: Many people rely on their morning coffee to help get things moving. This is because caffeine increases contractions in the intestines and helps to move stool forward and out. However, excess caffeine can have a diuretic effect and encourage urination, which can dehydrate the body, resulting in hard stools that are difficult to excrete. [59] If you rely on your morning cup to poop, it may be an indication of choline deficiency. Low levels of choline lead to low levels of acetylcholine, which is needed to trigger contractions in the intestines. Eggs, salmon, beef liver, and chicken liver are all high in choline, and a choline supplement may be helpful as well.
- Increase your intake of potassium-rich foods: Potassium helps retain water in the stool, alleviating constipation. Good food sources of potassium include bananas, avocado, daikon radish, and white root vegetables like potatoes.
- Add anti-inflammatory herbs to your diet: Some root causes of constipation such as high toxins and IBS-C, are associated with increased inflammation in the GI tract, and decreasing this inflammation can be an effective root cause solution for improving constipation. [60]
- Turmeric: One of my favorite anti-inflammatory herbs is turmeric — turmeric has been shown to have anti-inflammatory, antioxidant, antibacterial, and antiviral activity. [61] It is great for detoxifying various inflammatory metals and toxins as well. [62] Curcumin is the main active component of turmeric that lends this herb these benefits. You can read my article on turmeric for more information on this herb.
- Ginger: Whether consumed as a tea, or added to a juice or a meal, ginger may help with motility, relieving both indigestion and constipation. According to a 2015 research review, 100 milligrams of ginger extract may increase bowel movements. [63] Many of the benefits of ginger are due to gingerol and shogaol, compounds called gingeroids, which may also help with bloating, belching, and discomfort after meals. [64]
Lifestyle Solutions
- Squatty Potty: The Squatty Potty is a popular stool that helps you move your stool! 🙂 It fits at the base of the toilet and elevates the feet, putting us into a “squat” position, which has been shown to straighten the colorectal canal and decrease the need to strain with a bowel movement. [65] Proper positioning can make passing a bowel movement easier for someone with constipation. Both globally and historically, squatting has been the primary position used by humans for defecation. I learned the hard way that a squatting toddler in the tub is NOT a good thing! If you’ve ever seen the clever unicorn poop commercials, then you’ve likely heard of this option. 🙂
- Move more: A sedentary lifestyle, in which an individual is sitting for long periods of time, can reduce gut motility, compress the digestive organs of the gut, and reduce the ability to carry out gut functions properly. [66] Moving the body can help to move the bowels. If you are experiencing constipation, I recommend going for regular walks to get your bowels moving. My dog Boomer can attest to this, and if you have a dog, you will certainly know this to be true!
- Stress, sympathetic dominance, and adrenal support: Both short-term and long-term stress can cause changes in gastrointestinal motility, changes in gastrointestinal secretions, an increase in intestinal permeability, negative effects on gastrointestinal mucosa, and negative effects on intestinal microbiota. [67] A stressed state shunts blood away from the digestive system, whereas a relaxed state is optimal for digestion, and can help with constipation.
Sympathetic dominance is when our sympathetic nervous system is consistently activated and cortisol levels are elevated. [68] When we stay in this state for an extended period of time, it can lead to adrenal dysfunction and eventually, low cortisol levels. Both of these states can affect the thyroid and the state of the gut, leading to constipation.
Stress support is crucial for digestion and gut support. My book Adrenal Transformation Protocol is a wonderful resource for learning the best ways to support your body’s stress response. An easy way to start improving your digestion right away is to take 5 to 10 deep breaths before each meal. (Try taking a deep breath now and notice how it calms your nervous system.)
- Listen to your body’s signals: Don’t ignore or delay the urge for a bowel movement; rather, go to the bathroom as soon as you feel the need. The more you ignore your body’s signals to move the bowels, the weaker they become, leading to constipation. [69] Pay close attention to any signals you experience, especially in the hour after eating. This is when your colon is the most active, so it’s the easiest time to have a bowel movement.
- Toilet timing: Our bodies like routines, and when we get out of our usual routines, sometimes we can get a little backed up! Making time to go to the bathroom at the same time every day (such as first thing in the morning, or after meals) trains our migrating motor complex (which moves food through our intestines) that now is the time for a bowel movement. If you’ve ever traveled and been out of your normal routine, you know what I’m talking about. It is so much easier to have normal bowel movements when we are home, making the time to stop for a few minutes and use the bathroom. As often as possible, I recommend making time each day to establish a regular bathroom routine to “train” your system to eliminate.
- Castor oil packs: Castor oil packs are pieces of fabric that have been soaked in castor oil, then applied to specific areas of the body, and secured so that the skin has ample time to absorb the oil. They’ve been used for centuries to support the liver, gallbladder, gut, inflammation, joint pain, PMS, and the thyroid. [70]
Castor oil packs have also been used to treat constipation. By supporting the lymphatic system and stimulating activity of our liver, kidney, gut, and gallbladder, they can encourage gut motility and soften the stool, which makes it a useful remedy for constipation. [71]
Check out my article on castor oil to learn more, as well as learn how to make a castor oil pack at home. Please note: do not ingest the castor oil!
Supplements to Help Resolve Constipation
If I were working with someone with constipation who was already optimized on thyroid hormones, my first recommendation would be to take a magnesium supplement, and this usually helps about 50 percent of the time, without the need for further supplements.
In the case I get someone who is not helped by magnesium, I might recommend prokinetics, aloe, enzymes, or other supportive nutrients or herbs, depending on the suspected cause and additional symptoms that a person might have. Let’s start with magnesium before we get into the additional options.
- Magnesium Citrate: Magnesium citrate is my go-to recommendation for constipation due to its stool-softening properties and calming effect. [72] I suggest taking it before bed to help promote a bowel movement the next morning. A teaspoon of Rootcology Magnesium Citrate is typically a good starting dose, but if you experience loose stools, try reducing the dose or switching to magnesium glycinate (up to 400 mg per day). Magnesium is safe and beneficial, especially since most people are deficient. Not only does it help with constipation, but it also helps sleep, anxiety, and muscle cramps. [73] You can read my full article on magnesium for more information. Note: Keep thyroid medications and magnesium at least four hours apart.
