I hear this story all the time: someone gets diagnosed with Hashimoto’s or hypothyroidism, relieved to finally have an answer to their frustrating symptoms. They feel hopeful and excited as they start thyroid medication. They’re patient, thinking it will take some time for the medication to kick in. Maybe they start feeling a little bit better, but a few months into treatment, they’re more or less struggling with the same symptoms as before – fatigue, brain fog, hair loss.
Even with dose adjustments, they still don’t feel like how they had hoped.
One of the reasons for not feeling well on thyroid medication is the type of medication prescribed.
Levothyroxine is the generic name of a synthetic version of the thyroid hormone thyroxine, referred to as T4. In an extensive survey done in 2014 (and published in 2018), it was the second most prescribed drug in the United States. It is among the most widely prescribed medications in the world. [1]
For some people, it’s tremendously helpful for their symptoms, and for others, it doesn’t move the needle much. Thyroid medication can be a very important part of many people’s healing journeys, as it can help them get back to a baseline of feeling well, so that they actually have the energy to address their root causes!
T4 is a prodrug and needs to be converted to T3, the active thyroid hormone in the body. This conversion process doesn’t always happen well, and thus some people are not able to adequately convert T4 to T3 within their bodies. This can result in inadequate treatment and ongoing symptoms.
Those of us with Hashimoto’s may have a particularly difficult time converting T4 to T3, for reasons that we’ll cover in this article.
Some people benefit from adding in a T3 medication or switching to a T4/T3 combination medication such as Natural Dessicated Thyroid (NDT), but this isn’t always possible, and some people don’t tolerate T3-containing medications very well. Others may not have access due to where they live or the physicians they work with, who may not be familiar with how to prescribe T3-containing meds. Moreover, the FDA has recently reported that they will start “taking action” against NDT medications, so the future availability of these thyroid meds is uncertain.
The good news is that there are many things you can do to support the T4 to T3 conversion process naturally, and help maximize the effectiveness of your T4 medication. I want to make sure you get the most from your thyroid meds, regardless of which ones you are using!
In this article, you’ll discover:
- How the right testing can give you valuable insight into this conversion process
- The many reasons someone may not convert T4 to T3 well
- How to support this conversion process to get the most benefits from your T4 medication
T4 and T3 Overview
T4 (thyroxine) and T3 (triiodothyronine) are the two main thyroid hormones. T4 is known as a prohormone and is 300 percent less biologically active than T3. T3 is the main biologically active thyroid hormone that gives us beautiful hair, replenishes our energy, and runs our metabolism. [2]
The conversion of T4 to T3 is a complex process that relies on several key factors. It’s estimated that over 50 percent of this conversion occurs in the liver, while about 20 percent occurs in the gut. [3] The rest occurs in the kidneys and other tissues.
Adequate liver function is essential, as the liver contains deiodinase enzymes responsible for converting T4 to T3. [4] Nutrients such as selenium, zinc, and ferritin are critical for this enzymatic activity. Additionally, adequate levels of vitamins A and D support thyroid hormone metabolism.
A healthy gut microbiome also plays a role, as gut bacteria assist in the conversion process. Inflammation, chronic stress, or poor gut health (e.g., dysbiosis or leaky gut) can impair this conversion.
Overall, optimal T3 levels depend on sufficient nutrient status, a well-functioning liver and gut, and balanced adrenal and stress hormone levels. We’ll explore more of each of these factors in this article.
How Do I Know If I’m Converting Well?
The standard TSH test can’t tell us if we are converting T4 to T3 well. A full thyroid panel that measures free T4 and free T3 will give us better insight into how well we are converting.
In general, if your free T4 is normal or high, and your T3 is low or borderline, this is a red flag that you’re not converting well – but there can be some nuances to this as well. Here’s a little more information about these tests and how to interpret them:
Recommended tests: Free T3 and Free T4
The reference ranges for free T3 and free T4 are usually expressed in pmol/L or ng/dL, and the standard reference ranges can vary depending on the lab. Some labs even break them down by age.
Ideally, you should be getting both of these tests and looking at them together to see if you are properly converting T4 to T3, and if you are under- or overdosed on either T4 or T3 hormones (or both).
Because there’s some confusion about how to convert the different reference ranges, and I would rather have you become an expert in understanding your labs, rather than in pharmaceutical/medical calculations, I will share a method that integrative pharmacists use to determine if someone is converting their T4 to T3 well, regardless of the reference range.
Let’s use the Ulta Labs reference ranges with my results from 2022 – when I was having hair loss while taking Tirosint, which had worked well for me previously – as an example.
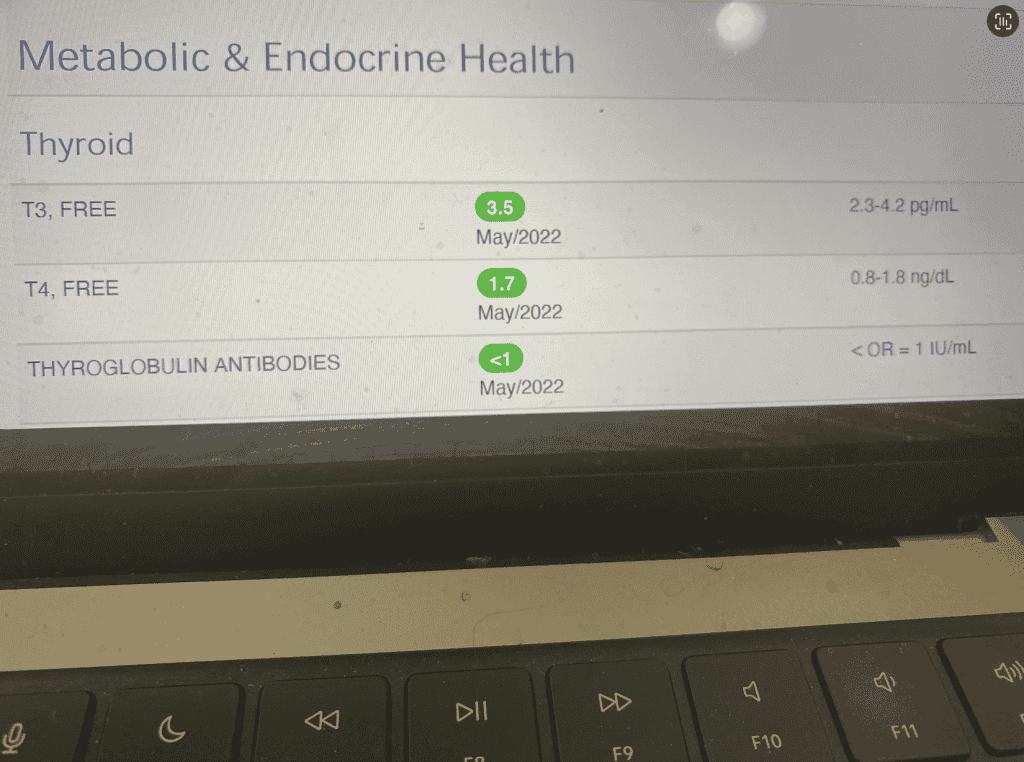
Ulta Labs Free T4 reference range: 0.8 to 1.8 ng/dL
(My Free T4 result was 1.7 pg/mL.)
Ulta Labs Free T3 reference range: 2.3 to 4.2 pg/mL
(My Free T3 result was 3.5 pg/mL.)
Using the Thyroid Gradient (see image below), you will draw two “gradients” (half circles), one for free T4, one for free T3.
On the left-hand side of each gradient, you will write the low number of the respective reference range. On the right-hand side, you will write the top number of the reference range.
You will then find your results, and draw a dot pointing to the space where your results are, and draw an arrow from the center of the bottom of the gradient, to the top of the arch, to meet your results.
Ideally, you want to have both your T3 and T4 somewhere in the middle of that reference range (though some feel better in the top half of the reference range), and you want to have both arrows pointing in the same direction. When they are both roughly in the same direction, there is adequate T4 to T3 conversion.
