Every now and then, I get a message from someone who says, “Help! I don’t know what to do! My TSH is low, but so are my levels of T4 and T3 thyroid hormones! Does this mean that I need more or less thyroid medication?”
If you understand thyroid physiology, you know that this is a very unusual situation. This is because in the presence of low levels of T4 and T3 thyroid hormones, the pituitary begins to secrete more TSH (thyroid stimulating hormone) in an effort to get the thyroid gland to produce more thyroid hormone.
Thus, in “normal” thyroid physiology, whenever there is a low level of T4 and/or T3, one’s TSH level shoots up. In contrast, when there is too much T4/T3, one’s TSH level drops.
An elevated TSH in the presence of low or normal T4/T3 is usually due to hypothyroidism or subclinical hypothyroidism, respectively. When TSH is suppressed, and T4/T3 is elevated or normal, this is usually due to hyperthyroidism or subclinical hyperthyroidism, respectively. These conditions are known as primary hypothyroidism and hyperthyroidism, respectively, as they are primarily thought to originate due to the dysfunction of the thyroid gland.
Thus, a low TSH in the presence of normal or low T4/T3 levels can leave patients and doctors baffled — and this, as you may have guessed by the title of this article , is known as central hypothyroidism (sometimes called pituitary hypothyroidism or secondary hypothyroidism – I’ll explain why in this article).
I have personally experienced central hypothyroidism three times.
The first time was while I was taking Armour® Thyroid (a natural desiccated thyroid medication) and began taking adrenal glandulars to support my adrenals and stress response.
I was still experiencing a variety of symptoms at the time, but was unaware of what symptoms might be indicators of central hypothyroidism. I only learned that I had central hypothyroidism as a result of a routine blood test (being a human guinea pig, I tested my thyroid function at least every other month for the first few years after diagnosis).
Because many people may experience it, even as a transient condition, I wanted to write this article to share some thoughts on what may be behind central hypothyroidism, what it looks like, and how to approach treatment.
In this article, you will learn:
- What central hypothyroidism is and what its symptoms may look like
- What labs best identify central hypothyroidism
- Common causes and conventional treatment for the condition
- Why central hypothyroidism is more common in those with Hashimoto’s
- The treatment protocol I recommend for central hypothyroidism
What is Central Hypothyroidism?
Most people who have hypothyroidism have what is referred to as primary hypothyroidism. [1]
This is hypothyroidism due to thyroid hormone deficiencies brought on by the failure of the thyroid gland. The vast majority of people with primary hypothyroidism also have Hashimoto’s, an autoimmune disease where the body attacks and damages the thyroid, causing thyroid hormone deficiencies.
Central hypothyroidism also results in thyroid hormone deficiencies and related symptoms, but the cause is a disorder of pituitary or hypothalamus hormone production (versus failure of the thyroid gland itself).
When the pituitary is the cause of central hypothyroidism, the condition is referred to as secondary hypothyroidism, or pituitary central hypothyroidism. If the hypothalamus (a region of the brain that controls your endocrine system) is the cause, your doctor may refer to your central hypothyroidism as “tertiary hypothyroidism”.
What Causes Central Hypothyroidism?
In simple terms, a communication breakdown between the hypothalamus and pituitary gland can lead to central hypothyroidism.
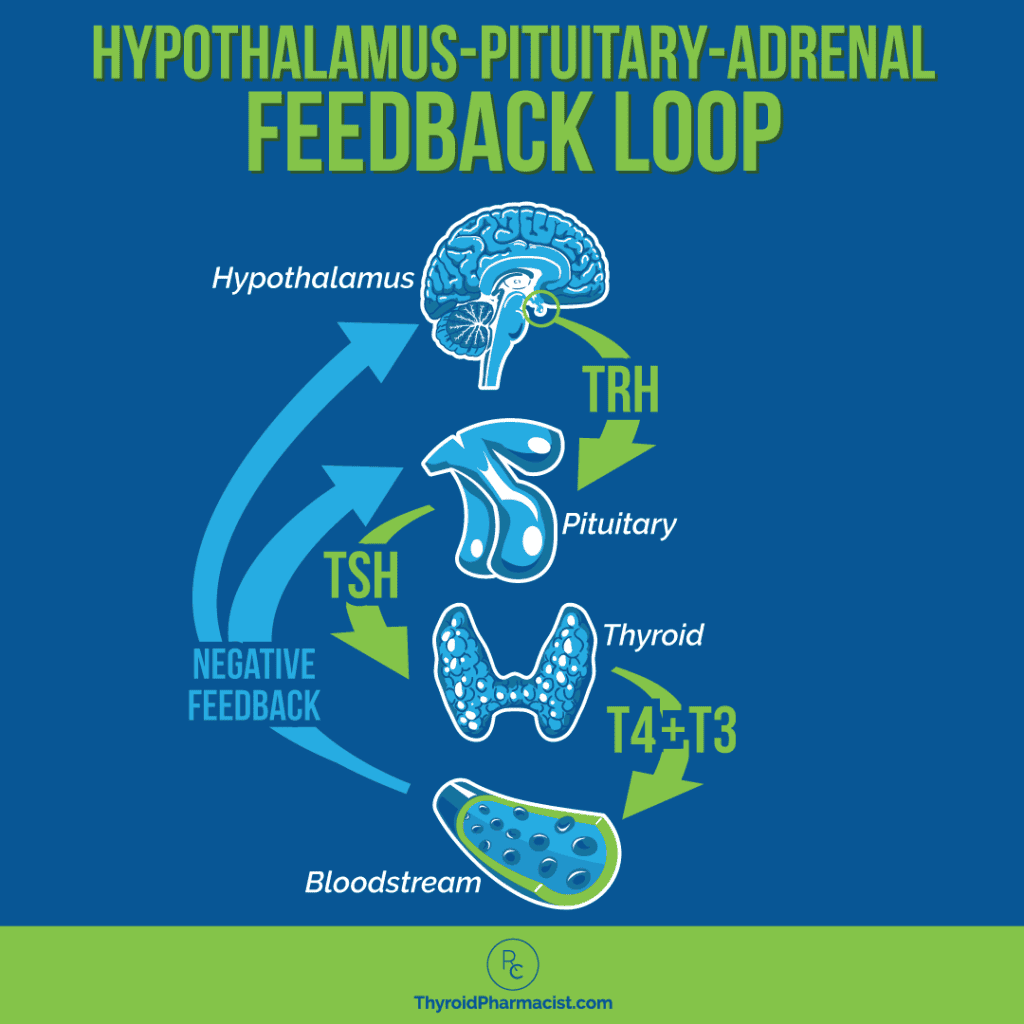
In chemical messenger terms, a healthy communication pathway that results in the production of thyroid hormones, involves the hypothalamus, sensing that there are low levels of thyroid hormones – so it begins secreting thyrotropin-releasing hormone (TRH), which in turn tells the pituitary gland to release thyroid stimulating hormone (TSH). TSH then stimulates the production of thyroid hormone (T4 and T3) from the thyroid gland.
If the hypothalamus doesn’t sense low thyroid hormones (despite them indeed being low), or if the chemical message released by the hypothalamus isn’t received by the pituitary, TSH can be normal or even low, despite the person having low thyroid hormones. This is how central hypothyroidism is thought to occur.
