There is a saying that I’m sure you’ve heard many times: “You are what you eat.”
And while that’s very true, I also like for people to remember: “You are what your body can digest, absorb and eliminate.” However, many people with Hashimoto’s may have issues related to these processes.
Specifically, many of my readers have been diagnosed with gallbladder issues, or have even had their gallbladder surgically removed. As a result, they find their ability to digest fats to be significantly impaired. These people suffer from a wide variety of symptoms, including diarrhea, nausea, belching, and stomach pain.
While you may think that the body’s inability to absorb fat sounds like a good thing weight-wise, it isn’t. We all need healthy fats in order to absorb vital fatty acids and other nutrients that our body needs. If our body isn’t able to absorb these nutrients, we should take that as a sign that there are other issues going on that are impacting us negatively as well.
I have found that difficulty with digesting fats (fat malabsorption) commonly affects 40 to 50 percent of people with Hashimoto’s. In fact, research has found links between thyroid disease, fat malabsorption, and gallbladder issues.
So let’s talk about fat malabsorption, the role of the liver and gallbladder in digesting fats and eliminating toxins, and how Hashimoto’s increases your risk of having these issues.
In this article, you will learn:
- How the liver and gallbladder affect one’s digestion of fats
- The link between fat malabsorption, gallstone disease, and Hashimoto’s
- Symptoms of fat malabsorption and gallbladder issues
- What to do if you don’t have a gallbladder
- The Root Cause Approach to addressing fat malabsorption, as well as liver and gallbladder problems
The Liver and Gallbladder’s Role in Healthy Fat Digestion
First, let’s talk about how the liver and gallbladder work together (along with the pancreas) to break down fats for healthy digestion, absorption, and elimination.
We know that whatever we eat eventually makes it down into the small intestine, which does most of the digestion, absorption, and elimination of food molecules.
Our small intestine is a very watery environment, and as fats do not dissolve in water, other digestive organs must step in to provide support and help to effectively digest fats.
To do this, our liver produces a substance called bile. Bile from the liver is sent to the gallbladder via a passageway called the common bile duct, and then it is concentrated and stored there.
When we eat a fatty meal, the concentrated bile is released from the gallbladder through the common bile duct, then heads to the duodenum, which is the initial part of the small intestine.
There, the bile begins to break down the fats into tiny globules.
At the same time, the neighboring pancreas organ releases its own pancreatic juices (containing digestive enzymes such as lipase and bicarbonate ions), mixing with the bile and tiny globules of fat. The pancreatic juices neutralize the digesting food (which is very acidic) and also help with protein and carbohydrate digestion.
Both bile and pancreatic secretions emulsify the fats (or lipids) so that they can be digested in the watery small intestine.
Here’s an analogy to help visualize the role of bile: bile acts like dish soap and works to dissolve globs of fat (picture fats that are sometimes left in a pan soaking in your sink). In the small intestine, this allows nutrients to be more readily absorbed. In particular, bile helps us absorb fatty acids and fat-soluble vitamins such as A, D, E, and K, as they cannot be absorbed without adequate bile. Without adequate bile, these essential nutrients can be lost and excreted with other wastes in the stool – leading to nutrient deficiencies. Issues with bile levels and/or function are one reason why nutrient depletions are so common in people with Hashimoto’s!
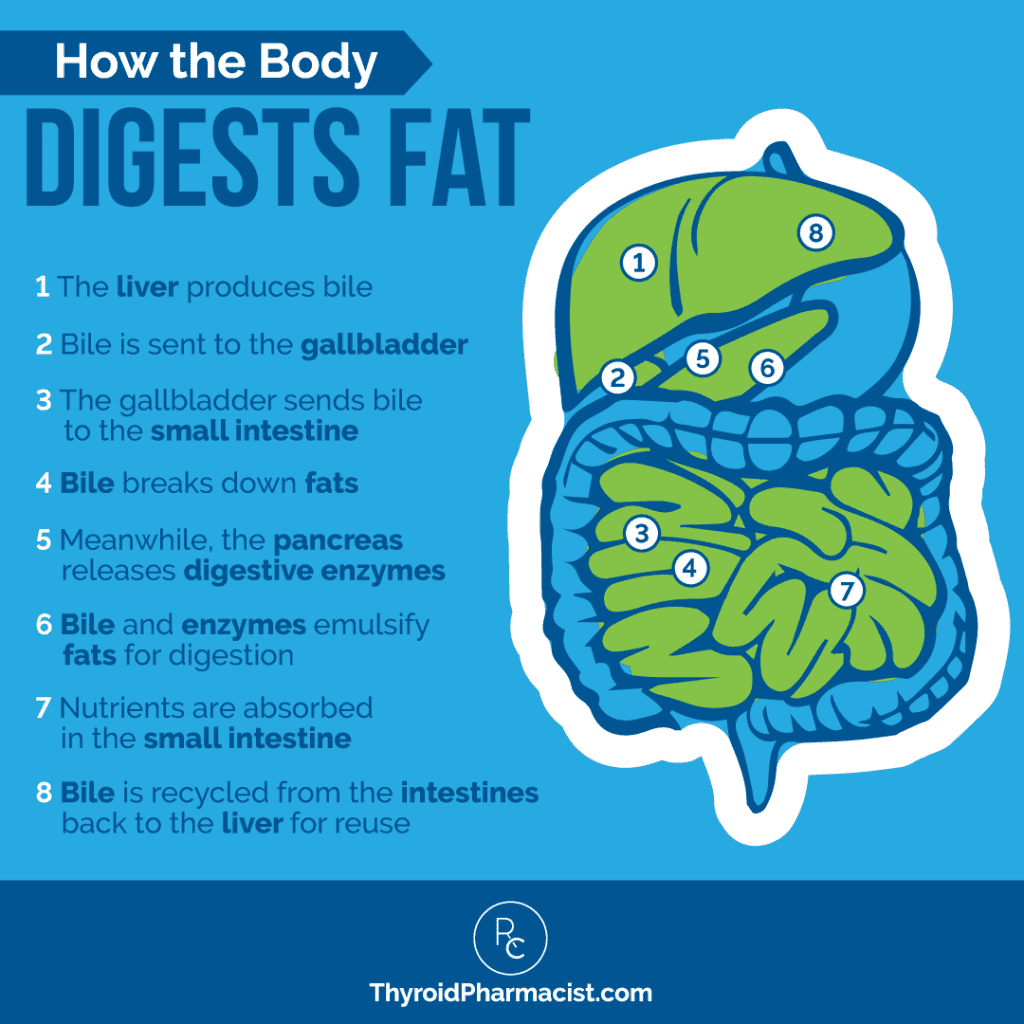
After working to break down fats in the small intestine, bile is then recycled from the intestines, back to the liver, for reuse. This offloads the workload of the liver by recycling about 95 percent of the body’s bile. This way, the liver doesn’t have to continually produce new bile.