For Suspected Dysbiosis
Dysbiosis is when there is an imbalance of beneficial and pathogenic bacteria in the gut. Studies have shown that those with hypothyroidism have an altered composition of gut bacteria with reduced populations of the beneficial short-chain fatty acid (SCFA)-producing bacteria, and higher levels of inflammation-driving lipopolysaccharides (LPS)-producing bacteria. [74]
To address dysbiosis, we want to start shifting the microbiome in a positive direction by increasing levels of beneficial bacteria, and decreasing levels of pathogenic bacteria. I’ve spoken about probiotics at length, as they can be so helpful for people with Hashimoto’s.
Many years ago, I thought that taking probiotics from the drugstore or eating yogurt would be enough to balance gut microbes, but then I began to learn about how different strains of probiotics have different benefits, and how the dose of the same strain can turn a “maintenance probiotic” into a “therapeutic probiotic.” I also learned (the hard way), that taking the wrong type or dose of probiotics can be disastrous!
People with autoimmunity tend to have lower amounts of the probiotic bacteria Lactobacillus and Bifidus, and higher amounts of the opportunistic E. coli and Proteus bacteria. [75]
I’ve seen this pattern of low levels of probiotic bacteria with high levels of opportunistic bacteria on my own lab tests, as well as on the tests of many clients with Hashimoto’s who have had stool testing to quantify microbial flora.
Fermented foods like sauerkraut, kimchi, and similar fermented vegetables are a wonderful source of beneficial bacteria and can help to restore proper gut flora when consumed regularly.
- Probiotics: In addition to obtaining probiotics from fermented foods, probiotic supplements can also help with constipation for some. [76] It has been shown that decreased levels of Bifidobacterium and Lactobacillus in adults can result in constipation. [77] I’ve found that a deficiency in Bifidobacterium can be addressed really well with a mix of probiotic strains and phages (benevolent viruses) like the kind found in Microphage, which has been shown to boost Bifidobacterium levels tenfold. Soil-based probiotics can also be beneficial for relieving constipation. Read my article about the best types of probiotics for Hashimoto’s for more information on which types can be most helpful, which ones to avoid, guidance, and dosing.
- Inulin: Inulin is a prebiotic soluble fiber that feeds beneficial gut bacteria, supporting a healthy microbiome and regular bowel movements. A daily dose of around 15 g of inulin helps maintain gut health and prevent constipation.
- Aloe vera: Aloe vera has natural laxative properties that can be particularly beneficial for relieving constipation. The outer leaf of the aloe plant contains compounds called anthraquinones, which stimulate bowel movements by increasing intestinal water content, mucus production, and gut motility. [78] This makes the stool softer and easier to pass. Aloe vera also has soothing properties that can reduce inflammation in the digestive tract, making it helpful for those with irritated or inflamed bowels. [79] Additionally, its prebiotic effects support healthy gut bacteria, further promoting regularity. However, it’s important to use aloe vera in moderation, as high doses can lead to cramping or diarrhea. The added bonus is that aloe vera can also reduce thyroid antibodies and improve thyroid hormones in those with Hashimoto’s. [80] You can read more in my article on aloe vera.
- Butyrate: Butyrate is a short-chain fatty acid that provides a number of health benefits to humans. It’s produced when the gut bacteria break down fiber, and prebiotics in particular help stimulate the production of butyrate. Butyrate protects the intestinal barrier and supports proper intestinal permeability, reduces inflammation in the gut, and even has other benefits like supporting brain health, increasing insulin sensitivity, and improving mitochondrial function. [81] It’s also available as a supplement.
- Resistant starch: Resistant starch is a type of carbohydrate that resists digestion in the small intestine and ferments in the large intestine, where it acts as a prebiotic to feed beneficial gut bacteria. This fermentation process produces short-chain fatty acids, such as butyrate, which help improve gut health and promote regular bowel movements. Resistant starch can increase stool bulk and soften stools, making them easier to pass, while also supporting the overall health of the digestive system. Good sources of resistant starch include green bananas, cooked and cooled potatoes, and legumes. Additionally, supplements like Rootcology Paleo Starch offer a convenient way to incorporate resistant starch into your diet. For individuals struggling with constipation, adding resistant starch can enhance gut motility, reduce inflammation, and support a healthy gut microbiome, making it an effective tool for relieving constipation naturally.
For Suspected Motility Issues
Slow GI motility, or delayed movement of food through the digestive tract, can be caused by several factors. Hypothyroidism is a common culprit, as low thyroid hormone levels slow down metabolism and gut function. Mitochondrial dysfunction, which impacts energy production in cells, can also weaken the muscles responsible for peristalsis. Chronic stress and elevated cortisol levels disrupt gut motility by altering the gut-brain axis. Additionally, imbalances in gut bacteria (dysbiosis), nutrient deficiencies (like magnesium or thiamine), and conditions like SIBO or IBS, can all contribute to sluggish digestion. Addressing these root causes can help restore normal motility and improve digestive health.
The following supplements may also be helpful:
- Prokinetic agents: These types of drugs or supplements enhance gut motility by increasing the strength or frequency of contractions. [82] Many of them do so by helping the gut to communicate with the central nervous system, essentially retraining it to move more efficiently. Prescription prokinetics that are helpful for constipation include low-dose naltrexone and low-dose erythromycin, while Motilpro by Pure Encapsulations and Iberogast can be purchased without a prescription.
There are also supplements and herbs with prokinetic properties. I have found that the most efficient ones are:- Carnitine
- Ginger (as a tea or food)
- P5P (vitamin B6)
- Magnesium citrate
It is interesting to note that serotonin is one of the main neurotransmitters that help with GI motility. [83] P5P and magnesium are cofactors (essential for the production) of serotonin, so taking these nutrients can help the body produce serotonin, which in turn, helps with GI motility. [84]
Besides helping relieve digestive issues and constipation, prokinetics have another important benefit. They stimulate the intestinal tract so that it can move food along effectively and prevent bacteria from “snacking” on the food as it passes. (Gut infections like SIBO thrive on slow motility because it allows the bacteria to feed at leisure on the slow-passing food, and therefore proliferate in the gut.)