All of the hormones work together in a potent negative feedback system as illustrated below.
Central hypothyroidism is thought to be rare in the general population, with an incidence in otherwise “normal” thyroids (having no Hashimoto’s) estimated to affect about one in 80,000 to one in 120,000 people. [2]
I think this estimate is likely low, since research has speculated (and I agree) that the condition often goes undetected or misdiagnosed (possibly as a mild case of primary hypothyroidism or subclinical hypothyroidism). [3] I’ve personally had it at least three times over the course of testing my thyroid for 10 years, LOL, and have seen it in countless clients!
While I haven’t seen any statistics on this (and boy do I scour PubMed!), I suspect that, based on my own experience having central hypothyroidism, as well as seeing thousands of thyroid labs of people with Hashimoto’s, central hypothyroidism is a lot more common in people with Hashimoto’s compared to the “general” population. We’ll talk about why this might be so.
In my clinical experience, I estimate that the incidence of central hypothyroidism is closer to 5 to 10 cases per 1,000 people with Hashimoto’s.
Symptoms of Central Hypothyroidism
Symptoms of central hypothyroidism may be similar to those of good old (primary) hypothyroidism, such as cold intolerance, headaches, fatigue, muscle cramps, constipation, weakness, peripheral edema, dry skin, and weight gain. [4] Goiters are not typically seen. Some people may have more mild symptoms compared to standard hypothyroid symptoms.
With non-specific, milder thyroid symptoms, this condition can be difficult to diagnose. There are, however, more noteworthy pituitary symptoms that can point the way to a diagnosis.
Because the pituitary gland also controls the production of other hormones, including hormones produced by the adrenal glands and reproductive organs, as well as human growth hormone, prolactin, and oxytocin, many people with central hypothyroidism may experience additional symptoms due to these additional hormonal imbalances. [5]
One study of 48 patients with central hypothyroidism found that only one patient had a singular pituitary hormone deficiency of TSH, whereas 17 percent had a deficiency in two hormones, 16 percent had a deficiency in three, 21 percent had a deficiency in four, 10 percent in five, and 10 percent in six. These pituitary deficiencies are referred to as hypopituitarism. [6]
Pituitary hormone abnormalities that often co-occur in central hypothyroidism include:
- Growth Hormone Deficiencies (GH): GH regulates metabolism, growth, and body composition. Deficiencies can result in fatigue, decreased muscle mass and strength, changes in body fat composition, and premature atherosclerosis (a disease of the arteries resulting from a build-up of plaque). [7]
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) deficiency: These gonadotropin hormone deficiencies can result in issues of the reproductive system, including infertility (due to a reduction in sexual hormones such as estrogen and testosterone, or impacts to egg and sperm maturity), amenorrhea (absence of a woman’s period), loss of libido, and impaired sexual function (erectile dysfunction). It can also result in conditions such as hair loss, anorexia, osteoporosis, dyspareunia (short-term), and premature atherosclerosis (long-term). [8]
- Antidiuretic Hormone (ADH): ADH is produced by the hypothalamus, stored in the pituitary gland, and secreted into the bloodstream. Deficiencies can cause electrolyte imbalances, blood pressure issues, and diabetes insipidus (a condition that is unrelated to diabetes mellitus). Some symptoms of diabetes insipidus include nocturia (needing to urinate during the night), polydipsia (abnormal thirst), and polyuria (producing large volumes of dilute urine). [9]
- Prolactin: Prolactin is needed for breast development and to stimulate milk production for successful breastfeeding. It also plays a role in fertility and sexual function in both men and women. [10]
- Oxytocin: Oxytocin is produced by the hypothalamus, stored in the pituitary, and released into the bloodstream. Known as the “love hormone,” oxytocin plays a role in bonding between friends, mother-newborn bonding (for instance, by stimulating uterine contractions during childbirth and promoting milk secretion during breastfeeding), sexual arousal, romantic attachment, and promoting positive feelings.
- Adrenocorticotropic Hormone (ACTH): ACTH stimulates the adrenal glands to secrete steroid hormones such as cortisol and maintains balance in the hypothalamus-pituitary-adrenal (HPA) axis. Its levels play a large role in how your body responds to stress. Stress activates ACTH production and increases cortisol levels in the body, eventually resulting in adrenal fatigue. Symptoms can include fatigue, persistent infections, dizziness, weakness, nausea, anorexia, hypotension (low blood pressure), and pallor (a very pale color of the skin). The cortisol produced and released by the pituitary gland can also contribute to high blood sugar issues such as hypoglycemia. [11]
Here’s a graphic that illustrates the relationship between the hypothalamus, pituitary, and various target organs (including the thyroid) where symptoms may occur.
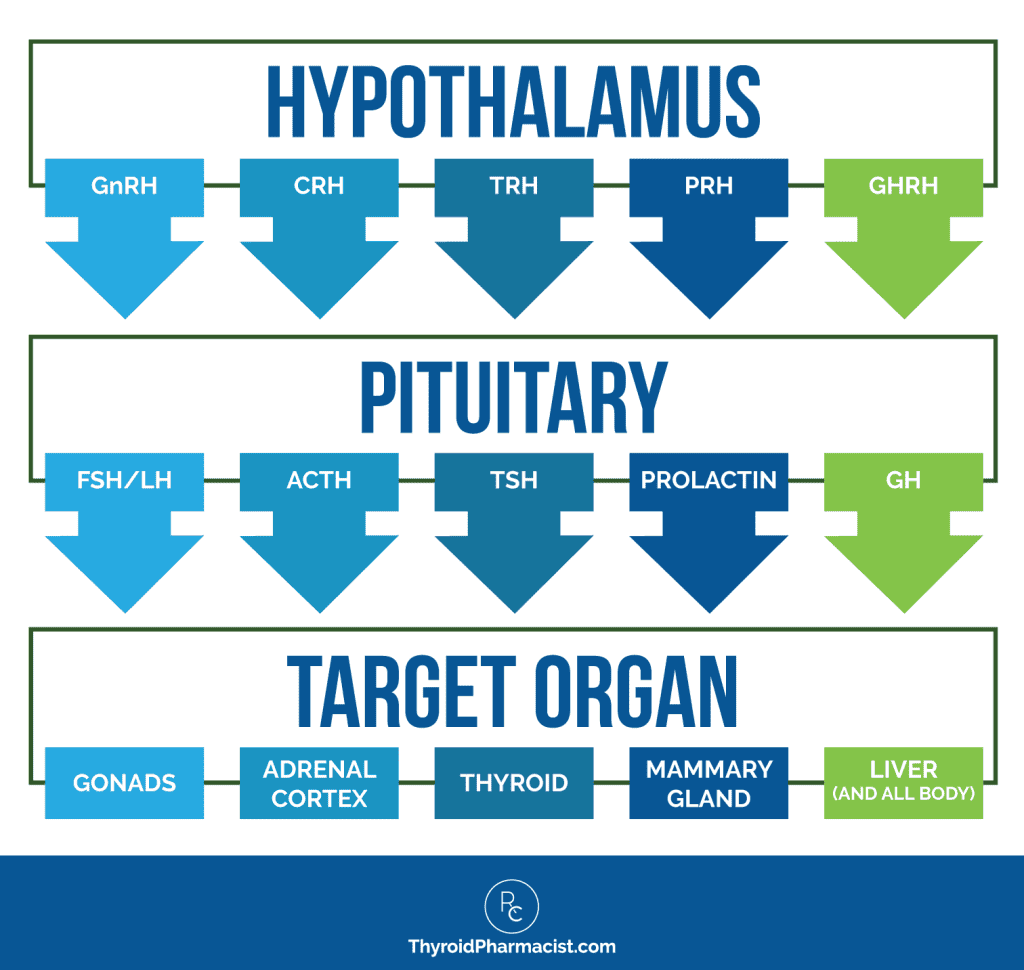
If a doctor knows to look for them, the presence of these types of pituitary symptoms can help identify central hypothyroidism. Some occur more frequently than others. In the earlier mentioned study, for example, pituitary hormone abnormalities were seen in:
- 85 percent of patients for LH/FSH
- 65 percent of patients for GH
- 62 percent of patients for ACTH
- 23 percent for ADH
- 15 percent for prolactin
Of the 48 patients in the study, 60 percent had deficiencies in TSH. [12]
Tumors can also cause excesses in GH, gonadotropin, prolactin, or ACTH.