If the gallbladder is dysfunctional, it is likely that the liver is also dysfunctional and producing unhealthy bile. The entire process – and your bile’s health – ultimately comes down to your liver’s health. This is why I focus on liver support as an initial step with any new client I work with!
You can see how bile’s role in breaking down fats, and emulsifying them, is vital to our ability to digest – and absorb key nutrients from – anything fatty. This includes healthy fats, too, like fish oil or avocados.
If you’ve had your gallbladder removed, or if your gallbladder is not functioning optimally, you are not going to have the concentration of bile that you need, nor will you get some of the additional benefits you would get from a healthy bile flow.
So What Are the Additional Benefits of Bile?
- Bile is thought to be antimicrobial, although the exact mechanism as to how it provides this benefit isn’t certain. It appears to stimulate the immune system in the intestines. In fact, it has been known to help prevent the bacterial overgrowth that is seen in small intestinal bacterial overgrowth (SIBO), a common root cause of Hashimoto’s. Thus, I always recommend testing for SIBO if you have issues with fat malabsorption.
- Bile is key to supporting the liver in excreting hormones and excess toxins, including cholesterol, the body’s waste products, environmental toxins, heavy metals, and other harmful substances. Since it helps remove excess estrogen, bile plays a key role in female sex hormone balance (and I’ll discuss this more in a minute).
- Bile may also have a role in blood sugar metabolism. Along with fat metabolism, bile may act as a signaling molecule relating to glucose (blood sugar) metabolism, and insulin levels have been correlated with bile cholesterol saturation. Thus, bile may play an important role in maintaining blood sugar balance. There have also been a lot of studies pointing to clear associations between insulin resistance and gallstones (solid particles that block the common bile duct and pancreatic duct, resulting in inflammation of the gallbladder), which can form as a result of bile issues. I found this particularly interesting, as blood sugar issues and type 2 diabetes often co-occur with Hashimoto’s, along with gallbladder issues!
The Link Between Fat Malabsorption, Gallstone Disease, and Hashimoto’s
People with Hashimoto’s and hypothyroidism often experience fat malabsorption issues and have an increased risk for gallbladder problems, as the thyroid can affect the composition of bile and its ability to flow.
The lack of thyroxine (free T4), as seen in hypothyroidism, decreases liver cholesterol metabolism. This results in changes to the bile composition itself, which then leads to what is called a state of bile cholesterol supersaturation. This thickens the bile and impairs it by slowing its rate of flow.
Decreased bile flow impacts an important process called peristalsis, the wave-like muscle contractions that push food and bile through the intestines. As peristalsis is reduced, many people experience constipation, with up to 15 percent of hypothyroid patients report having fewer than three bowel movements weekly.
As digestion slows down, there can also be increased bacterial growth, which can then result in diarrhea.
Furthermore, the change in bile composition and delayed flow can cause the liver’s cholesterol to crystallize, forming gallbladder stones, or gallstones.
The lack of thyroxine associated with hypothyroidism can also affect the sphincter of Oddi, which refers to layers of muscle that regulate the flow of bile into the small intestine/duodenum, which close between meals, preventing bile from continuing to flow into the small intestine when it isn’t needed. The sphincter may experience increased tension, which can prevent normal bile flow.
This has been thought to contribute to the formation of common bile duct stones, as well as gallstones/gallbladder stones.
Thus, it’s not surprising that there is an increased prevalence of hypothyroidism found in patients with common bile duct stones. In fact, patients with common bile duct stones and gallstones have, respectively, a seven-fold and three-fold increase in the frequency of hypothyroidism.
Experiments with hypothyroid rats have confirmed the thyroxine effect on bile composition, decreased bile flow, and relaxation of the sphincter of Oddi. Research in rats has also shown that the administration of thyroid hormone improves bile flow – suggesting that there is a strong correlation between developing gallbladder issues and hypothyroidism.
There are also indirect effects relating to bile production in those with thyroid disease.
Remember that when you have issues with bile production, you can have deficiencies in essential fat-soluble vitamins such as vitamins A, E, D, and K, as well as fatty acids. Vitamin D deficiency is commonly found in people with Hashimoto’s. Some 68 percent of my readers have reported having a diagnosed vitamin D deficiency. In fact, when I know someone has been supplementing with vitamin D, but still tests as deficient, I view that as an important clue that they may have fat malabsorption issues. The lack of key vitamins along with fatty acid deficiencies, can cause a whole host of additional symptoms and further impact thyroid hormone conversion (T4 to the active T3 hormone).
Furthermore, poor bile flow can lead to a recirculation of toxins such as heavy metals and excess hormones.
As you may know, nutrient depletions and impaired detoxification pathways are often the root causes of Hashimoto’s symptoms, so it’s important to address the gallbladder and bile issues that may be at the root of these issues.