As you can see, my arrows did not line up, and my T4 to T3 conversion wasn’t terrible, but it wasn’t optimal. As mentioned before, I was taking Tirosint, which had previously been working well for me, but I was experiencing hair loss.
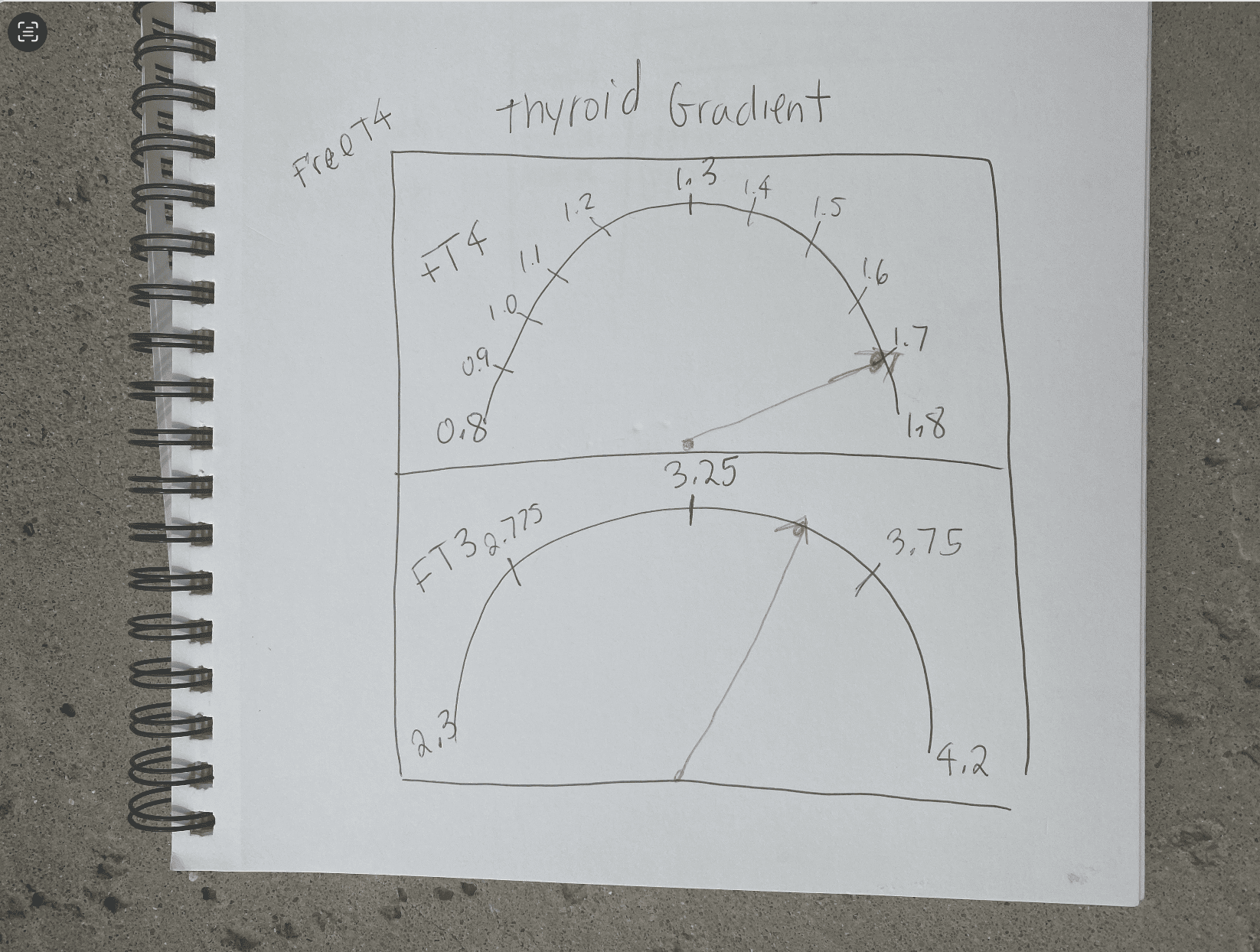
Please note, this gradient initially came to my attention via ZRT Lab and Jim Paoletti, RPh, in a training on thyroid disorders for pharmacists, but I am not sure who the original creator of it is. [5]
(As a side note – why was I losing my hair, and why was my conversion impacted? The clue was in another test I did, the ferritin test. Low ferritin levels can lead to hair loss and poor T4 to T3 conversion. More on this later on.)
How often you should test: I recommend testing every four to six weeks when starting a new medication, adjusting dosage, or experiencing symptoms, every two to three months if tracking the impact of lifestyle changes, and then every six to 12 months once symptoms are stable.
Things to consider before testing: I recommend testing your free T3 and free T4 early in the morning, and delaying your thyroid hormones until after taking the test to ensure accurate results (especially if you are taking T3-containing medications). Taking your medications before the test can result in a falsely elevated T3 (and sometimes T4), making it look like you are overmedicated when you are not. Additionally, the supplement biotin, commonly used for hair loss, can also falsely increase both T4 and T3 levels, making it look like you are overmedicated or like you are hyperthyroid. The American Thyroid Association recommends patients stop taking biotin at least two days before a T4 and T3 test.
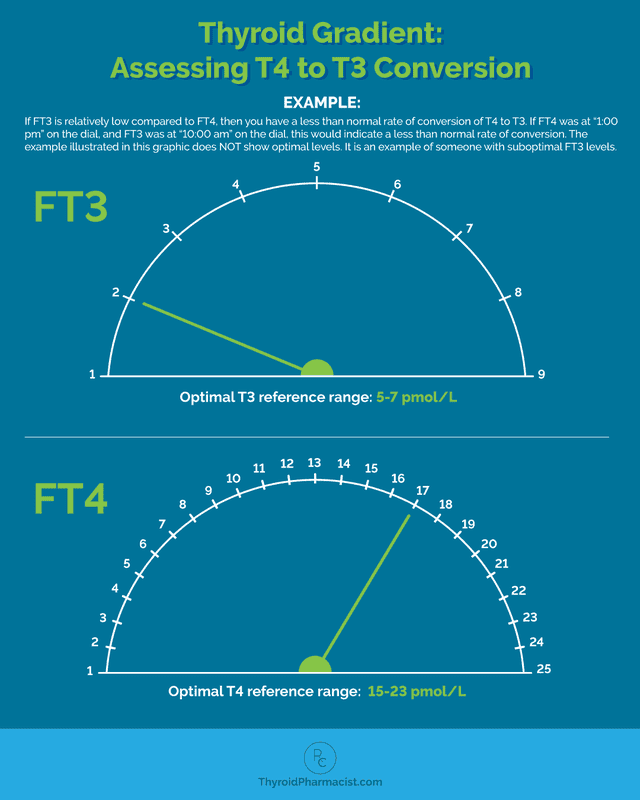
The reverse T3 (rT3) test measures how much of the active free T3 hormone is able to bind at thyroid receptors.