- L-Carnitine: Carnitine is a nutrient that I’ve found to often be deficient in those with Hashimoto’s. It can be really helpful for muscle weakness, and that could be why it’s also helpful for constipation. This is because proper muscle tone in the smooth muscles in the gut is needed for peristalsis. When muscle tone is low, these muscles may not work properly to propel waste through the digestive tract, resulting in constipation.
Research involving different populations of patients experiencing constipation has found that many of them are deficient in carnitine. These deficiencies have been linked to abnormal diets, medications, and other issues relating to gastrointestinal health (gut motility issues, lack of hydration). In several studies, supplementation with carnitine was shown to improve constipation challenges. [85]
One small study of 27 patients with carnitine deficiency found that the level of existing carnitine was correlated with the degree of constipation they were experiencing. [86]
- Thiamine: Also known as vitamin B1, thiamine deficiency can impair peristalsis. Elliot Overton, who is an expert on all things thiamine, says, “In the stomach, thiamine deficiency inhibits the release of hydrochloric acid from gastric cells and leads to hypochlorhydria (low stomach acid). The rate of gastric motility and emptying also grinds down to a halt, producing delayed emptying, upper GI bloating, GERD/reflux, and nausea.” [87]
Unfortunately, standard lab tests for thiamine deficiency will not show if someone is mildly deficient — they only screen for severe deficiencies. If you’ve been struggling with fatigue, low stomach acid, carbohydrate intolerance, low blood pressure, and symptoms related to your adrenals, you may have a thiamine deficiency and may benefit from extra B1 intake. (Generally, most people can supplement with thiamine without prior testing.)
Supplements I trust include Benfotiamine by Rootcology and BenfoMax by Pure Encapsulations. I recommend 600 mg per day for most people as a starting point. Thiamine can also be very helpful for thyroid-related fatigue. You can learn more about thiamine in my article.
- Alpha-lipoic acid (ALA): ALA can be a helpful addition when using prokinetics, especially for individuals with diabetes. ALA is known for its antioxidant properties and ability to improve insulin sensitivity, but it also supports nerve health and may help improve gut motility by supporting the nervous system. [88] This can be particularly beneficial in managing slow digestion often seen in diabetic gastroparesis. A typical dose of ALA for digestive support is around 600 mg per day.
For Suspected Digestive Enzyme Deficiencies
Constipation can be the result of not having enough digestive enzymes to break down the food we eat, and low digestive enzymes can be the result of dysbiosis. Adding in the right kinds of digestive enzymes and supporting your body’s own production of them may be helpful for constipation.
- Digestive Enzymes: Many people with Hashimoto’s produce fewer digestive enzymes, leading to poor digestion and constipation. Digestive enzymes help break down food and improve nutrient absorption. I recommend Rootcology’s Pancreatic Enzymes Plus, which aids in the digestion of proteins, carbs, and fats. For those with low stomach acid, adding Betaine HCl can further support digestion, especially if H. pylori or low thyroid function is present. [89] You can read my article on digestive enzymes for more details and dosing.
- Bitters: Rather than replacing enzymes, digestive bitters work by stimulating the production of digestive enzymes throughout the gut. This enhances nutrient absorption, supports digestion, and promotes healthy bowel movements. Bitters stimulate “bitter receptors,” which release enzymes throughout the digestive tract. [90]
Here’s a list of herbs that are commonly used as digestive bitters, which help stimulate digestion and promote healthy bile flow, enzyme production, and gut motility: [91]
- Gentian Root: One of the most potent digestive bitters, gentian root stimulates bile production and supports overall digestive function. [92]
- Dandelion Root: Dandelion root helps stimulate bile production and supports liver detoxification, which aids digestion and nutrient absorption. [93]
- Milk Thistle: Known for its liver-supporting properties, milk thistle also works as a digestive bitter to enhance bile flow and detoxification. [94]
- Artichoke Leaf: Artichoke leaf promotes bile production and improves fat digestion, making it a popular choice for digestive health. [95]
- Burdock Root: Burdock root supports digestion and detoxification by stimulating bile flow and promoting healthy gut bacteria. [96]
- Ginger: Ginger acts as both a warming herb and a mild bitter, helping to stimulate digestive juices and improve motility. [97]
These digestive bitters can be consumed in tinctures, teas, or capsules to support digestion, enhance nutrient absorption, and relieve symptoms like bloating and indigestion. Two herbal bitters formulations that I recommend are:
- Dr. Shade’s Bitters No. 9 – This is a liposomal blend of nine bitter herbs and essential oils that aids in healthy bile flow, supports digestive function and comfort, and contributes to healthy liver and gallbladder function.* (Use code drwentz15 for 15% off your first order.)
- Wellena’s Liver & Digestive Bitters Kit – This thoughtfully crafted kit contains a combination of herbal bitters designed to promote normal bile production and healthy digestion, and support the body’s natural cleansing process, before and after meals.*
For Suspected Intestinal Permeability and Constipation
I’ve been speaking about the thyroid and intestinal permeability connection since 2013, and I’m excited that an endocrinology journal published a 2020 study about intestinal permeability and Hashimoto’s. [98] It’s exciting to see some root causes making it into the mainstream. I remember attending a conference in 2013 and speaking to an endocrinologist about the intestinal permeability and thyroid connection, but he hadn’t seen any of the research published in the endocrinology medical journals. It dawned on me that this could have been because the research was in a gastroenterology journal, and not an endocrinology journal! I hope that one day, every person with Hashimoto’s will be able to walk into any practitioner’s office to get proper treatment that will result in 100 percent symptom elimination as well as a root cause resolution. For now, my goal is to educate my readers… so here it goes!
In intestinal permeability, partially digested food, bacteria, and other toxins are able to pass through the damaged barrier and are freely absorbed into the bloodstream, activating the immune system. When we have intestinal permeability, there is also inflammation in the gut. When the lining of our gut is inflamed, it alters gastrointestinal motility, leading to constipation. [99]
- L-glutamine: In addition to eliminating reactive foods, as mentioned earlier, and incorporating gut-healing foods like bone broth, I often recommend L-glutamine in conjunction with mucilaginous agents. L-glutamine by itself is known to resolve diarrhea; however, in combination with mucilaginous herbs, I’ve seen it help constipation as well.