Symptoms of Fat Malabsorption Issues and Gallbladder Problems
Since gallbladder and bile impairment can contribute to fat malabsorption issues and have been linked to hypothyroidism, it is no surprise that fat malabsorption issues are relatively common with Hashimoto’s. Unfortunately, they are often overlooked by practitioners or viewed as symptoms of other common conditions. Let’s review the common signs and symptoms of fat malabsorption and gallbladder issues:
- Digestive symptoms include greasy, smelly, floating, or light-colored stools; gas or belching after eating, diarrhea, stomach pain, gallbladder pain (located on the right side, under the ribs), gallstones, nausea, and weight loss. If you are not properly digesting and absorbing fats from food, you may start to experience low energy levels and increased cravings for carbs, since fats are an incredible slow-burning source of energy. People attempting a ketogenic (high-fat) diet may experience nausea or any of the above symptoms, and find that they are unable to comply with the high-fat dietary requirements.
- Non-digestive symptoms include dry hair, eczema, depression, dry/itchy/flaky skin or scalp, oily scalp, dandruff, and rashes. Hormonal imbalances (including estrogen dominance) and adrenal issues may also be seen.
- Symptoms related to vitamin and fatty acid deficiencies: As I already mentioned, if you’ve had fat malabsorption occurring for a while, you may start to develop symptoms of fatty acid deficiency, as well as depletions in the fat-soluble vitamins A, D, E, and K. Fatty acid deficiency symptoms may present as pain, inflammation, dry skin, oily hair, acne, or eczema. Deficiencies in the fat-soluble nutrients can lead to numerous additional symptoms, including vision problems, immune system imbalance, fragile bones, poor wound healing, easy bruising, bleeding gums, nosebleeds, dull hair, depression, skin disorders, eczema, dry and itchy/flaky skin or scalp, dandruff, oily scalp, rashes, and many other seemingly unrelated symptoms.
How to Diagnose Gallbladder Issues
There are a number of simple diagnostic tools that I use with clients. The first is just evaluating your symptoms. Your stools can tell you a lot, too! Greasy, smelly, floating, or light-colored stools can be a sign of bile issues.
I have found that many people with fat malabsorption issues also often experience low stomach acid (another common issue associated with Hashimoto’s), which makes it more difficult to digest proteins. The proteins that are often most difficult to digest are gluten, dairy, and soy.
Those who have symptoms of low stomach acid and see improvement after eliminating these proteins from their diet, may have a fat malabsorption issue.
Furthermore, if you have the MTHFR gene variation or difficulties with methylation, you may already have challenges with clearing toxins from your body, and may suffer from symptoms related to impaired methylation (like brain fog, anxiety, irritability, and chemical sensitivities).
An impaired ability to detoxify may also contribute to gallbladder issues.
Your practitioner can run some labs, such as liver function tests and/or a complete blood count (CBC) test, to check for gallbladder issues. Markers for impaired gallbladder functioning may include high bilirubin, AST, ALT, LDH, GGT, ALP, and 5’-nucleotidase. However, I find that oftentimes, gallbladder dysfunction can be missed.
As mentioned earlier, if a person has been supplementing with vitamin D but their labs still show a deficiency in it, I always suspect fat malabsorption, so testing one’s vitamin D levels can also help with diagnosis.
A low fecal elastase test result and/or high fecal fats/steatocrit, on functional-medicine stool tests such as the GI-MAP test, can also indicate fat malabsorption.
Since I originally published this article, I’ve learned that while a “low” result for fecal elastase is reported as being under 200 μg/g, an optimal level is above 500 μg/g, and people may be symptomatic, even with fecal elastase between 200-500 μg/g. Low fecal elastase can be an indication of exocrine pancreatic insufficiency, which can have more root causes, such as celiac disease, mold toxicity, SIBO, and many others.
I wrote a more in-depth article on pancreatic enzymes, as I’ve noticed some interesting patterns in people with Hashimoto’s with this particular issue.
If you are experiencing pain, or if your practitioner suspects gallbladder issues such as gallstones or common bile duct stones, they may use ultrasound testing or an abdominal X-ray to look for stones or other problems.
Other Risk Factors That May Point the Way to Gallstone Issues
If you are experiencing some of the above symptoms, there are other risk factors that may point to the presence of gallstones. Known risk factors for gallstone formation include:
- Obesity
- Genetic susceptibility (can dramatically increase risk, by nearly five times)
- High homocysteine levels
- Insulin resistance
- Metabolic syndrome (three or more symptoms of high blood pressure, high fasting glucose and/or insulin resistance, abdominal obesity, reduced HDL levels, and increased triglyceride levels)
- Advanced cirrhosis, chronic hepatitis C, or nonalcoholic fatty liver disease
Furthermore, female sex hormone (estrogen) changes can lead to gallbladder issues. This is the reason why women who have not yet reached menopause are three times more likely to be at risk of having gallstones.
Interestingly, oral contraceptive use and estrogen hormone replacement therapy have both been tied to changes in bile composition, specifically increases in cholesterol levels, which thickens the bile. This composition change is thought to contribute to the formation of gallstones. I’ve heard of increases in incidents of estrogen dominance seen after gallbladder removals, which would make sense given that the increased levels of estrogen would not be getting eliminated without sufficient amounts of bile.
Some women also experience cholestasis, a reduction in bile flow, in late pregnancy. This is thought to be related to changes in estrogen and progesterone hormone levels. There can be a reduction in both the normal flow of bile (along with greater cholesterol saturation), as well as in the body’s ability to clear out hormones. This sometimes results in reduced gallbladder function, as well as the formation of gallstones, although gallstones may clear during the postpartum period.
Conventional Treatments
Many people are not aware that they may have a fat malabsorption or gallbladder issue, as common symptoms may mirror other conditions. Gallstones themselves may often go completely undetected. It is estimated that about 15 percent of adults in the U.S. have gallstones, with only a very small percentage (1-3 percent) experiencing gallbladder-related symptoms.
It’s important, however, to be aware of severe gallbladder issues.
A gallbladder attack (acute cholecystitis), which happens when a gallstone passes into the small intestine or becomes stuck in a bile duct, can cause a good deal of continuous pain (in the upper right side of the abdomen) and is associated with nausea and vomiting, as well as fevers.
Infections may also occur. This blockage is often what inspires someone to contact their physician or visit the ER. Gallstone issues are a leading cause of hospital admissions related to gastrointestinal problems.
The conventional treatment for a gallbladder attack is often gallstone surgery.