In my clinical experience, I find that stress and the adrenals (ACTH hormone and cortisol issues) are very large contributing factors in my clients’ cases of central hypothyroidism.
Some 90 percent of my clients with Hashimoto’s have some level of adrenal dysfunction.
Additionally, I see a lot of LH and FSH deficiencies which result in estrogen and progesterone abnormalities and their associated symptoms. Stress (ACTH and cortisol) can diminish progesterone even further, as the adrenals “steal” it to produce cortisol.
I have personally experienced the impact of out-of-balance reproductive hormones.
In one occurrence of central hypothyroidism in my early 30s, I began to have menstrual irregularities, which were a new symptom for me! I had previously had menses like clockwork (or as some would say, my “Aunt Flo” was previously very punctual ;-)). This is a symptom many conventional doctors would likely not associate with central hypothyroidism.
Central hypothyroidism is an important condition that should be identified and addressed. It is important for thyroid function and metabolic health, as well as for heart health, as even mild hypothyroidism may result in higher risks of coronary artery disease and atherosclerosis. An increase in cardiovascular morbidity has also been reported in hypopituitarism. [13]
While symptoms may not always be tell-tale, labs are the best way to identify central hypothyroidism.
The Best Labs for Identifying and Assessing Central Hypothyroidism
Let me preface this section with a cautionary note that many conventional doctors will not perform the necessary labs required to identify central hypothyroidism.
Often, conventional doctors may, as part of a standard lab wellness check, simply do a TSH test. The challenge here is that TSH will usually be low or normal in central hypothyroidism, and certainly not substantially elevated, so the patient will be deemed to have a “normal” thyroid!
There also appears to be more limited recognition by many general practitioners that a normal TSH does not exclude the diagnosis of central hypothyroidism. TSH itself just isn’t a good diagnosis tool, and I’ve been encouraging my community for years to seek out a good functional doctor who does not rely on the singular TSH lab as a valid measure of thyroid health!
In cases of central hypothyroidism, a low or normal level of serum free T4 (along with a low or normal TSH) will best identify the condition. [14]
This is why I always recommend doing a complete thyroid panel. 🙂
While measuring T3 is not usually “required” to diagnose central hypothyroidism, serum total and free T3 levels will typically be normal or low. The exception here is that people on liothyronine (T3) supplementation or who have autonomous thyroid nodules, may have serum T3 levels that are elevated (while having low free T4 and suppressed TSH levels). [15]
Here’s a chart showing how having these lab measures can point to different thyroid states, including central hypothyroidism.
Thyroid Lab Interpretation
| TSH | T4/T3 | Meaning |
| Normal | Normal | Euthyroid |
| Elevated | Normal | Subclinical hypothyroidism |
| Elevated | Low | Hypothyroidism |
| Low | Normal | Subclinical hyperthyroidism |
| Low | High | Hyperthyroidism |
| Low/ Borderline Normal/Normal | Low/Normal | Central hypothyroidism |
Adrenal Testing
Since the adrenals are so often the culprit in central hypothyroidism and Hashimoto’s, I typically recommend the ZRT Adrenal Saliva test to my clients, which you can order through Rupa or MyMedLab.
The test measures the adrenal hormones cortisol and DHEA-S. You can self-order it via the links above. I have found most people who have symptoms and take the test have some level of adrenal dysfunction.
If your cortisol tests as low, and especially if the sex hormone DHEA-S also tests as low, that’s a good indication that you have a pituitary issue going on. If those numbers are fine, that means only your thyroid is not working correctly.
Once you confirm you have a pituitary issue, you can take certain supplements and/or a pituitary glandular to bring your pituitary back to life.
You can self-order a DUTCH test, like I did from Rupa Health or Direct Labs.
You probably will need to work with a practitioner to help you interpret this test, as it is an advanced adrenal test (and more expensive than the adrenal saliva test). I don’t recommend this as an initial test, but for people with pituitary issues, it can provide a lot of interesting and helpful information.
Additional Pituitary Testing to Identify Central Hypothyroidism
Because people with central hypothyroidism often have multiple pituitary hormone deficiencies (such as those causing low adrenal function and low sexual hormones), it may be helpful to test for those as well.
Along with specific tests to measure for abnormalities in individual pituitary hormones (most can be tested via blood tests), some doctors may perform a TRH Stimulation Test to assess what is happening in the pituitary gland. Remember, TRH (thyrotropin-releasing hormone) acts on the pituitary to stimulate the production of TSH.
With this test, TRH is administered intravenously, and changes to the TSH level are measured. This test was used more often in the past, but now the measures of T4 and TSH (and to some extent T3) are typically the preferred tests. (They’re less invasive, too.)
Patients who have lab results that point to central hypothyroidism and/or symptoms of pituitary tumors (mass lesions, recurring headaches, visual field disturbances) may require further testing, such as an MRI or CT scan, to evaluate the hypothalamic-pituitary region for abnormalities (pituitary adenoma, a tumor, being the most frequent cause of central hypothyroidism).
Again, working with the right doctor is important, as some general practitioners are just not familiar with the condition. Research has found missed diagnoses as well as delays relating to the diagnosis of central hypothyroidism. One small study looked at 16 patients with central hypothyroidism and found that even though 81 percent of them had both TSH and T4 measured, and 75 percent had results suggesting pituitary disease (and 44 percent had symptoms), there was still a delay in diagnosis that ranged from three to more than 12 months. [16]
Common Causes for Central Hypothyroidism
I’ve experienced central hypothyroidism three times. The causes contributing to my condition included:
- Being overmedicated with thyroid meds
- Taking hydrocortisone
- Using topical steroids
- Taking adrenal glandulars
- Being super stressed
- Mold exposure
I’ll share more about these and other potential causes.
Please note that someone can have a genetic disposition to central hypothyroidism, and there have been a number of genes identified that relate to the pituitary dysfunction seen in central hypothyroidism. Someone having one or more of these would likely have both a family history of pituitary or hypothalamus-related disease, as well as lifelong issues with symptoms and lab abnormalities.