- Mucilaginous agents: Herbs like marshmallow root, licorice root, and slippery elm have mucilaginous properties, which means they form a soothing gel that coats and protects the digestive tract. This helps reduce inflammation, supports the gut lining, and encourages the growth of beneficial bacteria. [100]
L-glutamine, along with mucilaginous herbs, can be found in various “leaky gut support powders” on the market. Consider Rootcology’s Gut R&R if you are looking for an especially tasty and helpful option for promoting healthy gut function and motility.*
Digging Deeper: Treat Underlying Gut Infections
If you’ve already tried modifying your diet and various lifestyle changes and supplements to no avail, you may need to look into testing for gut infections that could be causing constipation. Common infections in constipation include:
- Helicobacter pylori, or H. pylori: This is a type of bacteria that can infect the stomach lining and neutralize stomach acid, affecting digestion and often contributing to constipation. [101]
- SIBO: SIBO (small intestinal bacterial overgrowth) is another potential Hashimoto’s root cause and contributor to constipation. [102] There are a few different types of SIBO, and each is characterized by the type of bacteria that migrates from the colon to the small intestine. Cases of SIBO caused by methane-producing bacteria are more often associated with the symptom of constipation. [103] Moreover, SIBO can lead to the destruction of digestive enzymes such as lactase (digests dairy) and amylase (digests starch), increasing food intolerances and constipation. [104]
- Protozoa: Protozoal infections, like those caused by parasites such as Blastocystis hominis or Giardia, can disrupt gut function and lead to constipation. [105] These infections trigger inflammation in the gut, which can slow down peristalsis, the wave-like muscle contractions that move food through the digestive tract. When this process slows, it results in sluggish bowel movements and constipation. [106]
In many cases, addressing infections and underlying conditions can greatly improve Hashimoto’s and sometimes even produce complete remission! The best way to test for gut infections is a comprehensive stool test like the GI-MAP, GI Effects, or Gut Zoomer.
Takeaway
If you’ve been diagnosed with Hashimoto’s thyroiditis, you might think that regular or occasional constipation is the least of your worries. However, I can’t stress enough how important healthy digestion is to healing Hashimoto’s.
What I know to be true through my own thyroid journey, and by walking this path with so many of you, is that everything is connected. By healing one area of your body or life, you can heal so much more. It’s incredible to think that healing your digestion can not only relieve constipation, and other uncomfortable GI symptoms, but support thyroid health as well.
There are many strategies to help reduce constipation, and I want you to feel empowered to try one or two simple things that you can begin implementing today to promote whole-body healing. It might be as simple as picking up some magnesium and aloe to add to your daily routine, or getting outside for a walk. Simple, natural strategies can often be some of the most powerful ones.
I wish you well on your healing journey!
P.S. Be sure to sign up to my weekly newsletter to get a free book chapter, recipes, Thyroid Diet Starter Guide and notifications about upcoming events and my latest research. For future updates, be sure to follow us on Facebook, Instagram, TikTok, and Pinterest too!
References
[1] Bharucha AE, Pemberton JH, Loke GR. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;122(1):218-238. doi: 10.1053/j.gastro.2012.10.028.
[2] Lacy BE, Levenick JM, Crowell M. Chronic constipation: new diagnostic and treatment approaches. Therap Adv Gastroenterol. 2012;5(4):233-247. doi:10.1177/1756283X12443093
[3] Bharucha AE, Pemberton JH, Loke GR. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;122(1):218-238. doi: 10.1053/j.gastro.2012.10.028.
[4] Chaker L, Bianco AC, Jonklaas J, Peeters RP. Hypothyroidism. Lancet. 2017;390(10101):1550-1562. doi:10.1016/S0140-6736(17)30703-1
[5] Bharucha AE, Pemberton JH, Loke GR. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;122(1):218-238. doi: 10.1053/j.gastro.2012.10.028.
[6] Yaylali O, Kirac S, Yilmaz M, et al. Does hypothyroidism affect gastrointestinal motility?. Gastroenterol Res Pract. 2009;2009:529802. doi:10.1155/2009/529802
[7] Patel KS, Thavamani A. Physiology, Peristalsis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; January 21, 2022.
[8] Daher R, Yazbeck T, Jaoude JB, Abboud B. Consequences of dysthyroidism on the digestive tract and viscera. World J Gastroenterol. 2009;15(23):2834-2838. doi: 10.3748/wjg.15.2834.
[9] Roager HM, Hansen LB, Bahl MI, et al. Colonic transit time is related to bacterial metabolism and mucosal turnover in the gut. Nat Microbiol. 2016;1(9):16093. Published 2016 Jun 27. doi:10.1038/nmicrobiol.2016.93
[10] Azzo L. Managing Irritable Bowel Syndrome. PharmCon. 2020. Accessed June 6, 2023. Freece.com.; 1. Fidler B. Updates on the Management of Irritable Bowel Syndrome Management. 2018. Accessed June 6, 2023. freece.com.
[11] Bhattacharjee B, Upadhyay S, Ghosh J. Study of the Interrelationship Between Irritable Bowel Syndrome and Hypothyroidism. ResearchGate. April 2023. Accessed September 6, 2024. https://www.researchgate.net/publication/322946988_Prevalence_of_Thyroid_Dysfunction_in_Irritable_Bowel_Syndrome.
[12] Lauritano EC, Bilotta AL, Gabrielli M, et al. Association between hypothyroidism and small intestinal bacterial overgrowth. J Clin Endocrinol Metab. 2007;92(11):4180-4184. doi:10.1210/jc.2007-0606
[13] Adlercreutz H, Järvenpää P. Assay of estrogens in human feces. J Steroid Biochem. 1982;17(6):639-645. doi:10.1016/0022-4731(82)90565-9
[14] Roager HM, Hansen LB, Bahl MI, et al. Colonic transit time is related to bacterial metabolism and mucosal turnover in the gut. Nat Microbiol. 2016;1(9):16093. Published 2016 Jun 27. doi:10.1038/nmicrobiol.2016.93
[15] Ramos CI, Armani RG, Canziani ME, et al. Bowel Habits and the Association With Uremic Toxins in Non-Dialysis-Dependent Chronic Kidney Disease Patients. J Ren Nutr. 2020;30(1):31-35. doi:10.1053/j.jrn.2019.02.004
[16] Wszelaki M. How constipation causes hormonal imbalances and ways to get going again. Hormones & Balance. April 4, 2017. Accessed June 6, 2023. https://hormonesbalance.com/articles/how-constipation- causes-hormonal-imbalances-ways-to-get-going-again/.