In my opinion (and many medical professionals agree), you should not have your gallbladder removed unless the symptoms warrant it. True, a cholecystectomy (the complete removal of the gallbladder) can sometimes be unavoidable – especially if someone has been dealing with gallbladder disease for a lengthy time. However, unfortunately, the surgery is overused today, and is often called for even when a patient is experiencing only minimal – and correctable – symptoms. It is one of the most common elective abdominal surgeries performed in the U.S. today!
After this surgery, bile flows directly from the liver to the small intestine via the common bile duct, but it does not get stored and concentrated, so you can experience all of the symptoms we’ve already talked about. Having the bile flow directly into the small intestine may also affect the gut microbiome and gut function. Additionally, this surgery doesn’t necessarily stop the patient from producing another gallstone in the bile duct or liver!
If you are thinking of having gallbladder surgery (in a nonemergency situation), I highly recommend the book Save Your Gallbladder Naturally by Sandra Cabot, as well as consulting with a functional medicine practitioner, for guidance.
The Root Cause Approach to Supporting Liver, Gallbladder, and Fat Digestion
If you are experiencing symptoms associated with fat malabsorption, if you know you have a gallbladder condition such as gallstones, or if you are at an increased risk for gallbladder disease, my Root Cause Approach recommends several goals to focus on:
- Supporting your liver and gallbladder health overall
- Stimulating bile flow (quantity and motility) to support fat digestion
- Dissolving gallstones or common bile duct stones
- Supporting your body’s overall detoxification system
There are a number of supplements that I recommend, as well as supportive foods that you can incorporate into your diet, to help you reach these goals:
1. Rootcology’s Liver & Gallbladder Support can help support liver and gallbladder health, while also supporting fat digestion, in three different ways: it can support the liver’s ability to process fat, it can give us extra bile, and it can support a healthy bile flow (with ingredients such as dandelion, artichoke, and beets). I routinely recommend taking one capsule of this supplement with each meal, as a key component of my Liver Support Protocol!
This supplement also contains some key ingredients that help with gallbladder health:
- Taurine – This amino acid is a major constituent of bile. It protects the body from both toxicity and oxidative stress, and can naturally improve bile production. It has also been found to support thyroid function: research has shown taurine may help improve thyroid function in animals exposed to environmental toxins such as lead and insecticides.
- Milk Thistle – This plant contains silymarin, a compound that is considered to have hepatoprotectant effects (which means it protects liver health – hepato is greek for liver), in particular relating to toxins. Silymarin is also considered to have antioxidant effects and potential anti-inflammatory effects. Furthermore, it has been shown to improve pancreatic function after exposure to toxic agents. As a bonus, it has been found to support high blood sugar levels, which are commonly seen in those with Hashimoto’s.
- Ox Bile – Bile salts from oxen have been shown to increase bile flow and support fat digestibility in animal studies.
- L-Methionine – This amino acid helps detox heavy metals and prevents excess fat buildup in the liver.
- Inositol – In rat studies, this sugar has been shown to improve bile acid secretion as well as reduce oxidative stress. By the way, one form of inositol, myo-inositol, is known to have additional benefits in lowering TSH, as well as addressing blood sugar imbalances, OCD, and anxiety, in people.
Here is what Kristen H. had to say after trying Rootcology Liver and Gallbladder Support:
“I was suffering from on and off again gallbladder pain. Two doctors recommended having it removed. Then I developed abdominal pain right below my rib cage. I felt like I had a hardened organ (sounds weird, I know). The pain restricted my breathing severely. The doctors were stumped, and so was my chiropractor. After doing my own research, I discovered that it was likely my pancreas. Knowing I have a liver that struggles to detoxify itself, I had decided to finally start the Liver Protocol that Dr. Wentz mentions in her book. I had put it off for a while due to cost, but I’m glad I finally tried it! After two days of taking this supplement, my gallbladder and probable pancreas pain subsided. By day seven, my upper abdomen felt better than it had in years. Even though I’ve completed the protocol, I continue with the supplements and can really tell if I miss a dose. If you have similar issues, I can’t recommend trying this (and the Liver Protocol) enough. I’m so thankful to have been able to keep all my organs and not have to take prescription medications for my pain!”
Precautions
Liver & Gallbladder Support should not be used by those with Addison’s disease, a corn allergy, or a history of electrolyte imbalance. Do not use if you are allergic or sensitive to any of the ingredients in this supplement. Consult with a doctor before use if pregnant or breastfeeding.
Milk thistle has been known to cause gastrointestinal issues, itchiness, headaches, and can cause an allergic reaction in people who are allergic to other plants in the Asteraceae family, such as ragweed, daisies, marigolds, and chrysanthemums.
If you have diabetes, use milk thistle with caution, since the supplement might lower blood sugar. There is also concern that milk thistle might have estrogenic effects. If you have breast cancer, uterine cancer, ovarian cancer, endometriosis, or uterine fibroids, consider avoiding milk thistle.
Additionally, I don’t recommend taking this supplement if you currently take any of the following medications: antidiabetic drugs, Cytochrome P450 1A2, 2B6, 2C19, or 2D6 substrates, blood thinners such as warfarin, diclofenac, diuretics, dupilumab (Dupixent), glucuronidated drugs, HMG-CoA Reductase Inhibitors, immunosuppressants, lithium, monoamine oxidase inhibitors, monoclonal antibodies (MABs), morphine, niacin, p-glycoprotein substrates, quinolone antibiotics, raloxifene, retinoids — including acitretin (Soriatane), bexarotene (Targretin), etretinate (Tegison), isotretinoin (Accutane), tretinoin (Retin-A, Renova), and tazarotene (Avage) — steroid medications, sirolimus, and/or tamoxifen.
Furthermore, Liver & Gallbladder Support should not be taken by those using certain medications that have the potential to be toxic to the liver, including acetaminophen (Tylenol), amiodarone (Cordarone), carbamazepine (Tegretol), isoniazid (INH), methotrexate (Rheumatrex), methyldopa (Aldomet), or tetracycline-based antibiotics, including demeclocycline (Declomycin), minocycline (Minocin), and tetracycline.