Beyond genetics, a variety of additional causes have been described in the literature for central hypothyroidism that occurs in non-Hashimoto’s patients. These include:
- Sick euthyroid syndrome, a condition seen in about 75 percent of hospitalized patients with critical illnesses where there are changes in thyroid function, resulting in a low total T3 and free T3 levels, with normal T4 and TSH levels. [17]
- Tumors, such as a pituitary adenoma (the most common cause of central hypothyroidism causing compression on the cells in the pituitary that produce TSH, thus decreasing its secretion and/or causing abnormalities in pituitary hormones) or cancerous pituitary lesions that have metastasized. [18]
- Aneurysms
- Pituitary atrophy/shrinkage
- Infections (toxoplasmosis, tuberculosis, syphilis, and bacterial abscess, among others)
- Radiation
- Trauma/head injury/concussion
- Sarcoidosis (an inflammatory condition)
- The use of addictive substances, including morphine and even sniffing glue [19]
- Smoking (Smoking has been found to affect hormone secretions relating to the pituitary, adrenals, ovarian and testicular function, thyroid, the action of insulin, and calcium metabolism. Research has found it increases the risk and severity of Graves’ hyperthyroidism (low TSH) and osteoporosis, ophthalmopathy, and reduced fertility.) [20]
Medications
Additionally, some medications have been reported to lead to central hypothyroidism and/or TSH suppression. Most of these are transient conditions and are reversible.
- Over-replacement with thyroid hormones: When we use thyroid medications, it’s important for them to be at the right levels for our needs. If levels are too high, this can suppress the feedback loop between free T3, free T4, and TSH, resulting in suppressed levels of TSH.
- Corticosteroids: These man-made anti-inflammatory medications that closely resemble cortisol, are often referred to as steroids. They include things like hydrocortisone, cortisone, prednisone, and prednisolone. They can suppress TSH secretion, especially if used in high doses, with prolonged use, or if they are given at bedtime, when the pituitary signals the thyroid. [21] TSH drops in the presence of increased cortisol. Normally, TSH is supposed to increase in the evening, as cortisol decreases. Taking corticosteroids in the evening or later in the day, can suppress TSH secretion through direct effects on TRH in the hypothalamus. In the long term, corticosteroids can suppress pituitary function by inhibiting the release of ACTH from the pituitary gland. Please note that even steroid-containing creams can do this when used for a prolonged time and in the evening.
- Growth hormone-suppressing medications: One example of these is octreotide, which is used for acromegaly, a rare condition. These medications interfere with the communication of the thyroid and pituitary, potentially suppressing TSH levels. [22]
- Dopamine-affecting drugs: Amphetamines like Adderall or Ritalin, as well as the dopamine receptor agonist Wellbutrin (bupropion), often prescribed for depression, may affect TSH secretion, likely due to their ability to suppress the secretion of prolactin, impacting the feedback loop. [23]
- Salicylates: These common over-the-counter medicines like aspirin can affect thyroid function by suppressing TSH secretion from the pituitary. [24]
- Carbamazepine: This medication used for seizures and other antiepileptic medications, may alter pituitary responsiveness and result in central hypothyroidism; however, research is limited. [25]
- Rexinoids: Medications such as Bexarotene, used for the treatment of cutaneous T-cell lymphoma and which is being studied for use in many other advanced cancer conditions, as well as metabolic and dermatologic disorders, have been found to induce clinically significant central hypothyroidism in most patients. [26]
- Accutane® and other retinoids (isotretinoin): These medications have been found to suppress both TSH as well as some pituitary hormone levels such as ACTH, LH, total testosterone, and prolactin levels. [27] Brand names for isotretinoin include Accutane®, Absorica®, Claravis®, Amnesteem®, Myorisan®, Sotret®, and Zenatane™.
- Opioids: Opioid medications such as morphine, codeine, oxycodone, and hydrocodone, suppress the release of gonadotropin-releasing hormone (GnRH), which then decreases the release of LH and FSH, resulting in decreased production of key hormones in both men and women. [28]
- High-dose estrogen therapy: Long-term use of oral contraceptives or hormone replacement therapy can inhibit the release of GnRH and suppress the secretion of LH and FSH from the pituitary gland. [29]
- Antipsychotics: Some antipsychotic medications such as risperidone (used to treat schizophrenia and bipolar disorder) may lead to high levels of prolactin and potential suppression of other pituitary hormones. [30]
Natural Supplements
As a pharmacologist, whenever I learn about new ways our body responds to various substances, I think about the mechanism of action. Medications and natural supplements can have very similar mechanisms of action, and while there is less known about supplements causing pituitary suppression, in theory, the following supplements could potentially lead to dampening pituitary hormone production, especially when used in doses that are too high, for too long, or too close to bedtime. Please note that in my experience, they’re fine for most people, but if a person with pituitary suppression was taking them, I would be asking questions as to whether they were contributing.
- Adrenal-supporting supplements – While I have not seen this anywhere in the literature, I have seen clinically that some adrenal-supporting supplements (especially adrenal glandulars and pregnenolone) can lead to pituitary suppression.
- Adrenal glandulars are derived from sheep, pig, or cow adrenal glands, and I’ve seen their use cause HPA axis suppression and atrophy (turning off production of the body’s own adrenal hormones as well as thyroid hormones by pituitary feedback loop inhibition, decreasing TSH and causing central hypothyroidism). Someone who initially feels better taking adrenal glandulars, only to crash a few weeks/months later with a normal or low TSH, should be suspected of HPA axis suppression. For this reason, they should only be taken under medical supervision.
- Pregnenolone is a hormone that is produced by the adrenals, and is also available in supplement form. Pregnenolone is often “stolen” by the body to produce more cortisol in times of stress. It is often recommended by functional practitioners when someone is experiencing adrenal fatigue and has low progesterone, aldosterone, or DHEA.
- L-tyrosine (which is a dopamine precursor) may contribute to pituitary suppression, but I don’t have enough data to confirm this.
- Some adrenal adaptogens may also contribute, although again, I don’t have enough patient cases to confirm this definitively. Given the involvement of the HPA axis in central hypothyroidism cases, it makes sense that some supplements meant to support the adrenals (with the goal of lowering TSH and bumping up cortisol production) could result in pituitary suppression for some people.
- High-dose melatonin: High doses or prolonged use of a melatonin supplement can affect the body’s circadian rhythm, and may also interact with the HPA axis, which may result in suppressed pituitary function. [31]
- DHEA: DHEA is a hormone produced by the adrenal glands, and is a precursor to sex hormones. It’s available as a supplement, and some people will take it for its reported anti-aging and performance-enhancing effects (levels decline as we age). High doses may interfere with the hypothalamus-pituitary feedback loop and affect pituitary function.
- Licorice root: Licorice root and its extract contain glycyrrhizic acid and glycyrrhetinic acid. These compounds inhibit a certain enzyme that is required for the conversion of cortisol into its active form, which over time can result in increased cortisol levels and HPA axis dysregulation; however, this effect is not well understood.