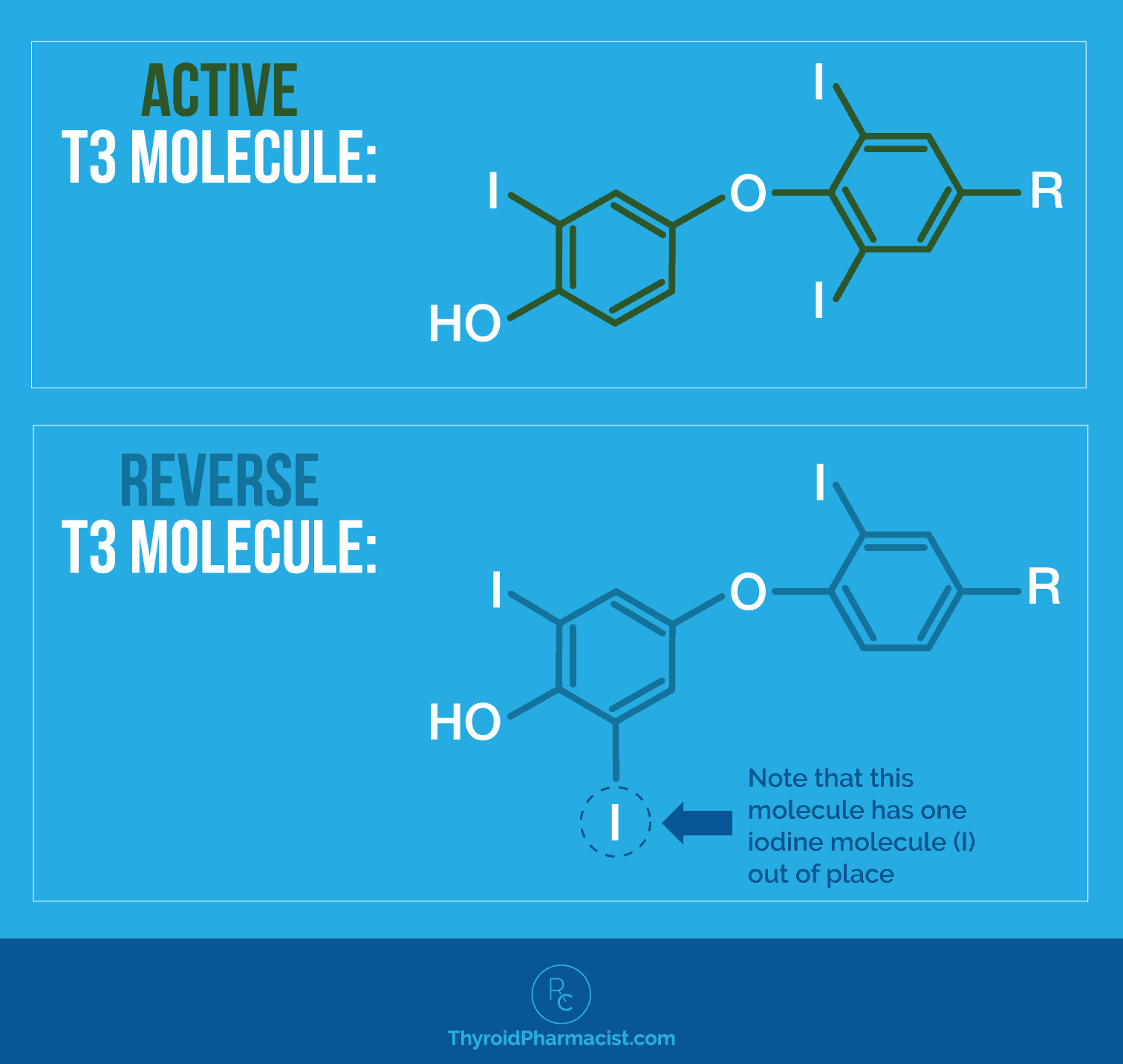
RT3 is produced in stressful situations and binds to thyroid receptors, but turns them off instead of activating them. (Stress is a common cause of low T4 to T3 conversion. Under stressful situations, T4 gets converted to reverse T3 instead of to T3. Reverse T3 is an inactive molecule related to T3, but without any physiological activity.) [6]
The rT3 test is sometimes used to identify cases of poor T4 to T3 conversion, as well as thyroid symptoms that are due to adrenal stress, instead of thyroid malfunction or autoimmunity.
However, in most cases, this test doesn’t change my other recommendations, so I consider this an optional test. The free T4/free T3 test is more useful for me to determine if a person is properly converting thyroid hormones.
When assessing your rT3 results, it is important to watch for trends of your levels going up. This usually indicates your body is reacting to a stressful situation. Your body produces rT3 to give it a break and to prevent you from becoming hyperthyroid. This is an evolutionary adaptation to slow your metabolism in times of famine (for more information on this, take a look at my Safety Theory).
Recommended tests: Reverse T3 (rT3)
Optimal rT3 reference range: Between 11 and 18 ng/dL
How often you should test: Every six months, if recommended by your integrative physician.
Why T4 Doesn’t Work for Everyone
As mentioned, T4 medications unfortunately don’t work for everyone. There are a few main reasons as to why they don’t always produce the intended effect.
Absorption Issues
Our thyroid medications can only work if we’re actually absorbing them! I’m always shocked to find out how many people were not properly instructed on how to take their thyroid medication.
Some of the fundamental guidelines for ensuring proper medication absorption are:
- Take your thyroid medication first thing in the morning on an empty stomach (you can have some lemon water alongside it to support absorption).
- Wait 30-60 minutes before consuming any other beverages, food, supplements, or medications (and yes, this includes coffee!).
- Some medications and supplements will need to be spaced even further from thyroid medication. Avoid magnesium, calcium, and iron supplementation within four hours of taking thyroid medication.
In some cases, absorption issues may also occur due to low stomach acid, IBS/SIBO, celiac or gluten sensitivity, PPIs, and even because of drinking coffee a few hours after taking meds. In that case, you may benefit from a levothyroxine (T4) gel-cap formulation, such as Tirosint (see my full article to learn more). I switched to Tirosint when I was a new mom with fluctuating thyroid levels and wasn’t willing to give up or move my coffee to later in the day. 😉
I have found that some of my clients experience sensitivities and adverse reactions to the many inactive ingredients or fillers found in their T4 medications. These are added as bulking agents used to stabilize the tablets, as coloring agents, as preservatives, or to aid in the manufacturing process in some way. Many have been shown to potentially cause adverse reactions, as well as affect the absorption rate and effectiveness of the very medication meant to help the thyroid.
Most generic levothyroxine products contain lactose (the generic manufactured by Mylan is, however, lactose-free) and not all are gluten-free (examples: Lannet does not contain gluten, per se, but the maker does not certify it as gluten-free; Mylan does certify their product as gluten-free).
Can small amounts of these types of fillers really be problematic? Yes! Many people with Hashimoto’s have sensitivities to these ingredients, even when exposed to tiny amounts. In my 2015 survey of 2,232 readers, 57 percent of respondents said they reacted to or avoided all dairy, and over 75 percent avoided gluten due to sensitivities and reactions. Other fillers that are commonly found in T4 medications may include confectioners’ sugar (which contains corn starch – corn is another food sensitivity for many people with Hashimoto’s), sucrose, talc, and dyes.
For some people, this is, again, a place where Tirosint might be of benefit. Additionally, looking for medications without the fillers that you are sensitive to, or trying compounded thyroid medications may also be an option.
Conversion Issues
One of the biggest reasons why some individuals may not have a full therapeutic response to T4-only thyroid hormones (even when dosed and taken correctly) can be due to the person’s ability to convert T4 to T3. (This is not just specific to the generic version of levothyroxine, by the way. It applies to all T4 medications.)
As I mentioned, this is because levothyroxine contains the less-active but longer-acting T4 hormone, which needs to be converted to T3, the more active thyroid hormone, by our bodies.
In 2014, Dr. Wilmar Wiersinga, a Dutch endocrinologist and top thyroid researcher, stated that: “Impaired psychological well-being, depression or anxiety are observed in 5-10 percent of hypothyroid patients receiving levothyroxine, despite normal TSH levels. Such complaints might hypothetically be related to increased free T4 and decreased free T3 serum concentrations, which result in the abnormally low free T4/free T3 ratios observed in 30 percent of patients on levothyroxine. Evidence is mounting that levothyroxine (T4) monotherapy cannot assure a euthyroid state in all tissues simultaneously, and that normal serum TSH levels in patients receiving levothyroxine reflect pituitary euthyroidism alone.” In other words, this study suggested that T4-only therapy might not be enough to address the symptoms of hypothyroid patients, especially those related to mental well-being.