[17] Mokhtare M, Alimoradzadeh R, Agah S, Mirmiranpour H, Khodabandehloo N. The Association between Modulating Inflammatory Cytokines and Constipation of Geriatrics in Iran. Middle East J Dig Dis. 2017;9(4):228-234. doi:10.15171/mejdd.2017.78
[18] Peirson E. Gut motility – Driver of the Microbiome. Peirson Center for Children. April 24, 2019. Accessed June 6, 2023. https://www.peirsoncenter.com/articles/gut-motility-driver-of-the-microbiome.
[19] Khalif IL, Quigley EM, Konovitch EA, Maximova ID. Alterations in the colonic flora and intestinal permeability and evidence of immune activation in chronic constipation. Dig Liver Dis. 2005;37(11):838-849. doi:10.1016/j.dld.2005.06.008
[20] Kalaitzakis E. Gastrointestinal dysfunction in liver cirrhosis. World J Gastroenterol. 2014;20(40):14686-14695. doi:10.3748/wjg.v20.i40.14686; Sumida K, Molnar MZ, Potukuchi PK, et al. Constipation and Incident CKD. J Am Soc Nephrol. 2017;28(4):1248-1258. doi:10.1681/ASN.2016060656
[21] Huang YC, Wu MC, Wang YH, Wei JC. Influence of constipation on atopic dermatitis: A nationwide population-based cohort study in Taiwan. Int J Clin Pract. 2021;75(3):e13691. doi:10.1111/ijcp.13691
[22] Panarese A, Pesce F, Porcelli P, et al. Chronic functional constipation is strongly linked to vitamin D deficiency. World J Gastroenterol. 2019;25(14):1729-1740. doi:10.3748/wjg.v25.i14.1729
[23] Hsu SP, Chen HH, Wang TY, et al. Association of Hemorrhoids With Hashimoto’s Thyroiditis and Associated Comorbidities: A Nationwide Population-Based Cohort Study. Front Endocrinol (Lausanne). 2020;11:577767. Published 2020 Oct 8. doi:10.3389/fendo.2020.577767
[24] Ibid
[25] Rao SSC, Brenner DM. Efficacy and Safety of Over-the-Counter Therapies for Chronic Constipation: An Updated Systematic Review. Am J Gastroenterol. 2021;116(6):1156-1181. doi:10.14309/ajg.0000000000001222
[26] Ibid
[27] Sondheimer JM, Gervaise EP. Lubricant versus laxative in the treatment of chronic functional constipation of children: a comparative study. J Pediatr Gastroenterol Nutr. 1982;1(2):223-226. doi:10.1097/00005176-198201020-00012
[28] Treatments for Constipation: A Review of Systematic Reviews. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; November 17, 2014.
[29] Lazzaroni M, Casini V, Bianchi Porro G. Role or carbon dioxide-releasing suppositories in the treatment of chronic functional constipation: a double-blind, randomised, placebo-controlled trial. Clin Drug Investig. 2005;25(8):499-505. doi:10.2165/00044011-200525080-00002
[30] Azzo L. Managing Irritable Bowel Syndrome. PharmCon. 2020. Accessed June 6, 2023. Freece.com.; 3. Fidler B. Updates on the Management of Irritable Bowel Syndrome Management. 2018. Accessed June 6, 2023. freece.com.
[31] Pustorino S, Foti M, Calipari G, et al. Interazioni funzionali tra tiroide e motilità gastrointestinale [Thyroid-intestinal motility interactions summary]. Minerva Gastroenterol Dietol. 2004;50(4):305-315.
[32] Rollet M, Bohn T, Vahid F, On Behalf Of The Oriscav Working Group. Association between Dietary Factors and Constipation in Adults Living in Luxembourg and Taking Part in the ORISCAV-LUX 2 Survey. Nutrients. 2021 Dec 28;14(1):122. doi: 10.3390/nu14010122. PMID: 35010999; PMCID: PMC8746799.
[33] Yurtdaş G, Acar-Tek N, Akbulut G, et al. Risk Factors for Constipation in Adults: A Cross-Sectional Study. J Am Coll Nutr. 2020;39(8):713-719. doi:10.1080/07315724.2020.1727380
[34] Mori H, Tack J, Suzuki H. Magnesium Oxide in Constipation. Nutrients. 2021 Jan 28;13(2):421. doi: 10.3390/nu13020421. PMID: 33525523; PMCID: PMC7911806.
[35] Ioniță-Mîndrican CB, Ziani K, Mititelu M, Oprea E, Neacșu SM, Moroșan E, Dumitrescu DE, Roșca AC, Drăgănescu D, Negrei C. Therapeutic Benefits and Dietary Restrictions of Fiber Intake: A State of the Art Review. Nutrients. 2022 Jun 26;14(13):2641. doi: 10.3390/nu14132641. PMID: 35807822; PMCID: PMC9268622.; Shrimanker I, Bhattarai S. Electrolytes. StatPearls. July 24, 2023. Accessed September 17, 2024. https://www.ncbi.nlm.nih.gov/books/NBK541123/.
[36] Patel KS, Thavamani A. Physiology, Peristalsis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; March 12, 2023.