Please note: Liver & Gallbladder Support uses non-GMO corn-derived ingredients and may contain a protein component that could cause an allergic response in those with corn allergies.
As always, please consult with your practitioner before starting any new supplement.
2. Remember that chronic fat malabsorption may result in a deficiency of essential fatty acids. If you have signs of fatty acid deficiency such as pain, inflammation, dry skin, oily hair, acne, or eczema, you may benefit from one to four grams of fish oil per day.
3. DaVinci Labs makes an A.D.K. combo that I recommend (note, it does contain the retinyl palmitate version of vitamin A, which can be controversial, though there is one study that showed this form can lower TSH in hypothyroid women), which may be helpful along with a soy-free vitamin E, for those with fat malabsorption.
4. Consider supporting any issues related to low stomach acid with betaine and pepsin, to help promote the proper digestion of proteins.
5. I’ve found supplementing with pancreatic enzymes to be very helpful in the breaking down and digesting of fats. This is because some people with fat malabsorption issues may also have exocrine pancreatic insufficiency, or a deficiency in pancreatic enzymes. This condition may result from chronic stress, mold toxicity, SIBO, alcohol use, H. pylori, low stomach acid, Giardia, celiac disease, or damaged microvilli in the gut.
In fact, about 50 percent of people who have tried pancreatic enzymes have reported seeing benefits after using pancreatic enzymes for a few weeks to a few months. In some cases, people may need to take pancreatic enzymes long-term and try other things to completely resolve their symptoms. Options for pancreatic enzymes include the prescription medication Creon, Rootcology Pancreatic Enzymes Plus, and Pure Encapsulations Pancreatic Enzyme Formula. I have written a deeper dive on pancreatic enzymes for more information.
The typical dosage is one or two capsules per meal. However, the dosage may need to be tailored to your individual needs, so I recommend consulting with your practitioner to find the right dosage for you.
6. Both magnesium citrate or magnesium glycinate can be helpful (note that magnesium citrate has a stool-softening effect, so the glycinate version may be a better option if you are experiencing diarrhea with the citrate version), as many people are deficient in magnesium, and it is an important nutrient required for the liver’s detoxification pathways. As an added bonus, magnesium also helps with sleep.
7. I recommend liver-supporting foods, including hot lemon water (my favorite morning drink), the Root Cause Green Smoothie, cruciferous veggies (note: some people may have a sulfur sensitivity and may be sensitive to crucifers), sprouts and seedlings, green juices and chlorophyll, fermented foods, turmeric, and berries. Cilantro is another great supportive food to help detox heavy metals.
Beets are also wonderful, as they are rich in betaine and folate, which help to break down homocysteine and can aid your body in eliminating toxins. (High levels of homocysteine are associated with health complications such as inflammation, heart disease, and pregnancy complications.) Beets are especially good for those with methylation issues as well.
8. Lastly, I recommend avoiding foods that may exacerbate gallbladder issues or contribute to the formation of gallstones. Gallstones have been associated with the Standard American Diet (S.A.D.), which is high in sugar and processed foods, and low in fiber. Research has shown that the intake of high energy simple sugars, and saturated fats, favor gallstone formation.
One study found that men who ate a diet high in polyunsaturated or monounsaturated fats (think olive and plant oils) were 18 percent less likely to develop gallstones than those on a diet consisting of the least of these types of fat (i.e. diets that were higher in saturated fat).
For this reason, I highly recommend increasing your intake of healthy fats and lowering your intake of sugar and carbs. Increasing your intake of fiber and ascorbic acid (a form of vitamin C) may also reduce your risk of developing gallstones.
In 1968, Dr. James Breneman described the ”gallbladder diet.” He believed that gallbladder attacks were the result of food sensitivities, and he recommended people use an elimination diet to identify their own triggers. In his research, he found that there were a handful of top food offenders, including eggs (the biggest offender), pork, onion, milk, poultry, coffee, oranges, nuts, corn, and tomatoes. He also found that about 20 percent of his study’s participants were sensitive to the prescription drugs they were using!
We know that food sensitivities can also be a trigger for Hashimoto’s. I always recommend people remove gluten and dairy as an initial step when evaluating any food sensitivities they might have. This is especially important, as gluten has been linked to an increased prevalence of gastric and gallbladder motility issues. Removing triggering food sensitivities can really make a difference in how you feel, and pretty quickly, too – so I recommend considering doing an elimination diet to identify your trigger foods! Also, please note, what I’ve learned about in my extensive research on food sensitivities is that we are often sensitive to the foods we eat most often… so use the “gallbladder diet” foods as a guide, but keep in mind that your personal food triggers may be different.
Tips for Those Without a Gallbladder
Along with the natural solutions discussed above, I’d also add a few recommendations specifically for those who no longer have a gallbladder:
- Supplement with ox bile. This can be found in combination products like Liver & Gallbladder Support or as a standalone supplement, like Ox Bile by Allergy Research Group. I recommend working with a practitioner to determine your ideal dose.
- Avoid trans fats and fried foods.
- Test for food sensitivities.
- Add fiber to your diet.
- Take vitamin C.
- Consider beetroot juice.
- Ensure you are getting adequate – and filtered – water (such as hot lemon water) to support a healthy detoxification system.
I’d also recommend people provide an extra dose of support for their liver by following the two-week Liver Support Protocol in my book, Hashimoto’s Protocol. In just two weeks, you will learn how to remove potentially triggering foods, add supportive foods, reduce your daily toxic exposure, and support your detoxification pathways.
Get Started Today
Remember, “You are what your body can digest, absorb and eliminate.” Optimal liver and gallbladder health is essential to all three of these important bodily functions. Remember too, how important bile is to your body’s ability to break down and gain the nutritional benefits of fats.
The good news? There is a lot you can do to ensure you are supporting these systems, as well as to address symptoms you may already be experiencing.
Eliminating food sensitivities is a great initial step, and if you are still experiencing fat malabsorption symptoms, consider some of my recommended digestive enzymes and supplements, like Rootcology Liver & Gallbladder Support, Ox Bile by Allergy Research Group, fish oil, Betaine with Pepsin, Pancreatic Enzymes Plus, and magnesium.