- Soy isoflavones: Soy isoflavone supplements are sometimes taken for menopausal symptoms and to support bone health. Because of their estrogenic effects, high doses of soy isoflavones may interact with estrogen receptors, and potentially affect hormone balance and hypothalamic-pituitary feedback mechanisms.
Whenever I have a client I suspect of having central hypothyroidism, I immediately opt for a medication and supplement review, paying special attention to thyroid and adrenal boosters that may “override” the system.
Exposures/Conditions
While most research focuses on drugs as culprits, and I have personally experienced central hypothyroidism while taking both glandulars and pregnenolone in the past, theoretically, anything that overwhelms the feedback loop and causes excess estrogen (like estrogen dominance, exposure to xenoestrogens, exposure to mycotoxins), excess salicylates (such as microbiome-induced salicylate toxicity) and of course excess cortisol (from extreme stress), could also lead to central hypothyroidism/pituitary suppression.
Stress
Along with adrenal-supportive supplements causing potential TSH suppression, there is research showing that stress itself can result in pituitary hormone deficiencies, including lower TSH. When we experience stress, we initially have high levels of cortisol in the body. Through the intricate feedback loop of the HPA axis, these high cortisol levels can cause suppression of other hormones, eventually leading to central hypothyroidism.
There has been some interesting research done regarding trauma (in animals and humans) showing how the stress from trauma increases HPA axis activity due to increases in corticotropin-releasing hormone (CRH), causing greater ACTH release. [32]
I know I had central hypothyroidism at least once due to being super stressed out, and as mentioned, I routinely see clients with central hypothyroidism alongside underlying stress and adrenal issues.
Even so, a conventional doctor is not likely to acknowledge stress or adrenal fatigue as “real” conditions that need treatment. The exception would be if a patient tested positive for Addison’s disease, an autoimmune condition that can result from extreme adrenal insufficiency.
Mold Exposure
The connection between mold exposure and pituitary issues is not well established, however, there is some research that suggests that mold exposure can impact hormone regulation and pituitary function.
My understanding of this mold-pituitary connection is that because mold can colonize the sinuses and can lead to allergies and sinus infections, this can cause inflammation in the sinuses and surrounding tissues, including the pituitary gland. Inflammation itself can also affect the HPA axis.
Other potential mechanisms that may explain why mold can contribute to pituitary dysfunction include exposure to mycotoxins and the neurological effects of mold, which may influence pituitary function.
One study looked at 79 patients with a history of mold exposure to see if there was a connection to anterior hypopituitarism, especially growth hormone deficiency. Of these patients, 94 percent had a history of chronic rhinosinusitis, 81 percent had primary or secondary hypothyroidism, 75 percent were deficient in ACTH, and 51 percent were deficient in growth hormone. [33] The study found that exposure to mold likely represents a major cause of growth hormone deficiency.
Based on this study and my own clinical observations, mold exposure does seem to play a role in central hypothyroidism (not to mention, many other health issues). It was certainly a factor for me one of the times I experienced central hypothyroidism!
Sleep, Diet, and Other Factors Contributing to Central Hypothyroidism
The research is a bit lacking in regards to lifestyle causes of the condition, but clinically I have found that inflammatory states – including those directly influenced by our own decisions – can indirectly affect pituitary secretions (in particular the adrenals) and be involved in the pathogenesis of central hypothyroidism. [34]
Sleep, blood sugar, diet, environmental toxins, and other inflammatory factors likely contribute. Leptin (the body’s satiety hormone which inhibits hunger when the body no longer needs additional energy) and other hormones related to eating behavior and sleep, have been shown to indirectly affect pituitary secretions. [35]
Many of these same root cause lifestyle factors that trigger autoimmunity in Hashimoto’s can impact pituitary hormones, although most conventional practitioners won’t evaluate or treat these types of root causes.
Conventional Treatment
Levothyroxine therapy is the conventional standard of care for central hypothyroidism, yet (as you may have guessed), using this alone does not get to the root of the problem, and may not be enough for some people. That said, it is often a great place to start when thyroid hormones are low, as it can help you manage and in some cases prevent the symptoms and consequences of hypothyroidism.
Because TSH levels are not particularly helpful in the cases of central hypothyroidism, doctors will need to test levels of actual thyroid hormones, T4 and T3. Monitoring needs to be frequent, initially at every one to two months.
The goal of levothyroxine therapy is to achieve free T4 concentrations in the upper end of the reference range, see improvements in clinical symptoms, and regulate one’s heart rate, which can be low in those with hypothyroidism. [36]
Most pituitary hormones can be easily tested with a blood test. GH and ACTH require stimulation tests, and an ACTH stimulation test is usually given to rule out adrenal insufficiency. [37]
In the case that a mass is found, an assessment for a tumor would take place, possibly resulting in surgery or other treatments.
The conventional view is that most hormone deficiencies related to central hypothyroidism are irreversible conditions requiring lifetime hormone replacement.
Besides thyroid hormones, other hormones that may need to be replaced (and how to do so) are beyond the scope of this article, but hormone replacement may need to be considered.
What I Recommend for Central Hypothyroidism
In contrast to being a lifelong sentence, I have found that pituitary suppression and/or central hypothyroidism can be a temporary occurrence… as long as you do the right things!
The first thing I would do for anyone experiencing this (assuming you’ve already had a work-up with your conventional doctors and ruled out causes such as tumors), would be reviewing your medications and supplements to see if any of them could be the cause.
In some cases, tapering the corticosteroids or other offending medications/supplements from my earlier lists may do the trick in resolving central hypothyroidism. Always work with a qualified professional when tapering!
Supplements That May Help with Pituitary Suppression
The first time I had pituitary suppression, I was in my late twenties and I was taking adrenal glandulars. Stopping them resolved the condition.
The second time my labs pointed to me having central hypothyroidism was sometime after we moved to Boulder, CO, and I was in my early thirties. I was not hungry at all, but found myself gaining weight. I put on close to 10 pounds within two months! I also slept a LOT during that time! So I reduced my thyroid medication dosage, thinking that perhaps I was overdosed, and this resulted in my T3/T4 plummeting lower, while my TSH stayed depressed.
I was taking pregnenolone and hydrocortisone to support my adrenals at the time, and decided to taper off of both to see if that would help with my symptoms and numbers.
My symptoms improved slightly, but I was still more tired than usual. I tested my thyroid and adrenals again (once I was off the pregnenolone and hydrocortisone), and found that my TSH was still suppressed, and worse, so were my adrenals – my internal cortisol production was barely there. I also began to have the menstrual irregularities I mentioned earlier.
I decided on advanced adrenal testing through the DUTCH test, which revealed that I was indeed having pituitary suppression, and this was potentially leading to impaired thyroid and adrenal hormone production.
The lovely clinicians at the Precision Analytical Provider support line gave me a couple of protocol ideas (one of my hobbies is speaking to the technical support people with various lab companies to nerd out on lab results and learn new things). I implemented the protocol I will share with you below for myself, and have used it successfully with numerous clients over the last decade. The protocol is followed for two to three months, at which time, the labs are retested and it can be continued for an additional three months if needed.