[37] Mosiello G, Safder S, Marshall D, Rolle U, Benninga MA. Neurogenic Bowel Dysfunction in Children and Adolescents. J Clin Med. 2021;10(8):1669. Published 2021 Apr 13. doi:10.3390/jcm10081669; Chen TH, Koh KY, Lin KM, Chou CK. Mitochondrial Dysfunction as an Underlying Cause of Skeletal Muscle Disorders. Int J Mol Sci. 2022;23(21):12926. Published 2022 Oct 26. doi:10.3390/ijms232112926
[38] Ohkusa T, Koido S, Nishikawa Y, Sato N. Gut Microbiota and Chronic Constipation: A Review and Update. Front Med (Lausanne). 2019;6:19. Published 2019 Feb 12. doi:10.3389/fmed.2019.00019
[39] Skrzydło-Radomańska B, Cukrowska B. How to Recognize and Treat Small Intestinal Bacterial Overgrowth?. J Clin Med. 2022;11(20):6017. Published 2022 Oct 12. doi:10.3390/jcm11206017
[40] Azpiroz F, Malagelada C. Diabetic neuropathy in the gut: pathogenesis and diagnosis. Diabetologia. 2016;59(3):404-408. doi:10.1007/s00125-015-3831-1
[41] Sizar O, Genova R, Gupta M. Opioid Induced Constipation. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 20, 2022.
[42] Jones RH, Tait CL. Gastrointestinal side-effects of NSAIDs in the community. Br J Clin Pract. 1995;49(2):67-70.
[43] Jeong B, Sung TS, Jeon D, et al. Inhibition of TRPC4 channel activity in colonic myocytes by tricyclic antidepressants disrupts colonic motility causing constipation. J Cell Mol Med. 2022;26(19):4911-4923. doi:10.1111/jcmm.17348
[44] Patel RH, Mohiuddin SS. Biochemistry, Histamine. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 1, 2023.
[45] Ahn Y, Nam MH, Kim E. Relationship Between the Gastrointestinal Side Effects of an Anti-Hypertensive Medication and Changes in the Serum Lipid Metabolome. Nutrients. 2020;12(1):205. Published 2020 Jan 13. doi:10.3390/nu12010205
[46] McQuade RM, Stojanovska V, Abalo R, Bornstein JC, Nurgali K. Chemotherapy-Induced Constipation and Diarrhea: Pathophysiology, Current and Emerging Treatments. Front Pharmacol. 2016;7:414. Published 2016 Nov 3. doi:10.3389/fphar.2016.00414
[47] Li K, Wang XF, Li DY, et al. The good, the bad, and the ugly of calcium supplementation: a review of calcium intake on human health. Clin Interv Aging. 2018;13:2443-2452. Published 2018 Nov 28. doi:10.2147/CIA.S157523
[48] Poveda C, Pereira DIA, Lewis M, Walton GE. The Impact of Low-Level Iron Supplements on the Faecal Microbiota of Irritable Bowel Syndrome and Healthy Donors Using In Vitro Batch Cultures. Nutrients. 2020;12(12):3819. Published 2020 Dec 14. doi:10.3390/nu12123819
[49] Tebben PJ, Singh RJ, Kumar R. Vitamin D-Mediated Hypercalcemia: Mechanisms, Diagnosis, and Treatment. Endocr Rev. 2016;37(5):521-547. doi:10.1210/er.2016-1070; 1. Conquering Constipation – An SAFM Mini Clinical Course. The School of Applied Functional Medicine. Accessed June 6, 2023. https://schoolafm.com/.
[50] Arnaud MJ. Mild dehydration: a risk factor of constipation?. Eur J Clin Nutr. 2003;57 Suppl 2:S88-S95. doi:10.1038/sj.ejcn.1601907
[51] Stumm RE, Thomas MS, Coombes JA, Greenhill J, Hay J. Managing constipation in elderly orthopaedic patients using either pear juice or a high fibre supplement. ResearchGate. https://www.researchgate.net/ publication/ 281366998_Managing _constipation_in_elderly_orthopaedic_patients_using_either_pear_ juice_or_a_high_fibre_supplement. Published January 2001. Accessed September 22, 2022.
[52] Rollet M, Bohn T, Vahid F, On Behalf Of The Oriscav Working Group. Association between Dietary Factors and Constipation in Adults Living in Luxembourg and Taking Part in the ORISCAV-LUX 2 Survey. Nutrients. 2021;14(1):122. Published 2021 Dec 28. doi:10.3390/nu14010122
[53] Kaczmarczyk MM, Miller MJ, Freund GG. The health benefits of dietary fiber: beyond the usual suspects of type 2 diabetes mellitus, cardiovascular disease and colon cancer. Metabolism. 2012;61(8):1058-1066. doi:10.1016/j.metabol.2012.01.017
[54] Shoaib M, Shehzad A, Omar M, et al. Inulin: Properties, health benefits and food applications. Carbohydr Polym. 2016;147:444-454. doi:10.1016/j.carbpol.2016.04.020
[55] Erdogan A, Rao SS, Thiruvaiyaru D, et al. Randomised clinical trial: mixed soluble/insoluble fibre vs. psyllium for chronic constipation. Aliment Pharmacol Ther. 2016;44(1):35-44. doi:10.1111/apt.13647
[56] Chen M, Ye X, Shen D, Ma C. Modulatory Effects of Gut Microbiota on Constipation: The Commercial Beverage Yakult Shapes Stool Consistency. J Neurogastroenterol Motil. 2019;25(3):475-477. doi:10.5056/jnm19048
[57] Coucke F. Food intolerance in patients with manifest autoimmunity. Observational study. Autoimmun Rev. 2018;17(11):1078-1080. doi:10.1016/j.autrev.2018.05.011; Carroccio A, Scalici C, Maresi E, et al. Chronic constipation and food intolerance: a model of proctitis causing constipation. Scand J Gastroenterol. 2005;40(1):33-42. doi:10.1080/00365520410009401
[58] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
[59] Lohsiriwat S, Hirunsai M, Chaiyaprasithi B. Effect of caffeine on bladder function in patients with overactive bladder symptoms. Urol Ann. 2011;3(1):14-18. doi:10.4103/0974-7796.75862
[60] Miller C, Emmanuel A, Zarate-Lopez N, Taylor S, Bloom S. Constipation in ulcerative colitis: pathophysiology and practical management. Frontline Gastroenterol. 2020;12(6):493-499. Published 2020 Aug 26. doi:10.1136/flgastro-2020-101566
[61] Adamczak A, Ożarowski M, Karpiński TM. Curcumin, a Natural Antimicrobial Agent with Strain-Specific Activity. Pharmaceuticals (Basel). 2020;13(7):153. Published 2020 Jul 16. doi:10.3390/ph13070153
[62] García-Niño WR, Pedraza-Chaverrí J. Protective effect of curcumin against heavy metals-induced liver damage. Food Chem Toxicol. 2014;69:182-201. doi:10.1016/j.fct.2014.04.016
[63] Giacosa A, Morazzoni P, Bombardelli E, Riva A, Bianchi Porro G, Rondanelli M. Can nausea and vomiting be treated with ginger extract? Eur Rev Med Pharmacol Sci. 2015;19(7):1291-1296
[64] Nikkhah Bodagh M, Maleki I, Hekmatdoost A. Ginger in gastrointestinal disorders: A systematic review of clinical trials. Food Sci Nutr. 2018;7(1):96-108. Published 2018 Nov 5. doi:10.1002/fsn3.807; Hu ML, Rayner CK, Wu KL, et al. Effect of ginger on gastric motility and symptoms of functional dyspepsia. World J Gastroenterol. 2011;17(1):105-110. doi:10.3748/wjg.v17.i1.105
[65] Modi RM, Hinton A, Pinkhas D, et al. Implementation of a Defecation Posture Modification Device: Impact on Bowel Movement Patterns in Healthy Subjects. J Clin Gastroenterol. 2019;53(3):216-219. doi:10.1097/MCG.0000000000001143
[66] Huang R, Ho SY, Lo WS, Lam TH. Physical activity and constipation in Hong Kong adolescents. PLoS One. 2014;9(2):e90193. Published 2014 Feb 28. doi:10.1371/journal.pone.0090193
[67] Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011;62(6):591-599.