If you’re looking for tips and a handful of delicious recipes that are free of the most common foods that cause gallbladder issues, you may consider picking up a copy of my cookbook, Hashimoto’s Food Pharmacology: Nutrition Protocols and Healing Recipes to Take Charge of Your Thyroid Health. In it, you’ll find 125 recipes, tips on how to tailor your diet to your unique needs, and more!
I also encourage people to work with a functional medicine practitioner who can best identify your unique needs on your own healing journey. You can find my list of recommended practitioners here.
The important thing is to take action, even if it is just one simple change for today. You will find that you can have significant symptom improvements with even minor changes. And most importantly, you can feel much better.
I hope this helps you on your healing journey. I’m rooting for you!
P.S. Be sure to sign up for my weekly newsletter to get a free book chapter, recipes, my Thyroid Diet Quick Start Guide, notifications about upcoming events, and my latest research. For future updates, make sure to follow me on Facebook, TikTok, Pinterest, and Instagram!
References
- Hofmann AF, Eckmann L. How bile acids confer gut mucosal protection against bacteria. Proc Natl Acad Sci U S A. 2006;103(12):4333-4.
- Sieron D, Czerny B, Sieron-Stoltny K, et al. The effect of chronic estrogen application on bile and gallstone composition in women with cholelithiasis. Minerva Endocrinol. 2016 Mar;41(1):19-27. Epub 2014 Nov 21.
- Shaffer EA. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep. 2005. May;7(2):132-40.
- Wei J, Qiu DK, Ma X. Bile acids and insulin resistance: implications for treating nonalcoholic fatty liver disease. J Dig Dis. 2009 May;10(2):85-90.
- Chang Y, Sung E, Ryu S, Park YW, Jang YM, Park M. Insulin resistance is associated with gallstones even in non-obese, non-diabetic Korean men. J Korean Med Sci. 2008;23(4):644-50.
- Chang Y, Sung E, Ryu S, Park YW, Jang YM, Park M. Insulin resistance is associated with gallstones even in non-obese, non-diabetic Korean men. J Korean Med Sci. 2008;23(4):644-50.
- Laukkarinen J, Sand J, Nordback I. The Underlying Mechanisms: How Hypothyroidism Affects the Formation of Common Bile Duct Stones—A Review. HPB Surgery. 2012; 2012(102825).
- Laukkarinen J, Sand J, Saaristo R, et al. Is bile flow reduced in patients with hypothyroidism? Surgery. 2003. Mar;133(3):288-93.
- Daher R, Yazbeck T, Jaoude JB, Abboud B. Consequences of dysthyroidism on the digestive tract and viscera. World J Gastroenterol. 2009;15(23):2834-8.
- Goldin E, Wengrower D. Diarrhea in hypothyroidism: bacterial overgrowth as a
possible etiology. J Clin Gastroenterol. 1990 Feb;12(1):98-9. - Laukkarinen J, Sand S, Aittomäki S, et al. Mechanism of the prorelaxing effect of thyroxine on the sphincter of Oddi. Scandinavian Journal of Gastroenterology. 2002;37(6):667–673.
- Völzke H, Robinson DM, John U. Association between thyroid function and gallstone disease. World J Gastroenterol. 2005;11(35):5530-4.
- Laukkarinen J, Sand J, Nordback I. The Underlying Mechanisms: How Hypothyroidism Affects the Formation of Common Bile Duct Stones—A Review. HPB Surgery. 2012; 2012(102825).
- Inkinen J, Sand J, Nordback I. Association between common bile duct stones and treated hypothyroidism. Hepatogastroenterology. 2000;47:919–921.
- Daher R, Yazbeck T, Jaoude JB, Abboud B. Consequences of dysthyroidism on the digestive tract and viscera. World J Gastroenterol. 2009;15(23):2834-8.
- Andreini JP, Prigge WF, Ma C, Gebbard RL. Vesicles and mixed micelles in hypothyroid rat bile before and after thyroid hormone treatment: evidence for a vesicle transport system for biliary cholesterol secretion. J Lipid Res. 1994 Aug;35(8):1405-12.
- Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6(2):172-87.
- More Unsaturated Fats, Fewer Gallstones?. WebMD. https://www.webmd.com/digestive-disorders/news/20041004/more-unsaturated-fats-fewer-gallstones. Published October 4, 2004. Accessed February 27, 2019.
- Cuevas A, Miquel JF, Reyes MS, Zanlungo S, Nervi F. Diet as a risk factor for cholesterol gallstone disease. J Am Coll Nutr. 2004 Jun;23(3):187-96. Review.
- Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6(2):172-87.
- Massironi S, Branchi F, Fraquelli M, et al. Effects of a Gluten-Containing Meal on Gastric Emptying and Gallbladder Contraction. Nutrients. 2018 Jul 16;10(7).
- Di Stefano M, Carnevale Maffè G, Bergonzi M, Mengoli C, Formagnana P, DiSabatino A, Corazza GR. The effect of gluten on intestinal fermentation, gastric and gallbladder emptying in healthy volunteers. Dig Liver Dis. 2015. Sep;47(9):751-6.
- Shaheen NJ, Hansen RA, Morgan DR, et al. The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol. 2006;101:2128–2138.
- Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6(2):172-87.
- Konikoff FM, Paitan Y, Gabay G, Reshef L, Naftali T, Gophna U. Interactions between the intestinal microbiota and bile acids in gallstones patients. Environmental Microbiology Reports. 2015 Jul 6;7(6):874-880. https://doi.org/10.1111/1758-2229.12319
- Lamberts MP, Lugtenberg M, Rovers MM, et al. Persistent and de novo symptoms after cholecystectomy: a systematic review of cholecystectomy effectiveness. Surg Endosc. 2013 Mar;27(3):709-18.