- Femmenessence Maca: 1000-2000 mg per day in the morning
- Cordyceps by NOW Foods: 500-1000 mg per day
- Cytozyme PT/HPT by Biotics Research: 1-3 per day
Maca
Maca stimulates the endocrine system through plant sterols which are utilized by the body with the help of the pituitary to improve adrenal function, ovarian and testicular function, thyroid function, pancreas function, and pineal gland function.
Maca has wonderful hormone-balancing properties that are supportive of the adrenals and the thyroid. I like Femmenessence, which has different formulations for women and men.
Maca is also known for its ability to support female hormone balance and menopause-related symptoms. While it does not have estrogenic properties, if you have any hormone-sensitive condition or estrogen-specific concerns, you should consult with your doctor. [38]
Adrenal adaptogens can have different effects on different people — some may find that they are overstimulated. With that in mind, be alert for side effects like jitters or heart palpitations.
Adrenal adaptogens and glandulars should be used with caution, one at a time to start, and under the guidance of a functional practitioner. Please take care to review all precautions on the package.
Cordyceps
A type of mushroom, cordyceps supports the HPA axis, and has anti-inflammatory, antioxidant, antiviral, and immune-modulating properties. It may also help to regulate blood sugar. It is rich in selenium, which is important to thyroid health and may support neurological health. Many of my clients report that it helps reduce fatigue. [39]
Cordyceps by NOW at a dosage of 500 to 1000 mg per day is a good place to start.
Cordyceps may not be suitable for everyone and may decrease the effectiveness of certain medications. Please see package instructions for precautions, and consult with your practitioner before introducing cordyceps.
Cytozyme PT/HPT
Pituitary/Hypothalamus Complex Concentrate (PT/HPT) by Biotics Research is a blend of pituitary and hypothalamic concentrates (derived from lamb), combined with other important antioxidant enzymes, to provide pituitary, hypothalamus, and adrenal function support.
The dosage is one daily, up to three times a day.
Using these three supplements for about three months is generally going to be the target for rebalancing. If you still have symptoms, continue for another few months, and retest your thyroid labs at about the six-month mark.
At that point, if you still have symptoms, you may wish to taper slowly at about a 10 to 20 percent reduction in dose, every four days to one week. Rapid withdrawal may cause symptoms like pain, low blood pressure, extreme fatigue, nausea, and a rebound effect of the thyroid condition.
If you’re curious about the third time I experienced central hypothyroidism, I will share that it was likely due to stress AND mold exposure, and required a bit more work! I have shared a comprehensive mold protocol in my Root Cause Reset Program, and hope to update my article on mold soon.
Takeaway
Central hypothyroidism is often due to a communication breakdown between the hypothalamus and pituitary that results in thyroid hormones not being produced. It is identified by labs consisting of a low or borderline normal TSH level, along with low or normal free T4 levels.
Symptoms include standard thyroid symptoms (which in some cases are more mild than symptoms of overt hypothyroidism), and often one or more symptoms associated with abnormal pituitary hormones, such as amenorrhea, infertility, loss of libido, or impaired sexual function.
I’ve experienced it a few times myself, and have seen it in many of my clients with Hashimoto’s.
Conventional doctors might tell you that central hypothyroidism (unless brought on by specific medications) will result in life-long hormone replacement of both the thyroid and any affected pituitary hormone disorder.
But I can tell you that this is not always the case if you know how to reconnect that communication pathway!
Have your lab results pointed to central hypothyroidism? If so, remember that healing may start with adjusting your medication.
Please let me know how things are going in the comments below!
I hope that you find this information helpful on your journey in overcoming Hashimoto’s!
P.S. You can also download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free, by signing up for my weekly newsletter. You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow me on Facebook, Instagram, Pinterest, and TikTok!
References
[1] Persani L, Cangiano B, Bonomi M. The diagnosis and management of central hypothyroidism in 2018. Endocr Connect. 2019;8(2):R44-R54.
[2] Persani L, Cangiano B, Bonomi M. The diagnosis and management of central hypothyroidism in 2018. Endocr Connect. 2019;8(2):R44-R54.
[3] Benvenga S, Klose M, Vita R, Feldt-Rasmussen U. Less known aspects of central hypothyroidism: Part 1 – Acquired etiologies. J Clin Transl Endocrinol. 2018;14:25-33. Published 2018 Sep 26. doi:10.1016/j.jcte.2018.09.003
[4] Ross DS. Central Hypothyroidism. UpToDate. 2021. Retrieved December 11, 2021. https://www-uptodate-com.mwu.idm.oclc.org/contents/central-hypothyroidism
[5] Benvenga S, Klose M, Vita R, Feldt-Rasmussen U. Less known aspects of central hypothyroidism: Part 1 – Acquired etiologies. J Clin Transl Endocrinol. 2018;14:25-33. Published 2018 Sep 26. doi:10.1016/j.jcte.2018.09.003; Ross DS. Central Hypothyroidism. UpToDate. 2021. Retrieved December 11, 2021. https://www-uptodate-com.mwu.idm.oclc.org/contents/central-hypothyroidism
[6] Yamada M, Mori M. Mechanisms related to the pathophysiology and management of central hypothyroidism. Nat Clin Pract Endocrinol Metab. 2008;4(12):683-694. doi:10.1038/ncpendmet0995
[7] Kim SY. Diagnosis and treatment of hypopituitarism. Endocrinol Metab (Seoul). 2015;30(4):443-455.
[8] Ibid
[9]Ibid
[10] Freeman ME, Kanyicska B, Lerant A, Nagy G. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80(4):1523-1631. doi:10.1152/physrev.2000.80.4.1523
[11]Ross DS. Central Hypothyroidism. UpToDate. 2021. Retrieved December 11, 2021. https://www-uptodate-com.mwu.idm.oclc.org/contents/central-hypothyroidism; Kim SY. Diagnosis and treatment of hypopituitarism. Endocrinol Metab (Seoul). 2015;30(4):443-455.
[12] Yamada M, Mori M. Mechanisms related to the pathophysiology and management of central hypothyroidism. Nat Clin Pract Endocrinol Metab. 2008;4(12):683-694. doi:10.1038/ncpendmet0995
[13] Feldt-Rasmussen U, Klose M. Central hypothyroidism and its role for cardiovascular risk factors in hypopituitary patients. Endocrine. 2016;54(1):15-23.
[14] Persani L, Cangiano B, Bonomi M. The diagnosis and management of central hypothyroidism in 2018. Endocrine Connections. 2019; 8(2): R44-R54. Retrieved Dec 10, 2021, https://ec.bioscientifica.com/view/journals/ec/8/2/EC-18-0515.xml; Ross DS. Central Hypothyroidism. UpToDate. 2021. Retrieved December 11, 2021. https://www-uptodate-com.mwu.idm.oclc.org/contents/central-hypothyroidism https://www-uptodate-com.mwu.idm.oclc.org/contents/central-hypothyroidism
[15] Ross DS. Central Hypothyroidism. UpToDate. 2021. Retrieved December 11, 2021. https://www-uptodate-com.mwu.idm.oclc.org/contents/central-hypothyroidism
[16] Benvenga S, Klose M, Vita R, Feldt-Rasmussen U. Less known aspects of central hypothyroidism: Part 1 – Acquired etiologies. J Clin Transl Endocrinol. 2018;14:25-33. Published 2018 Sep 26. doi:10.1016/j.jcte.2018.09.003
[17] Ganesan K, Wadud K. Euthyroid sick syndrome. [Updated 2020 Nov 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. https://www.ncbi.nlm.nih.gov/books/NBK482219/
[18] Ross DS. Central Hypothyroidism. UpToDate. 2021. Retrieved December 11, 2021. https://www-uptodate-com.mwu.idm.oclc.org/contents/central-hypothyroidism
[19] Ibid
[20] Jorde R, Sundsfjord J. Serum TSH levels in smokers and non-smokers. The 5th Tromsø study. Exp Clin Endocrinol Diabetes. 2006 Jul;114(7):343-7; Kapoor D, Jones TH. Smoking and hormones in health and endocrine disorders. Eur J Endocrinol. 2005 Apr;152(4):491-9.