[68] Conquering Constipation – An SAFM Mini Clinical Course. The School of Applied Functional Medicine. Accessed June 6, 2023. https://schoolafm.com/.
[69] Concerned about constipation? National Institute on Aging. https://www.nia.nih.gov/health/concerned- about-constipation. Published December 2013. Accessed September 16, 2022.
[70] Kennedy DA, Keaton D. Evidence for the Topical Application of Castor Oil. Int J Naturo Med. https://intjnm.com/evidence-for-the-topical-application-of-castor-oil/. Published March 13, 2012. Accessed September 16, 2022.
[71] Arslan GG, Eşer I. An examination of the effect of castor oil packs on constipation in the elderly. Complement Ther Clin Pract. 2011;17(1):58-62. doi:10.1016/j.ctcp.2010.04.004
[72]Schwalfenberg GK, Genuis SJ. The Importance of Magnesium in Clinical Healthcare. Scientifica (Cairo). 2017;2017:4179326. doi:10.1155/2017/4179326; Potter JD, Robertson SP, Johnson JD. Magnesium and the regulation of muscle contraction. Fed Proc. 1981;40(12):2653-2656.; Rao SSC, Brenner DM. Efficacy and Safety of Over-the-Counter Therapies for Chronic Constipation: An Updated Systematic Review. Am J Gastroenterol. 2021;116(6):1156-1181.
[73] Al Alawi AM, Majoni SW, Falhammar H. Magnesium and Human Health: Perspectives and Research Directions. Int J Endocrinol. 2018;2018:9041694. Published 2018 Apr 16. doi:10.1155/2018/9041694
[74] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
[75] De Luca F, Shoenfeld Y. The microbiome in autoimmune diseases. Clin Exp Immunol. 2019;195(1):74-85. doi:10.1111/cei.13158
[76] Yoon JY, Cha JM, Oh JK, et al. Probiotics Ameliorate Stool Consistency in Patients with Chronic Constipation: A Randomized, Double-Blind, Placebo-Controlled Study. Dig Dis Sci. 2018;63(10):2754-2764. doi:10.1007/s10620-018-5139-8
[77] Mitelmão FCR, Bergamaschi CC, Gerenutti M, et al. The effect of probiotics on functional constipation in adults: Double-blind, randomized, placebo-controlled study. Medicine (Baltimore). 2021;100(10):e24938. doi:10.1097/MD.0000000000024938
[78] Hong SW, Chun J, Park S, Lee HJ, Im JP, Kim JS. Aloe vera Is Effective and Safe in Short-term Treatment of Irritable Bowel Syndrome: A Systematic Review and Meta-analysis. J Neurogastroenterol Motil. 2018;24(4):528-535. doi:10.5056/jnm18077
[79]Ibid
[80] Metro D, Cernaro V, Papa M, Benvenga S. Marked improvement of thyroid function and autoimmunity by Aloe barbadensis miller juice in patients with subclinical hypothyroidism. J Clin Transl Endocrinol. 2018;11:18-25. Published 2018 Feb 14. doi:10.1016/j.jcte.2018.01.003
[81] Siddiqui MT, Cresci GAM. The Immunomodulatory Functions of Butyrate. J Inflamm Res. 2021;14:6025-6041. Published 2021 Nov 18. doi:10.2147/JIR.S300989; Ahmad MS, Krishnan S, Ramakrishna BS, Mathan M, Pulimood AB, Murthy SN. Butyrate and glucose metabolism by colonocytes in experimental colitis in mice. Gut. 2000;46(4):493-499. doi:10.1136/gut.46.4.493; Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. Published 2020 Jan 31. doi:10.3389/fendo.2020.00025; Yagi A, Al-Madboly L, Kabbash A, El-Aasr M. Dietary Aloe vera gel and Microbiota Interactions: Influence of Butyrate and Insulin Sensitivity. J of Gastroenterol Hepatol. 2017; 6(4): 2376-2383; Zhang J, Song L, Wang Y, et al. Beneficial effect of butyrate-producing Lachnospiraceae on stress-induced visceral hypersensitivity in rats. J Gastroenterol Hepatol. 2019;34(8):1368-1376. doi:10.1111/jgh.14536
[82] Quigley EM. Prokinetics in the Management of Functional Gastrointestinal Disorders. J Neurogastroenterol Motil. 2015;21(3):330-336. doi:10.5056/jnm15094
[83] Camilleri M. Serotonin in the gastrointestinal tract. Curr Opin Endocrinol Diabetes Obes. 2009;16(1):53-59. doi:10.1097/med.0b013e32831e9c8e
[84] Allen GF, Neergheen V, Oppenheim M, et al. Pyridoxal 5′-phosphate deficiency causes a loss of aromatic L-amino acid decarboxylase in patients and human neuroblastoma cells, implications for aromatic L-amino acid decarboxylase and vitamin B(6) deficiency states. J Neurochem. 2010;114(1):87-96. doi:10.1111/j.1471-4159.2010.06742.x; Schwalfenberg GK, Genuis SJ. The Importance of Magnesium in Clinical Healthcare. Scientifica (Cairo). 2017;2017:4179326. doi:10.1155/2017/4179326
[85] Murata S, Inoue K, Aomatsu T, Yoden A, Tamai H. Supplementation with carnitine reduces the severity of constipation: a retrospective study of patients with severe motor and intellectual disabilities. J Clin Biochem Nutr. 2017;60(2):121–124; Irie J, Kanno Y, Kikuchi R, et al. L-Carnitine improves gastrointestinal disorders and altered the intestinal microbiota in hemodialysis patients. Biosci Microbiota Food Health. 2017;36(1):11-16.