- Murakami S, Fujita M, Nakamura M, Sakono M, Nishizono S, Sato M, Imaizumi K,Mori M, Fukuda N. Taurine ameliorates cholesterol metabolism by stimulating bile acid production in high-cholesterol-fed rats. Clin Exp Pharmacol Physiol. 2016 Mar;43(3):372-8.
- Akande MG, Shittu M, Uchendu C, Yaqub LS. Taurine ameliorated thyroid function in rats co-administered with chlorpyrifos and lead. Vet Res Commun. 2016 Dec;40(3-4):123-129. Epub 2016 Aug 25.
- Kawaguchi-Suzuki M, Frye RF, Zhu HJ, et al. The effects of milk thistle (Silybum marianum) on human cytochrome P450 activity. Drug Metab Dispos. 2014;42(10):1611-6.
- Karimi G, Vahabzadeh M, Lari P, Rashedinia M, Moshiri M. “Silymarin”, a promising pharmacological agent for treatment of diseases. Iran J Basic Med Sci. 2011;14(4):308-17.
- Kazazis CE, Evangelopoulos AA, Kollas A, et al. The therapeutic potential of milk thistle in diabetes. Rev Diabet Stud. 2014;11(2):167-74.
- Alzawqari M, Moghaddam HN, Kermanshahi H, et al. The effect of desiccated ox bile supplementation on performance, fat digestibility, gut morphology and blood chemistry of broiler chickens fed tallow diets. Journal of Applied Animal Research. 2011;39:2, 169-174.
- Methionine. National Center for Biotechnology Information. PubChem Compound Database; CID=6137. https://pubchem.ncbi.nlm.nih.gov/compound/Methionine. Accessed March 3, 2019.
- Methionine. WebMD. https://www.webmd.com/vitamins/ai/ingredientmono-42/methionine. Accessed March 3, 2019.
- Zhao SS, Li NR, Zhao WL, et al. D-chiro-inositol effectively attenuates cholestasis in bile duct ligated rats by improving bile acid secretion and attenuating oxidative stress. Acta Pharmacol Sin. 2018 Feb;39(2):213-221.
- del Pozo R, Muñoz M, Dumas A, et al. Effects of vitamin C administration on cholesterol gallstone formation]. Rev Med Chil. 2014 Jan;142(1):20-6.
- Krajka-Kuźniak V, Szaefer H, Ignatowicz E, et al. Beetroot juice protects against N-nitrosodiethylamine-induced liver injury in rats. Food Chem Toxicol. 2012 Jun;50(6):2027-33.
- Farhangi MA, Keshavarz SA, Eshraghian M, Ostadrahimi A, Saboor-Yaraghi AA. The effect of vitamin A supplementation on thyroid function in premenopausal women. J Am Coll Nutr. 2012;31(4):268‐274. doi:10.1080/07315724.2012.10720431.
- Milk Thistle. Mayo Clinic website. https://www.mayoclinic.org/drugs-supplements-milk-thistle/art-20362885. Published October 14, 2017. Accessed July 3, 2020.
- Food, Herbs & Supplements. Natural Medicines website. https://naturalmedicines.therapeuticresearch.com/. Accessed July 3, 2020.
Note: Originally published in April 2019, this article has been revised and updated for accuracy and thoroughness.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
On number 6 you note that magnesium plays an important part in digestion. I’m wondering why you don’t recommend magnesium malate ? It’s one I’ve been taking for some time. Is it related to a trigger food – such as gluten ? Just curious if I’m taking one that could be detrimental in some way. I’m also gluten intolerant.
Lastly, I have been search for a vitamin C that my body can handle – I seem to react it citrus based vitamin C – which makes me break out in cystic acne (never a good thing). Do you have another type of vitamin C that you would recommend ?
Thank you for your help,
A
Adreeza – thank you for reaching out. There are about 20 different types of magnesium and the Magnesium glycinate and Magnesium citrate are the ones that I’ve seen people have the most success with. I believe that most nutrients should come from the diet. This is why I always list food sources in the book and on the blog, for most of the nutrients, vitamins, minerals. and probiotics that are depleted in Hashimoto’s. However, some may require or prefer supplements. I recommend getting tested for deficiencies to determine your need for a supplement as instructed in the book and blog. I also don’t recommend starting multiple supplements all at once. I recommend starting one at a time and then adding another a week or so later once it has been confirmed that the first supplement is not causing any harm.
I do have a full supplements chapter in my books. Have you checked them out? Not everyone should be taking every supplement and any of these books will help uncover your root cause. This will help you figure out your supplementation. Here are the links:
Hashimoto’s Root Cause:
http://amzn.to/2DoeC80
Hashimoto’s Protocol:
http://amzn.to/2B5J1mq
NEW STUDIES ON MAGNESIUM AND THYROID HEALTH
https://thyroidpharmacist.com/articles/new-studies-on-magnesium-and-thyroid-health
Yes my gallbladder removal occurred November 2017. I need to change my whole diet and get educated on the root cause approach.
Louis – thank you for sharing! I hope you will keep me posted on your progress. <3
Your instruction about the pancreas and gallbladder seems to be what is causing a problem for me. Also I haven’t been able to drink milk since I can remember. I was very young. I have been constipated for weeks at a time even if I would drink a lot of water. I started changing my diet with coconut milk, oil, and now trying some cashew nut milk. I would like to know more of what to take for my digestive pain I have every night after a light meal. I am on 0.075 MG of Levothyroxine. I have other health problems which I don’t wish to discuss on this comment. I wish you could help me to get better. Thanks
Jeanne – thank you for reaching out. I am so sorry you are struggling with all of this! My heart goes out to you. <3 I always recommend starting with the diet. Are you gluten, dairy, corn and soy free? Are you eating a nutrient dense diet with fermented foods? Hashimoto’s is often a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better.
Hashimoto's is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission.
You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto's. Once you do, you will know what types of changes you need to implement to make yourself feel better.
If you need further support, please check out the list of lab tests inside the “Testing” chapter of my book, Hashimoto’s Root Cause. I also offer a 12-week program, Hashimoto's Self Management Program. Here are some resources I hope you find helpful as well.