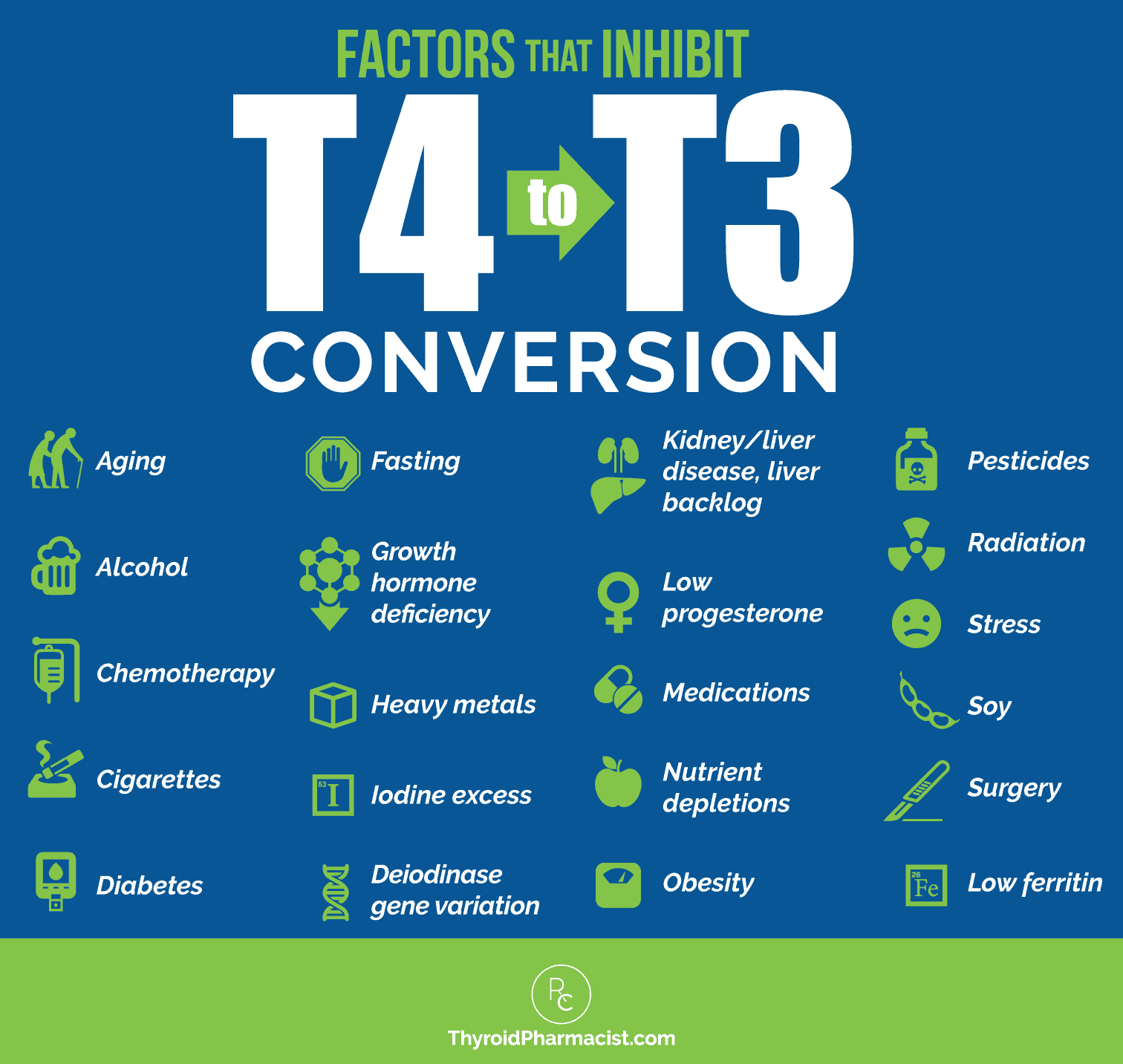
The conversion from T4 to T3 can be impeded by numerous factors. Some of the most impactful factors (that we can change!) include:
- Nutrient deficiencies (like zinc, selenium, and ferritin/iron)
- Impaired liver function
- Poor gut health (including dysbiosis and infection)
- Stress
I will explore each of these factors more in-depth in the next section.
Other potential factors impacting T4 to T3 conversion include:
- Aging
- Alcohol [7]
- Chemotherapy [8]
- Cigarettes [9]
- Deiodinase gene variation
- Diabetes [10]
- Fasting and calorie restriction [11]
- Growth hormone deficiency [12]
- Heavy metals [13]
- Iodine excess [14]
- Kidney and liver disease [15]
- Low progesterone [16]
- Medications
- Obesity [17]
- Pesticides [18]
- Radiation [19]
- Soy [20]
- Surgery [21]
Furthermore, in recent years, pharmacogenomics (the study of how a person’s genes impact their response to medications) has helped us determine which patients may best benefit from particular medications due to their unique genes.
From a pharmacogenomic standpoint, polymorphisms (variations) in the DIO2 deiodinase gene, which codes for the deiodinase 2 enzyme (Thr92Ala), can also lead to inadequate conversion of T4 to T3.
The thyroid gland plays a minor role in the daily production of T3, with the bulk of it being produced by two deiodinase genes (D1 and D2) that convert T4 to T3 outside the thyroid tissue. Thus, variations in these genes can impact how well the body is able to produce T3. Studies have shown that hypothyroid patients maintained on levothyroxine depend on D2 for more than 80 percent of all their T3 needs. [22] Thus, they are at much greater risk of developing low serum T3, especially during caloric restriction when the body acts to limit caloric expenditure, and temporarily slows metabolic function.
In one study suggesting a genetic link to poor ability to convert T4 to T3, a polymorphism in the DIO2 gene was found to be linked to who will or won’t respond well to T4 therapy (due to how well their body converts T4 to T3). [23] Findings, however, are still viewed as controversial, and more studies are required.
If you have challenges converting T4 to T3, you might want to consider a genetic test with Nutrition Genome.
It’s worth noting that many of the reasons people have poor conversion are also common triggers for Hashimoto’s. I believe this is one reason many of my clients do not do well on T4-only medications.
How to Get the Most from Your T4 Medication
You may consider adding a T3-containing medication, which you can learn more about in this article on different thyroid medication options. This is an option to discuss with your doctor.
However, some people may not have access to T3 medications for various reasons, and some people don’t do well on them, so I find that supporting the body’s natural conversion process can be really valuable in these situations.
Now, let’s address some of those bigger issues that we’ve touched on. Addressing the following factors will set you up for success and help support your body’s natural T4 to T3 conversion process.
1. Nutrient Deficiencies
Certain nutrients are needed in the conversion process, and some act as cofactors to enzymes that facilitate thyroid hormone conversion. It’s essential to make sure you have enough of these nutrients on board. These nutrients are also commonly deficient in those with Hashimoto’s.
- Ferritin/Iron: As mentioned earlier, T3 is sometimes called our “go” hormone because it tells our body to boost metabolism, grow hair, and create more energy. Without proper levels of ferritin (the iron storage hormone), the conversion of T4 to T3 can be impeded. [24] A 2018 study found that in women with persistent symptoms of hypothyroidism despite levothyroxine therapy, two-thirds were able to eliminate their symptoms when they got their ferritin levels over 100 µg/l. [25]
While the normal ferritin lab range for women is between 12 and 150 ng/mL, I’ve found that the optimal level for our thyroid is between 90 and 110 ng/mL. (When it comes to hair loss, some experts feel that ferritin levels of at least 40 ng/mL are needed to stop hair loss, and that a level of at least 70 ng/mL is needed for hair regrowth.) You can request ferritin testing from your doctor, or you can order your own test through Ulta Labs. Iron-boosting strategies include incorporating more red meat and organ meats into your diet, supporting stomach acid production (to assist with absorption), and iron supplements. Please see my full article on iron and ferritin for more information on optimizing ferritin/iron. I don’t recommend supplementing with iron unless you test!
- Selenium: The antioxidant selenium is required during the thyroid hormone conversion process, its role being to neutralize the toxic build-up of hydrogen peroxide (H2O2), which is a by-product of the hormone conversion. [26] Selenium also happens to be a very important nutrient for the thyroid itself, and has been shown to reduce thyroid antibodies at a dose of 83 mcg to 200 mcg per day. [27] This is a very common deficiency in those with Hashimoto’s. Selenium has a narrow therapeutic index, and doses of under 100 mcg per day may not be sufficient for improving Hashimoto’s symptoms and markers, while doses in excess of 800 mcg per day can be toxic. [28] Please read my full article on selenium for more information.