[21] Haugen BR. Drugs that suppress TSH or cause central hypothyroidism. Best Pract Res Clin Endocrinol Metab. 2009;23(6):793-800. doi:10.1016/j.beem.2009.08.003
[22] Ibid
[23]Ibid
[24] Samuels MH, Pillote K, Asher D, et al. Variable effects of nonsteroidal antiinflammatory agents on thyroid test results. J Clin Endocrinol Metab. 2003 Dec;88(12):5710-6.
[25] Ibid
[26] Ibid
[27] AlSaif F, AlOtaibi H, Balbisi A, et al. Affect of oral isotretinoin therapy on thyroid function in patients with moderate-to-severe acne vulgaris: A prospective study. J Dermatol Dermatol Surg. 2020. 24(1):38-40; Gül O, Cander S, Çalapkulu M, et al. A rare cause of central hypothyroidism: oral isotretinoin treatment. Endocrine Abstracts. 2018; 56:703. doi: 10.1530/endoabs.56.P703
[28] Bradley A, Boland JW. Effects of Opioids on Immune and Endocrine Function in Patients with Cancer Pain. Curr Treat Options Oncol. 2023;24(7):867-879. doi:10.1007/s11864-023-01091-2
[29] Shaw ND, Histed SN, Srouji SS, Yang J, Lee H, Hall JE. Estrogen negative feedback on gonadotropin secretion: evidence for a direct pituitary effect in women. J Clin Endocrinol Metab. 2010;95(4):1955-1961. doi:10.1210/jc.2009-2108
[30] Stojkovic M, Radmanovic B, Jovanovic M, Janjic V, Muric N, Ristic DI. Risperidone Induced Hyperprolactinemia: From Basic to Clinical Studies. Front Psychiatry. 2022;13:874705. Published 2022 May 6. doi:10.3389/fpsyt.2022.874705
[31] Pereira JC Jr, Pradella Hallinan M, Alves RC. Secondary to excessive melatonin synthesis, the consumption of tryptophan from outside the blood-brain barrier and melatonin over-signaling in the pars tuberalis may be central to the pathophysiology of winter depression. Med Hypotheses. 2017;98:69-75. doi:10.1016/j.mehy.2016.11.020
[32] Rinne T, de Kloet ER, Wouters L, et al. Hyperresponsiveness of hypothalamic-pituitary-adrenal axis to combined dexamethasone/corticotropin-releasing hormone challenge in female borderline personality disorder subjects with a history of sustained childhood abuse. Biol Psychiatry. 2002 Dec 1;52(11):1102-12.
[33] Dennis D, Robertson D, Curtis L, Black J. Fungal exposure endocrinopathy in sinusitis with growth hormone deficiency: Dennis-Robertson syndrome. Toxicol Ind Health. 2009;25(9-10):669-680. doi:10.1177/0748233709348266
[34] Benvenga S, Klose M, Vita R, Feldt-Rasmussen U. Less known aspects of central hypothyroidism: Part 1 – Acquired etiologies. J Clin Transl Endocrinol. 2018;14:25-33. Published 2018 Sep 26. doi:10.1016/j.jcte.2018.09.003
[35] Persani L. Clinical review: Central hypothyroidism: pathogenic, diagnostic, and therapeutic challenges. J Clin Endocrinol Metab. 2012;97(9):3068-3078. doi:10.1210/jc.2012-1616
[36] Gupta V, Lee M. Central hypothyroidism. Indian J Endocrinol Metab. 2011;15(Suppl 2):S99-S106.
[37] Kim SY. Diagnosis and treatment of hypopituitarism. Endocrinol Metab (Seoul). 2015;30(4):443-455.
[38] Meissner HO, Mrozikiewicz P, Bobkiewicz-Kozlowska T, et al. Hormone-Balancing Effect of Pre-Gelatinized Organic Maca (Lepidium peruvianum Chacon): (I) Biochemical and Pharmacodynamic Study on Maca using Clinical Laboratory Model on Ovariectomized Rats. Int J Biomed Sci. 2006;2(3):260-272.
[39] Olatunji OJ, Feng Y, Olatunji OO, et al. Cordycepin protects PC12 cells against 6-hydroxydopamine induced neurotoxicity via its antioxidant properties. Biomed Pharmacother. 2016 Jul;81:7-14.; Das SK, Masuda M, Sakurai A, et al. Medicinal uses of the mushroom Cordyceps militaris: current state and prospects. Fitoterapia. 2010 Dec;81(8):961-8.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Thank you. This is very helpful. I have central hypothyroidism which was why I was not diagnosed for a long time. I am in the UK and had to seek treatment privately. My TSH has been 0.01 mIU/L for years and but my T3 and T4 were incredibly low. On levothyroxine for years now, T3 and T4 are now well within range. However I keep being told that having low levels of TSH for many years has been associated with osteoporosis. I have not had a bone density scan. I am now 67 and not aware of any problems here. What is your opinion on osteoporosis in relation to TSH?
Alison – thankyou for reaching out. Here is an article that I hope is helpful: https://thyroidpharmacist.com/articles/micronutrients-bone-density-and-hashimotos/
So I had to have my thyroid removed and I was put on Synthroid and was seeming to do ok except at one point my TSH shot unexpectedly high but my T4 was in range and at the lower side, so as expected with a high TSH. My doctor switched me to Armour and I went to a 37 TSH. After a couple more test then my TSH was slightly low but now my T4 was also low. I fought Hashimoto’s for over 4 years before my thyroid removal and was fine for a year after surgery on the Synthroid with my T4 always in range and on the opposite side of my TSH every time it was test until the med change to Armour…could just this medication change be the cause of my T4 now being out and now on the same side as my TSH?
Jen – thank you for sharing your journey. I’m so sorry you are struggling with all of this. Removing the thyroid with a thyroidectomy eliminates thyroid antibodies, as there is nothing left to attack. However, life is not always roses with a thyroidectomy, as it does not remove the autoimmunity. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target.
We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are a couple articles you might find interesting:
IMPORTANCE OF GUT HEALTH
https://thyroidpharmacist.com/articles/importance-gut-health/
WHERE DO I START WITH HASHIMOTO’S
https://thyroidpharmacist.com/articles/where-do-i-start-with-hashimotos/
OMG … now that I know what to look for it looks like I’m being overmedicated and/or I have Central Hypothyroidism. Am I right?