[86] Murata S, Inoue K, Aomatsu T, Yoden A, Tamai H. Supplementation with carnitine reduces the severity of constipation: a retrospective study of patients with severe motor and intellectual disabilities. J Clin Biochem Nutr. 2017;60(2):121-124. doi:10.3164/jcbn.16-52
[87] Overton E. When SIBO & IBS-Constipation are just unrecognized thiamine deficiency. Elliot Overton Nutrition & Functional Medicine. October 28, 2020. Accessed June 6, 2023. https://www.eonutrition.co.uk/ post/when-sibo-ibs-constipation-are-just-unrecognized-thiamine-deficiency
[88] Salehi B, Berkay Yılmaz Y, Antika G, et al. Insights on the Use of α-Lipoic Acid for Therapeutic Purposes. Biomolecules. 2019;9(8):356. Published 2019 Aug 9. doi:10.3390/biom9080356
[89] Guilliams TG, Drake LE. Meal-Time Supplementation with Betaine HCl for Functional Hypochlorhydria: What is the Evidence?. Integr Med (Encinitas). 2020;19(1):32-36.
[90] McMullen MK, Whitehouse JM, Towell A. Bitters: Time for a New Paradigm. Evid Based Complement Alternat Med. 2015;2015:670504. doi:10.1155/2015/670504
[91] Ibid
[92]Ibid
[93] Fan M, Zhang X, Song H, Zhang Y. Dandelion (Taraxacum Genus): A Review of Chemical Constituents and Pharmacological Effects. Molecules. 2023;28(13):5022. Published 2023 Jun 27. doi:10.3390/molecules28135022
[94] Khazaei R, Seidavi A, Bouyeh M. A review on the mechanisms of the effect of silymarin in milk thistle (Silybum marianum) on some laboratory animals. Vet Med Sci. 2022;8(1):289-301. doi:10.1002/vms3.641
[95] Ben Salem M, Affes H, Ksouda K, et al. Pharmacological Studies of Artichoke Leaf Extract and Their Health Benefits. Plant Foods Hum Nutr. 2015;70(4):441-453. doi:10.1007/s11130-015-0503-8
[96] Watanabe A, Sasaki H, Miyakawa H, Nakayama Y, Lyu Y, Shibata S. Effect of Dose and Timing of Burdock (Arctium lappa) Root Intake on Intestinal Microbiota of Mice. Microorganisms. 2020;8(2):220. Published 2020 Feb 6. doi:10.3390/microorganisms8020220
[97] Nikkhah Bodagh M, Maleki I, Hekmatdoost A. Ginger in gastrointestinal disorders: A systematic review of clinical trials. Food Sci Nutr. 2018;7(1):96-108. Published 2018 Nov 5. doi:10.1002/fsn3.807
[98] Küçükemre Aydın B, Yıldız M, Akgün A, Topal N, Adal E, Önal H. Children with Hashimoto’s Thyroiditis Have Increased Intestinal Permeability: Results of a Pilot Study. J Clin Res Pediatr Endocrinol. 2020;12(3):303-307. doi:10.4274/jcrpe.galenos.2020.2019.0186
[99] Bassotti G, Antonelli E, Villanacci V, et al. Abnormal gut motility in inflammatory bowel disease: an update. Tech Coloproctol. 2020;24(4):275-282. doi:10.1007/s10151-020-02168-y; Pathmakanthan S, Hawkey CJ. A lay doctor’s guide to the inflammatory process in the gastrointestinal tract. Postgrad Med J. 2000;76(900):611-617. doi:10.1136/pmj.76.900.611
[100] Kassem IAA, Joshua Ashaolu T, Kamel R, Elkasabgy NA, Afifi SM, Farag MA. Mucilage as a functional food hydrocolloid: ongoing and potential applications in prebiotics and nutraceuticals. Food Funct. 2021;12(11):4738-4748. doi:10.1039/d1fo00438g
[101] Murata M, Sugimoto M, Miyamoto S, Kawai T. Long-term improvement in constipation-related symptoms after Helicobacter pylori eradication therapy. Helicobacter. 2022;27(1):e12863. doi:10.1111/hel.12863
[102] Patil AD. Link between hypothyroidism and small intestinal bacterial overgrowth. Indian J Endocrinol Metab. 2014;18(3):307-309. doi:10.4103/2230-8210.131155
[103] Bin Waqar SH, Rehan A. Methane and Constipation-predominant Irritable Bowel Syndrome: Entwining Pillars of Emerging Neurogastroenterology. Cureus. 2019;11(5):e4764. Published 2019 May 28. doi:10.7759/cureus.4764
[104] Sorathia SJ, Chippa V, Rivas JM. Small Intestinal Bacterial Overgrowth. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 5, 2022.
[105] Boorom KF, Smith H, Nimri L, et al. Oh my aching gut: irritable bowel syndrome, Blastocystis, and asymptomatic infection. Parasit Vectors. 2008;1(1):40. Published 2008 Oct 21. doi:10.1186/1756-3305-1-40
[106] Jadallah KA, Nimri LF, Ghanem RA. Protozoan parasites in irritable bowel syndrome: A case-control study. World J Gastrointest Pharmacol Ther. 2017;8(4):201-207. doi:10.4292/wjgpt.v8.i4.201


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Leave a Reply