- Zinc: A depletion in zinc prevents the conversion of the T4 hormone into the active T3 version. Zinc is also needed to form TSH, which is why those with hypothyroidism and who are constantly producing TSH, are more likely to develop deficiencies in this important mineral. [29] It’s also very important for gut health, immune function, and tissue healing. [30] Over 52 percent of my surveyed readers reported feeling better after starting zinc supplementation. See my full article on zinc to learn more.
- Vitamin D: There is a strong link between low vitamin D levels and autoimmune disease, and it also plays a role in the thyroid conversion process. [31] Many people with Hashimoto’s have low vitamin D levels. In fact, 67 percent of my readers with Hashimoto’s reported an improvement in fatigue when they took a vitamin D supplement. You can work with your doctor to have your vitamin D levels checked, or you can self-order a vitamin D test. In addition to spending more time in the sunshine, a vitamin D supplement is helpful for many people in boosting levels. Pure Encapsulations Vitamin D 5000 IU (without Vitamin K) and Designs for Health Vitamin D Supreme (with Vitamin K) are two high-quality options. See my full article on vitamin D for more information and dosing recommendations.
- Vitamin A: Vitamin A is supportive of the thyroid, as it helps keep the immune system balanced, and it’s also involved in the activation, proliferation, and differentiation of regulatory T cells. [32] Vitamin A deficiency can lead to structural and functional changes of the thyroid gland, and it also acts as a free radical scavenger, reducing oxidative stress on the thyroid. [33] A high-quality supplement like this one from may be helpful.
2. Liver Support
Since the body produces the active T3 hormone through a conversion process from either endogenous T4 that’s produced in the body or exogenous T4 that is taken as a medication, having a healthy liver means that our bodies can utilize our own thyroid hormones, as well as our thyroid medication, much more efficiently! This means more energy, better hair growth, and even effortless weight loss for some!
When the liver is impaired, usually due to an accumulation of toxins or a lack of nutrient absorption, we are unable to complete the process. I suggest liver support as a first step for nearly everyone with Hashimoto’s, as it helps people feel better quickly.
Here’s an overview of the four steps to my Liver Support Protocol:
- Remove potentially triggering foods such as gluten, dairy, and soy.
- Add in liver-supportive foods such as hot lemon water, beets, cruciferous vegetables, cilantro, fermented foods, green juices or chlorophyll, turmeric, and berries.
- Reduce toxic exposure. Our modern world exposes us to an unprecedented number of toxins every day. Common products that we use every day, like household cleaning supplies and personal care products, are packed with toxins. Using an air filter and a water filter are good first steps, and check out my article on things to do to lower your toxic burden for some ideas for non-toxic swaps.
- Support detoxification pathways. Focusing on ways to support the lymphatic system can help your body transport and eliminate toxins. Exercise, dry brushing, lymphatic massage, sauna use, and supplements such as NAC and Liver Reset, can help gently support detoxification pathways.
For more information about the liver and thyroid connection, my article on liver support is a good starting point. For a more detailed liver support protocol, see my book Hashimoto’s Protocol. For even more support, I highly recommend my Root Cause Reset program, which guides you through the liver support protocol in great detail, with a lot of support and resources.
3. Gut Support
We know that everyone with Hashimoto’s (and autoimmune conditions in general) has some degree of intestinal permeability. [34] Given that about 20 percent of the conversion of T4 to T3 takes place in the gut, improving gut health can help with the conversion process and improve T3 levels.
For many, the problem lies in the imbalance of beneficial to opportunistic bacteria in the gut microbiome, also known as gut dysbiosis, and getting a quality probiotic on board can help improve gut health and increase T3 levels.
A good starting point would be a high-dose probiotic that contains the beneficial Lactobacillus bacteria (which many with Hashimoto’s are low in – a common pattern I see on gut tests). Some high-quality options are Rootcology ProB 50, Pure Encapsulations Probiotic 50B, or Klaire Ther-Biotic (available via Fullscript – if you don’t have a Fullscript account, you can sign up with my credentials here).
High-dose, multi-strain probiotics can be very helpful for people with Hashimoto’s in general, and especially for those who often show low levels of them on gut lab tests. However, they may be problematic for people with SIBO, which can be caused by an overgrowth of various bacteria. It’s important to note that up to 50 percent of people with Hashimoto’s may have SIBO. For those with SIBO, I suggest a beneficial yeast called S. boulardii.
Learn more about supporting the gut in this article and more about the best probiotics for Hashimoto’s in this article. My new IBS Book offers a structured and supportive way to help you restore optimal gut function.
4. Adrenal Support
Stress is another very common cause of low T4 to T3 conversion. Under stressful situations, T4 gets converted to reverse T3 instead of T3. Reverse T3 is an inactive molecule related to T3, but without any physiological activity. (It essentially just takes up space!)
I find adrenal dysfunction to be incredibly common in my patients with Hashimoto’s. In fact, in my survey of over 2,230 people with Hashimoto’s, 69 percent reported a lot of stress in their lives before they began to feel unwell.
The six main pillars I use in adrenal support include:
- Rest
- Balance blood sugar
- Reduce stress
- Reduce inflammation
- Replenish nutrients and electrolytes
- Build resilience with supplements
You can read more about these pillars in my article on the adrenals, and I outline my full protocol in my book Adrenal Transformation Protocol. If you’re looking for guided support, check out my Fatigue and Brain Fog Fix in Six: Thyroid Adrenal Edition program, which has helped thousands of my readers feel better. In fact, 92 percent of participants reported reduced mental fog, 89 percent had reduced fatigue, and 86 percent had reduced anxiety.
5. Optimize Progesterone
Progesterone plays a key role in the conversion of T4 to the active T3 hormone by counterbalancing the effects of estrogen. When there is estrogen dominance, this can result in poor T4 to T3 conversion, leading to thyroid symptoms. Estrogen dominance may be the result of low progesterone levels in general, or sometimes a woman will have normal progesterone levels and too much estrogen. Additionally, progesterone has anti-inflammatory and calming effects on the body, helping to reduce stress, which is another factor that can hinder T4 to T3 conversion.
If you’ve found that your thyroid symptoms got worse around perimenopause, declining levels of progesterone may be an underlying reason.
For women, checking and optimizing progesterone levels is another important step in improving thyroid hormone conversion. See my article on estrogen dominance for more information on testing and balancing hormones.
Beyond optimizing conversion, some individuals may benefit from switching to T4/T3 medications. Of the readers I’ve surveyed, up to 60 percent have felt better taking a combination T4/T3 medication, while around 40 percent have felt better on a synthetic T4 medication. I used to routinely recommend T4/T3 medications for my clients, however, three of the four available brands have recently been recalled in the United States. For more information about the types of medications available, see this article.
Ensuring proper thyroid medication absorption, checking for problematic fillers, and supporting your body’s natural T4 to T3 conversion process can make a significant difference, especially for those who don’t have access to T3 medications or don’t tolerate them well.
Addressing nutrient deficiencies, improving liver and gut function, and supporting adrenal health are foundational strategies that can help enhance this conversion and reduce lingering symptoms. Now that we’ve explored these underlying factors, let’s take a closer look at targeted supplements that can further support and optimize the T4 to T3 conversion process.
Supplements that Support Conversion
In addition to addressing the key factors listed above, there are some supplements that I’d like to highlight, as they have been found especially effective in supporting T4 to T3 conversion. I’ve included a variety of formulations, as we all have individual needs based on our unique health stories. Be sure to note the differences between formulas and consult with a healthcare professional to help decide which one is most appropriate for you.
Guggul
Guggul is the gum resin obtained from two different plants, Commiphora and Boswellia. It contains many phenolic compounds, which possess substantial anti-inflammatory and antioxidant effects. [35]
You’ve likely never heard of guggul (Google it! ;-)), but it has been found to provide support in a number of conditions, including acne, arthritis, IBD, diabetes, psoriasis, respiratory diseases, and even cancer. [36] Along with its anti-inflammatory effects, it has hepatoprotective (liver protective), cardioprotective, neuroprotective, and hypolipidemic (low blood lipid) properties as well.