TSH Free T4
mlU/L pmol/L
Oct 15/08 1.80 16.00
Jan 1/12 8.00
May 22/12 0.37 12.90
Aug 7/15 1.10 12.30
Nov 24/15 1.40
Sept 6/17 0.04 13.00
Oct 24/17 0.09 12.90
Dec 6/17 0.42 9.90
Jan 11/18 0.29 10.10
May 13/19 0.29 11.20
Sept 1/19 0.04 13.00
Jan 10/20 1.69 8.40
Nov 20/20 0.80
Jan 11/21 1.53 11.20
Jan 4/22 1.40 10.60
Aug 11/22 0.53
Oct 13/23 0.99 10.10
My doctor’s keep saying everything looks fine and not adjusting meds (I take dessicated thryroid).
Hi Alison, Thank you for following this page. I’m so sorry you are struggling with this. I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and preventing serious chronic disease rather than treating individual disease symptoms. Check out this article:
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
I went down so many paths with so many blood tests for several years before finally getting the “fibromyalgia” bucket diagnosis by a Rheumatologist in 2014. My then Dr tested my TSH but only begrudgingly tested T3 and T4 a few times after I badgered him. It only ever resulted in “your labs are fine. I can refer you to rheumatology.” Now reading this I went looking at my past labs and see that they were all on the very low end of the ranges. Where do I go from here? Even though my younger Dr is an OD she gets stuck in the same loop as my other Doctors just looking at ranges. I just started BHRT that was prescribed by my Gyn. I’m so tired of the whackamole that is women’s health (sigh).
Toni – thank you for following and sharing your journey. I’m so sorry you have had to experience this. I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and preventing serious chronic disease rather than treating individual disease symptoms. Check out this article:
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
Thank you so much for this article!! I’ve been struggling with this exact thing for awhile and have always used your research to help my thyroid journey but could never find much on central hypothyroidism. I was so pumped to see this tonight and am truly so grateful for all your research you do and share with others.
Katie – You’re welcome! I hope you find it helpful!
I believe this is my current issue. I’ve had Hashimoto’s since 2002 and it has been regulated with 100mcg of Synthroid for years. I recently had a significantly stressful event. Several days afterwards, it felt like a switch was flipped. I started waking up multiple times a night- especially at 3am, have to urinate each time, and feel absolutely wiped out. With My last visit to my endocrinologist, my TSH was low, my free T4 was normal, and my total T3 was low. The only change my doctor made was for me to take half of dose of Synthroid every 7th day and she wants to see me in 3 months. I’m extremely frustrated with this. I’m now working with a functional medicine doctor, but won’t be able to see her until July. I really appreciate this article because I now have some understanding and will work on approaching my doctors about this.
CB – thank you for sharing. I’m so glad to hear you found this article helpful and that you have found a functional practitioner to help you! I hope you will keep me posted on your progress. ❤️
Thank you for sharing all your researches. I experimented this condition for year and i will follow your recommendation. I am under ERFA so i will slowly decreased the medication time I am boosting the pituitary gland with the supplements recommended.
Hopefully i will succeed to reconnect the communication pathway. Thank you very much.
Valerie – thank you for sharing. I do hope that you are working with your practitioner so they can monitor you while decreasing medications. It is never advisable to stop taking your medications, or alter your dosages, without the advice of your practitioner. T4 thyroid hormone medications have a half-life of about 1 week. This means that when a person stops taking them, the amount of the hormone activity in their body, from the medication, will decrease by about 1/2 each week. For T3 medications, this half-life is only about 1 day. Generally, within three weeks (or a few days for T3), most of the hormone will be out of the body. This could result in increased symptoms, an increase in the autoimmune attack on the thyroid, and extra stress on your body and the thyroid. Thyroid hormones affect every organ, tissue and cell in the body. Appropriate medication management will allow you to recover from the effects of hypothyroidism, giving you the energy, vitality and support to continue working on optimizing your health. Please do not change your medications without speaking to your doctor first.
Thank you so much for this article! I hope to share it with my PCP that just 2 months ago said I had autoimmune thyroid. But with my recent labs:
TSH 0.718
T4 5.7
Free T4 0.79
T3 92
T3 Uptake 23
Free T3 2.3
Reverse T3 10.6
TPO 9
I’m now really confused
Carletta, you’re welcome. Here is an article with some info on how to interpret your labs that I hope is helpful: https://thyroidpharmacist.com/articles/top-10-thyroid-tests/
Had wished could have found this on “Central” hypothyroidism 15 yrs ago !! Am wondering how much thyroid FT4 needs to be at on a lab compared to TSH to consider it CH. My TSH is usually 1.2 (0.7-2.2ranges over 10yrs) but see FT4 can be in range by labs but lower. Have had FT3out lo but when prescribed cytomel, got fast heartbeats and hot, so stopped and figured was adrenal issue and nutrients.
Would be nice to not be so chilly espec in winter. Had read licorice root reduces an enzyme that changes active cortisol to inactive cortisol (cortisone), so it can keep it from lowering too fast for a short time. Will ck out article on mold as had house then w mold.
Hi Izabella! Thank you for this article. I’ve been suffering with this and it took a year for me to figure it out. It’s done a lot of damage in that time. It was brought on by chronic high cortisol and probably a taxing of my adrenals. I’ve seen so many doctors and my Functional dr. doesn’t understand it but my PCP was kind enough to believe me and prescribe me Levothyroxine finally. I’m struggling a bit though because Levo often makes me feel as if I’ll go hyper, but it fixes all my problems too! I’ll take one 25mcg pill of Tirosint and it’ll feel like too much (chest pain) but a week or two after the pill all my symptoms dissolve! I sleep like I used to, my face slims out, my hair grows back, my muscles fill in – I see myself starting to heal. But one pill shouldn’t have that effect unless it might not be safe. I don’t want to be stuck between diseases (hyper or hypo) I know you can’t give me medical advice, but I’ll ask – Do you know of anyone that takes one pill a week? I’m considering a lower dose weekly. Thanks! Just desperately trying to get back to health and this is the best article I’ve seen for something no one seems to understand.
Kara, Thank you so much for sharing your journey, I’m glad the article was helpful! Some people with Hashimoto’s and a history of high cortisol or adrenal stress can be very sensitive to thyroid medications, even at low doses like 25 mcg of Tirosint. This sensitivity may cause symptoms of both hypo- and hyperthyroidism as your body adjusts. While daily dosing is standard, there are rare cases where less frequent or smaller doses are used under close medical supervision. The key is working with a practitioner who listens and adjusts based on both labs and how you feel. You’re doing an amazing job tuning into your body, keep advocating for yourself!
Can progesterone supplementation also cause central hypothyroidism?
Donna, At this time, there is no direct evidence linking progesterone supplementation to central hypothyroidism. Central hypothyroidism is a rare condition typically caused by issues with the pituitary or hypothalamus. While I’ve observed that certain hormones like pregnenolone and hydrocortisone may suppress the pituitary and contribute to this condition, I have not seen this effect documented with progesterone. As always, it’s important to work with your healthcare provider to monitor hormone levels and symptoms when using hormone therapies. Here is an article you might find helpful as well: https://thyroidpharmacist.com/articles/thyroid-condition-start-worsen-during-perimenopause/