Preliminary research suggests that guggul (gum resin extracted from plants) helps to maintain healthy thyroid function by supporting healthy iodine utilization and thyroid hormone conversion.* [37] Research with mice showed that it has the potential to ameliorate hypothyroidism. [38]
It’s available as a supplement, like the one from Himalaya Wellness (available via Fullscript; if you don’t have a Fullscript account, you can sign up with my credentials here). I’ve also added it to my new product, Rootcology’s Thyroid Conversion Support (more on this below).
Please note that guggul is not recommended if you are pregnant or lactating; it appears to stimulate the uterus, and not enough is known about its safety. Guggul may have an estrogen-like effect on the body, so it may not be appropriate for people with certain hormone-sensitive conditions such as breast cancer. Please consult with your doctor before use.
Ashwagandha
Ashwagandha is a popular adaptogenic herb found to have many anti-stress properties, along with being neuroprotective, anti-arthritic, anti-inflammatory, and analgesic. Unlike some adaptogens, it has more of a calming effect.[39] Adaptogens are natural substances that help the body resist stress and maintain balance.
I have found it to be extremely helpful for those who are fatigued during the day but have a hard time sleeping at night – AKA those of us who sometimes find ourselves “wired and tired” (a hallmark symptom of adrenal dysfunction). It is my favorite adaptogenic herb for Hashimoto’s.
In my clinical practice, I have seen ashwagandha help normalize thyroid hormone levels in cases of subclinical hypothyroidism. In one small study published in 2017 in The Journal of Complementary Medicine, after eight weeks of treatment, ashwagandha was found to improve serum TSH, T3, and T4 levels, normalizing serum levels. [40] Ashwagandha may support the conversion of T4 to T3 by reducing stress and lowering cortisol levels, which can otherwise inhibit this conversion.
If you are looking for a stand-alone ashwagandha supplement, Ashwagandha by Pure Encapsulations is a good option. I’ve also included it in Rootcology’s Adrenal Support and Rootcology’s Thyroid Conversion Support.
Precautions: Ashwagandha should not be taken by pregnant or lactating women. It may be contraindicated for individuals who have allergic reactions to nightshades (eggplant, bell peppers, white potatoes, tomatoes, cayenne pepper, etc.). People taking immunosuppressant medications or sedatives should consult with their practitioner in regards to any potential contrary effects. If you are taking thyroid medications, be sure to monitor your thyroid function with your practitioner, as ashwagandha can increase thyroid hormone levels, and your needs for thyroid hormones may decrease.
Rootcology Thyroid Conversion Support
For many years, I had a hard time finding a comprehensive supplement for thyroid hormone conversion that checked all my boxes. There are some excellent options, which I’ll outline below, though not all may be suitable for every individual or group. So I decided to create my own!
Thyroid Conversion Support is a specialized blend of nutrients and herbs designed to promote healthy biosynthesis of thyroid hormone, including the conversion of T4 to T3.*
It contains these key nutrients:
- Vitamin A – Vitamin A deficiency can lead to structural and functional changes of the thyroid gland, and it also acts as a free radical scavenger, reducing oxidative stress on the thyroid.* [41]
- Vitamin D3 – Research has shown that low levels are associated with increased self-tissue response (meaning your body is more likely to launch an immune attack on itself), and it plays a role in immune system balance.* [42]
- Vitamin E – May help protect thyroid cells/tissue and also supports the enzymatic conversion of T4 to T3 by scavenging damaging free radicals.* [43]
- Iodine – While iodine deficiency can lead to hypothyroidism and poor T4 to T3 conversion, excess iodine has been implicated as a trigger for autoimmune thyroid diseases, so I consider it a narrow therapeutic index nutrient. The small dose (75 mcg) in this formulation provides support without triggering the autoimmune inflammation a person would see with high doses (above 300 mcg per day).* [44]
- Zinc – Zinc is required for the conversion of T4 to T3, and is needed to form TSH.* [45]
- Selenium – Essential for the function of deiodinase enzymes involved in converting T4 to T3. Selenium also helps to protect the thyroid from oxidative stress as a result of this process. Selenium is also a narrow therapeutic index nutrient (a dosage of 83-400 mcg per day is usually recommended; above 800 mcg can be toxic). I added 100 mcg here, so it isn’t excessive even if you take another supplement that contains 83-200 mcg.* [46]
- Guggul extract – Preliminary research suggests that guggul (gum resin extracted from plants) helps to maintain healthy thyroid function by supporting healthy iodine utilization and thyroid hormone conversion.* [47]
- Rosemary extract – Like vitamin E, rosemary acts as an antioxidant and may help protect thyroid cells/tissue; it also supports the enzymatic conversion of T4 to T3 by scavenging damaging free radicals.* [48]
- Ashwagandha – Preliminary research suggests that ashwagandha helps to maintain healthy thyroid function and reduces oxidative stress. It’s also an adaptogen and supports adrenal health by supporting healthy cortisol levels.* [49]
Also, because I know what it’s like to have a supplement graveyard with supplements that I tried but found didn’t work for me or caused me to have reactions, Rootcology offers a full refund on all supplements within 30 days, so if the supplement doesn’t work for you, you can return it for a full refund.
Pure Encapsulations Thyroid Support Complex
This is another great option! The ingredients are similar to the Rootcology option above, but there are some key differences, which I will highlight below.
Thyroid Support Complex includes:
- Vitamin A
- Vitamin C – For additional antioxidant support.
- Vitamin D
- Iodine – This formulation contains 150 mcg of iodine, which is more than the Rootcology formulation, but is still an appropriate amount for someone with Hashimoto’s. I generally caution against doses above 200 mcg per day, unless pregnant or breastfeeding (keep in mind this includes iodine found in foods).
- Zinc
- Selenium
- L-tyrosine – This amino acid is a key component in the synthesis of thyroid hormones.
- Ashwagandha
- Forskohlii – Also known as Coleus barbatus, this extract has been shown to promote adenylate cyclase activity, supporting thyroid hormone metabolism. [50]
- Guggul – This formulation also contains guggul, but at a lower dose (50 mg vs. 500 mg in the Rootcology formulation).
- Turmeric – This formulation includes turmeric, which can neutralize free radicals that affect iodothyronine 5’-monodeiodinase enzyme activity, the limiting factor in the conversion of T4 to the more active T3 hormone. [51]
Pure Encapsulations is another great choice for thyroid hormone conversion support.
Designs for Health Thyroid Synergy
Thyroid Synergy by Designs for Health is another blend designed to support thyroid health and T4 to T3 conversion, and contains many of the nutrients that have been mentioned in this article, plus some other trace minerals like copper, manganese, and chromium. This is an overall great blend, but the selenium is a bit on the low end, and the copper content may not be ideal for certain individuals. Copper toxicity is a common issue in Hashimoto’s that I personally experienced (I wrote about it in my book Hashimoto’s Protocol and hope to have an article about it soon), and I generally advise against supplemental copper unless there is a known deficiency. (Symptoms like anxiety, insomnia, racing thoughts, PMS/PMDD, headaches, skin breakouts, and stubborn fatigue – frequently alongside thyroid and adrenal sluggishness – are potential symptoms of copper toxicity).
Takeaway
If you’re taking levothyroxine or other T4 medications and still experiencing symptoms like fatigue, brain fog, or hair loss, impaired conversion of T4 to T3 may be a key factor. The good news is that by strategically supporting this conversion process, you can significantly enhance the effectiveness of your medication and start seeing real improvements in how you feel.
I recommend working through these steps to identify which interventions have the greatest impact on your thyroid function and overall well-being.
I’d love to know about your experience with thyroid medications, if you ever found T4 to T3 conversion to be an issue for you, and what helped you finally feel better.
As always, I wish you the very best on your health journey!
P.S. You can also download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free, by signing up for my weekly newsletter. You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow me on Facebook, Instagram, Pinterest, and TikTok!
References
[1] Jonklaas J, DeSale S. Levothyroxine prescriptions trends may indicate a downtrend in prescribing. Ther Adv Endocrinol Metab. 2020;11:2042018820920551. Published 2020 May 19. doi:10.1177/2042018820920551
[2] Shahid MA, Ashraf MA, Sharma S. Physiology, Thyroid Hormone. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 8, 2022.
[3] Bruinstroop E, van der Spek AH, Boelen A. Role of hepatic deiodinases in thyroid hormone homeostasis and liver metabolism, inflammation, and fibrosis. Eur Thyroid J. 2023;12(3):e220211. Published 2023 Apr 13. doi:10.1530/ETJ-22-0211; Knezevic J, Starchl C, Tmava Berisha A, Amrein K. Thyroid-Gut-Axis: How Does the Microbiota Influence Thyroid Function?. Nutrients. 2020;12(6):1769. Published 2020 Jun 12. doi:10.3390/nu12061769
[4] Sabatino L, Vassalle C, Del Seppia C, Iervasi G. Deiodinases and the Three Types of Thyroid Hormone Deiodination Reactions. Endocrinol Metab (Seoul). 2021;36(5):952-964. doi:10.3803/EnM.2021.1198
[5] Pellegrino T. Thyroid Gradient Levels.
[6] Helmreich DL, Tylee D. Thyroid hormone regulation by stress and behavioral differences in adult male rats. Horm Behav. 2011;60(3):284-291. doi:10.1016/j.yhbeh.2011.06.003
[7] McGregor B. Extra-Thyroidal Factors Impacting Thyroid Hormone Homeostasis: A Review. Association for the Advancement of Restorative Medicine. December 1, 2015. Accessed September 26, 2025. https://restorativemedicine.org/journal/extra-thyroidal-factors-impacting-thyroid-hormone-homeostasis-a-review/.
[8] Huang J, Jin L, Ji G, et al. Implication from thyroid function decreasing during chemotherapy in breast cancer patients: chemosensitization role of triiodothyronine. BMC Cancer. 2013;13:334. Published 2013 Jul 6. doi:10.1186/1471-2407-13-334
[9] McGregor B. Extra-Thyroidal Factors Impacting Thyroid Hormone Homeostasis: A Review. Association for the Advancement of Restorative Medicine. December 1, 2015. Accessed September 26, 2025. https://restorativemedicine.org/journal/extra-thyroidal-factors-impacting-thyroid-hormone-homeostasis-a-review/.
[10] Kalra S, Aggarwal S, Khandelwal D. Thyroid Dysfunction and Type 2 Diabetes Mellitus: Screening Strategies and Implications for Management. Diabetes Ther. 2019;10(6):2035-2044. doi:10.1007/s13300-019-00700-4
[11] McGregor B. Extra-Thyroidal Factors Impacting Thyroid Hormone Homeostasis: A Review. Association for the Advancement of Restorative Medicine. December 1, 2015. Accessed September 26, 2025. https://restorativemedicine.org/journal/extra-thyroidal-factors-impacting-thyroid-hormone-homeostasis-a-review/.
[12] Jørgensen JO, Møller J, Laursen T, Orskov H, Christiansen JS, Weeke J. Growth hormone administration stimulates energy expenditure and extrathyroidal conversion of thyroxine to triiodothyronine in a dose-dependent manner and suppresses circadian thyrotrophin levels: studies in GH-deficient adults. Clin Endocrinol (Oxf). 1994;41(5):609-614. doi:10.1111/j.1365-2265.1994.tb01826.x
[13] McGregor B. Extra-Thyroidal Factors Impacting Thyroid Hormone Homeostasis: A Review. Association for the Advancement of Restorative Medicine. December 1, 2015. Accessed September 26, 2025. https://restorativemedicine.org/journal/extra-thyroidal-factors-impacting-thyroid-hormone-homeostasis-a-review/.
[14] Li N, Jiang Y, Shan Z, Teng W. Prolonged high iodine intake is associated with inhibition of type 2 deiodinase activity in pituitary and elevation of serum thyrotropin levels. Br J Nutr. 2012;107(5):674-682. doi:10.1017/S0007114511003552
[15] McGregor B. Extra-Thyroidal Factors Impacting Thyroid Hormone Homeostasis: A Review. Association for the Advancement of Restorative Medicine. December 1, 2015. Accessed September 26, 2025. https://restorativemedicine.org/journal/extra-thyroidal-factors-impacting-thyroid-hormone-homeostasis-a-review/.
[16] Gluck M. Estrogen dominance and hypothyroidism. The Marion Gluck Clinic. June 17, 2025. Accessed September 26, 2025. https://www.mariongluckclinic.com/blog/estrogen-dominance-hypothyroidism.html.
[17] Li Y, Zhang Q, Chen L, et al. Impaired sensitivity to thyroid hormones is associated with increased body fat mass/muscle mass ratio (F/M) in the euthyroid population. Diabetol Metab Syndr. 2025;17(1):128. Published 2025 Apr 15. doi:10.1186/s13098-025-01693-w
[18] Leemans M, Couderq S, Demeneix B, Fini JB. Pesticides With Potential Thyroid Hormone-Disrupting Effects: A Review of Recent Data. Front Endocrinol (Lausanne). 2019;10:743. Published 2019 Dec 9. doi:10.3389/fendo.2019.00743
[19] Patil N, Rehman A, Anastasopoulou C, Jialal I. Hypothyroidism. National Library of Medicine. February 18, 2024. Accessed September 26, 2025. https://www.ncbi.nlm.nih.gov/books/NBK519536/.
[20] Otun J, Sahebkar A, Östlundh L, Atkin SL, Sathyapalan T. Systematic Review and Meta-analysis on the Effect of Soy on Thyroid Function. Sci Rep. 2019;9(1):3964. Published 2019 Mar 8. doi:10.1038/s41598-019-40647-x
[21] Lee SH, Kang JG, Hahm MC, et al. Anesthetic experience in a clinically euthyroid patient with hyperthyroxinemia and suspected impairment of T4 to T3 conversion: a case report. Korean J Anesthesiol. 2014;67(2):144-147. doi:10.4097/kjae.2014.67.2.144
[22] Lipp HP. Administration and Pharmacokinetics of Levothyroxine. In: Kahaly GJ, ed. 70 Years of Levothyroxine. Cham (CH): Springer; March 12, 2021.13-22.
[23] Panicker V, Saravanan P, Vaidya B, et al. Common variation in the DIO2 gene predicts baseline psychological well-being and response to combination thyroxine plus triiodothyronine therapy in hypothyroid patients. J Clin Endocrinol Metab. 2009;94(5):1623-1629. doi:10.1210/jc.2008-1301
[24] Galton VA. Some effects of altitude on thyroid function. Endocrinology. 1972;91(6):1393-1403. doi:10.1210/endo-91-6-1393; Surks MI. Effect of thyrotropin on thyroidal iodine metabolism during hypoxia. Am J Physiol. 1969;216(2):436-439. doi:10.1152/ajplegacy.1969.216.2.436
[25] Rayman MP. Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease. Proc Nutr Soc. 2019;78(1):34-44. doi:10.1017/S0029665118001192
[26] Ventura M, Melo M, Carrilho F. Selenium and Thyroid Disease: From Pathophysiology to Treatment. Int J Endocrinol. 2017;2017:1297658. doi:10.1155/2017/1297658
[27] Gärtner R, Gasnier BC, Dietrich JW, Krebs B, Angstwurm MW. Selenium supplementation in patients with autoimmune thyroiditis decreases thyroid peroxidase antibodies concentrations. J Clin Endocrinol Metab. 2002;87(4):1687-1691. doi:10.1210/jcem.87.4.8421; Gärtner R, Gasnier BC. Selenium in the treatment of autoimmune thyroiditis. Biofactors. 2003;19(3-4):165-170. doi:10.1002/biof.5520190309
[28] Selenium. Institute of Medicine (US) Panel on Dietary Antioxidants and Related Compounds. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington (DC): National Academies Press (US); 2000.
[29] Severo JS, Morais JBS, de Freitas TEC, et al. The Role of Zinc in Thyroid Hormones Metabolism. Int J Vitam Nutr Res. 2019;89(1-2):80-88. doi:10.1024/0300-9831/a000262
[30] Stiles LI, Ferrao K, Mehta KJ. Role of zinc in health and disease. Clin Exp Med. 2024;24(1):38. Published 2024 Feb 17. doi:10.1007/s10238-024-01302-6
[31] Yang CY, Leung PS, Adamopoulos IE, Gershwin ME. The implication of vitamin D and autoimmunity: a comprehensive review. Clin Rev Allergy Immunol. 2013;45(2):217-226. doi:10.1007/s12016-013-8361-3; Babić Leko M, Jureško I, Rozić I, Pleić N, Gunjača I, Zemunik T. Vitamin D and the Thyroid: A Critical Review of the Current Evidence. Int J Mol Sci. 2023;24(4):3586. Published 2023 Feb 10. doi:10.3390/ijms24043586
[32] Capriello S, Stramazzo I, Bagaglini MF, Brusca N, Virili C, Centanni M. The relationship between thyroid disorders and vitamin A.: A narrative minireview. Front Endocrinol (Lausanne). 2022;13:968215. Published 2022 Oct 11. doi:10.3389/fendo.2022.968215
[33] Ibid
[34] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
[35] Kunnumakkara AB, Banik K, Bordoloi D, et al. Googling the Guggul (Commiphora and Boswellia) for Prevention of Chronic Diseases. Front Pharmacol. 2018;9:686. Published 2018 Aug 6. doi:10.3389/fphar.2018.00686
[36] Kunnumakkara AB, Banik K, Bordoloi D, et al. Googling the Guggul (Commiphora and Boswellia) for Prevention of Chronic Diseases. Front Pharmacol. 2018;9:686. Published 2018 Aug 6. doi:10.3389/fphar.2018.00686
[37] Panda S, Kar A. Guggulu (Commiphora mukul) potentially ameliorates hypothyroidism in female mice. Phytother Res. 2005;19(1):78-80. doi:10.1002/ptr.1602
[38]Ibid
[39] Singh N, Bhalla M, de Jager P, et al. An overview on ashwagandha: a Rasayana (rejuvenator) of Ayurveda. Afr J Tradit Complement Altern Med. 2011;8(5 Suppl):208-13
[40] Sharma AK, Basu I, Singh S. Efficacy and Safety of Ashwagandha Root Extract in Subclinical Hypothyroid Patients: A Double-Blind, Randomized Placebo-Controlled Trial. J Altern Complement Med. 2018;24(3):243-248. doi:10.1089/acm.2017.0183
[41] Capriello S, Stramazzo I, Bagaglini MF, Brusca N, Virili C, Centanni M. The relationship between thyroid disorders and vitamin A.: A narrative minireview. Front Endocrinol (Lausanne). 2022;13:968215. Published 2022 Oct 11. doi:10.3389/fendo.2022.968215
[42] Kivity S, Agmon-Levin N, Zisappl M, et al. Vitamin D and autoimmune thyroid diseases. Cell Mol Immunol. 2011;8(3):243-247. doi:10.1038/cmi.2010.73
[43] Macvanin MT, Gluvic Z, Zafirovic S, Gao X, Essack M, Isenovic ER. The protective role of nutritional antioxidants against oxidative stress in thyroid disorders. Front Endocrinol (Lausanne). 2023;13:1092837. Published 2023 Jan 4. doi:10.3389/fendo.2022.1092837
[44] Kalarani IB, Veerabathiran R. Impact of iodine intake on the pathogenesis of autoimmune thyroid disease in children and adults. Ann Pediatr Endocrinol Metab. 2022;27(4):256-264. doi:10.6065/apem.2244186.093
[45] Severo JS, Morais JBS, de Freitas TEC, et al. The Role of Zinc in Thyroid Hormones Metabolism. Int J Vitam Nutr Res. 2019;89(1-2):80-88. doi:10.1024/0300-9831/a000262
[46] Ventura M, Melo M, Carrilho F. Selenium and Thyroid Disease: From Pathophysiology to Treatment. Int J Endocrinol. 2017;2017:1297658. doi:10.1155/2017/1297658
[47] Panda S, Kar A. Guggulu (Commiphora mukul) potentially ameliorates hypothyroidism in female mice. Phytother Res. 2005;19(1):78-80. doi:10.1002/ptr.1602
[48] Nieto G, Ros G, Castillo J. Antioxidant and Antimicrobial Properties of Rosemary (Rosmarinus officinalis, L.): A Review. Medicines (Basel). 2018;5(3):98. Published 2018 Sep 4. doi:10.3390/medicines5030098
[49] Mikulska P, Malinowska M, Ignacyk M, et al. Ashwagandha (Withania somnifera)-Current Research on the Health-Promoting Activities: A Narrative Review. Pharmaceutics. 2023;15(4):1057. Published 2023 Mar 24. doi:10.3390/pharmaceutics15041057
[50] Laurberg P. Forskolin stimulation of thyroid secretion of T4 and T3. FEBS Lett. 1984;170(2):273-276. doi:10.1016/0014-5793(84)81327-7
[51] Samanta L, Panigrahi J, Bhanja S, Chainy GB. Effect of turmeric and its active principle curcumin on t(3)-induced oxidative stress and hyperplasia in rat kidney: a comparison. Indian J Clin Biochem. 2010;25(4):393-397. doi:10.1007/s12291-010-0046-6
https://www.dropbox.com/scl/fi/mu1i6gznovkeedflb4jge/TP-Infographics-Thyroid-Gradient-Assessing-T4-to-T3-Conversion-Filled-In.png?rlkey=7t5kcjo82iigk0r08td6il207&st=xvcbtu60&dl=0
https://www.dropbox.com/scl/fi/mnv1cf2qs5es9tdfrrc8c/TP-Infographics-T3.png?rlkey=zqi1f6hvnakkfeqio0i7gbbj2&st=de4e1yls&dl=0
https://www.dropbox.com/scl/fi/vwwzel6rq30cfbyf4a82v/TP-Pinterest-Factors-that-Inhibit-T4-T3-Conversion.png?rlkey=agqhowxcdjf3fusejs6ixa7is&st=e20cel5a&dl=0
https://www.dropbox.com/scl/fi/6s78txaabazql606c9vi0/RC-Thyroid-Conversion-Support-Front.png?rlkey=al9wyhy763kqv1l8uxlblamc7&st=kuy4vdx9&dl=0


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Could you address how to switch from NDT to Levothroxine and Liothyronine, in case the FDA does take away NDT? I am presently on Armour and Liothyronine because my doctor said I don’t convert T4 to T3 well. Unfortunately, my great thyroid doctor is no longer available to me so I have to figure this out alone.
Hi Lorraine, Thank you for sharing your situation! Switching from NDT to a combination of levothyroxine (T4) and liothyronine (T3) can be done, but it’s very individualized. Because everyone’s thyroid needs and T4-to-T3 conversion rates differ, it’s important to work with a knowledgeable practitioner to adjust doses safely. If your previous doctor isn’t available, consider finding a functional practitioner who is experienced in thyroid management and can help you transition gradually, monitor your labs, and track symptoms to ensure your thyroid levels stay balanced. Never make changes on your own, as thyroid dosing needs to be personalized for safety and effectiveness. Here is are some resources I hope are helpful:
A PHARMACISTS REVIEW OF MEDICATIONS
https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
Hello Dr. Wentz,
My TSH levels went up to 4.5 and my endocrinologist told me that it is normal for levels to go up as we age. I am 75. I am concerned. Is it normal? What can bring TSH levels down again?
Thank you!
Bonnie, Thank you for sharing this with me. I know it can feel concerning when labs shift. While TSH can rise a bit with age, a level of 4.5 may still point to suboptimal thyroid function for some people. Many feel their best when TSH is closer to 0.5–2.5, though this can vary.
Nutrients like selenium, zinc, and iron—as well as stress, inflammation, or gut and liver health, can all impact thyroid balance. It’s best to review your full thyroid panel (TSH, Free T4, Free T3, and antibodies) and symptoms with your practitioner to find what’s optimal for you. Here are a couple articles that I hope are helpful as well:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
PATIENTS WITH SUBCLINICAL HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/patients-subclinical-hypothyroidism-deserve-care-treatment/