BUILDING YOUR OWN HEALTH TIMELINE
https://thyroidpharmacist.com/sample-health-timeline/
Hashimoto’s Self-Management Program
https://thyroidpharmacist.com/enroll-in-hashimotos-self-management/
I can’t be sure if I have gallbladder or bile issues, although I have struggled with SIBO, Candida and possibly thyroid/hormone issues/hiatal hernia. I wonder about trying some of the things you mention. Would there be any harm in using this protocol?
Alison – thank you for reaching out. I am not able to advise on whether this protocol and supplements would be appropriate for you and your specific health needs without a comprehensive health assessment. It would not be legal or appropriate for me to give any type of medical advice here. If you have more specific questions on how and when to take particular supplements under normal circumstances, please do reach out to my team by email, at info@thyroidpharmacist.com and they will be more than happy to help ?
Thank you for this article Dr. Wentz. I had my gallbladder removed and have been struggling with all of the symptoms you mentioned. I also wondered if the problems originated in my liver instead of the gallbladder. I’m very careful about my diet but, recently I ate a fatty food, (busy day/bad choice) and a few days later, was hospitalized with possible pancreatitis or bile reflux/gastritis. Terrible pain and burning with Lipase levels over 6,000! Would I be a good candidate to try the Rootcology Liver & Gallbladder Support? I have also been diagnosed with Hashimoto’s and severe gluten intolerance. Thank you!
Kate – thank you for reaching out and sharing your journey. I am so sorry you experience this! <3 I am not able to advise on whether this supplement would be appropriate for you and your specific health needs without a comprehensive health assessment. I recommend that you discuss this with your personal doctor. If you have more specific questions on how and when to take this supplement under normal circumstances, please do reach out to my team by email, at info@thyroidpharmacist.com and they will be more than happy to help ?
Thank you for this amazing informative article! I had my gallbladder removed 10 years ago after having my first son, and even when they took it out they said it still looked healthy. As much as I can wish I knew all this prior, I’m so grateful to know it now! Thank you for taking the time to selflessly teach others how to better themselves. Super grateful!
Natalie – thank you so much for your support! I hope you keep me posted on your progress. <3
It was mentioned to eat cruciferous vegetables. With hypothyroidism an Hashimotos I thought cruciferous vegetables are not good for me…
David – thank you for reaching out. 🙂 There is a myth that foods known as goitrogens, such as cruciferous vegetables, are not good for those with Hashimoto’s. Iodine deficiency is not widespread in people with Hashimoto’s, and so eating cruciferous vegetables (unless you are sensitive to them) is perfectly healthy for people with Hashimoto’s and should not impact thyroid function. In the case that a person does have hypothyroidism due to iodine deficiency, he/she can still enjoy crucifers as long as they are cooked or fermented. Cooking/fermenting will break down the iodine blocking content. You can read more about the breakdown of the science behind the thyroid and goitrogens here: https://thyroidpharmacist.com/articles/what-are-goitrogens-and-do-they-matter-with-hashimotos/
I have cried for the needless suffering my daughter has endured as I have come to read more of Izabella’s books and online comments and learn about the causes of her ongoing problems. My daughter, now 40, has suffered since the age of 12 with a variety of symptoms that have severely impacted her life. We have sought medical help, resulting in a range of diagnoses, none of which have been helpful. She has had her gallbladder removed, had problems conceiving and now has a non-verbal, autistic child. So much suffering could have been avoided had we known Izabella’s information 30 years ago. It breaks my heart that all of this suffering was avoidable.
Steph – thank you so much for reaching out and sharing your daughters journey. I am so sorry she has struggled so long. My heart goes out to her! <3 Hashimoto’s is often a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better. Hashimoto's is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission. You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto's. Once you do, you will know what types of changes you need to implement to make yourself feel better.
If you need further support, please check out the list of lab tests inside the “Testing” chapter of my book, Hashimoto’s Root Cause. I also offer a 12-week program, Hashimoto's Self Management Program. Here are some resources I hope you find helpful as well.
BUILDING YOUR OWN HEALTH TIMELINE
https://thyroidpharmacist.com/sample-health-timeline/
Hashimoto’s Self-Management Program
https://thyroidpharmacist.com/enroll-in-hashimotos-self-management/
Hi Dr. Wentz,
I hope this message finds you well. I am concerned about the extremely high level of saturated fat in coconut milk. Will consuming it every day in the smoothies you recommend hurt my heart over time?
Thank you.
~M.S.
M.S. – thank you for reaching out! If you are concerned about the amount of fat in the smoothie feel free to find an alternative that works best for you. or use filtered water. I do offer other delicious smoothie recipes in my new cook book Hashimoto’s Food Pharmacology. Here is a link if you would like to check it out:
Hashimoto’s Food Pharmacology
https://www.amazon.com/Hashimotos-Food-Pharmacology-Nutrition-Protocols/dp/0062571591?tag=thyroipharma-20
I have high bilirubin due to a hereditary condition called Gilberts disease. I do not know if this has caused any problems. I also have issues with fat malabsorption according to a stool test. How are these things related?
Darci – thank you for reaching out and sharing. <3 I don’t currently have information to share on whether there is a connection between these but, I will add it to my list of possible future articles to research.
Very informative article! I have been suffering for a long time (much of that time undiagnosed). I have seen countless drs, naturopaths, nutritionists, specialists, etc, to no avail. I had my first gallbladder attack after I had my second child at the time went to the ER had elevated liver enzymes and gallstones. They said it was up to me to remove or not so I went home determined to heal it. I already didn’t eat dairy or gluten and most grains for quite some time. I have tried so many things that I’m just completely overwhelmed and exhausted by it that I’m thinking of removing my gallbladder but the thing that stops me is knowing it is still not addressing the root problem and most likely will exacerbate the conditions. I take Super enzymes with Pepsin, HCL and Ox bile 3 times a day with meals, I get magnesium and vitamin d3 and have tried C and B complexes (I frequently dip in iron). Initially I tried low fat to calm my gb down even though I know it’s not best and then slowly transformed to keto and was able to do that for 2 weeks successfully but at the end had painful gb attacks again. I’ve tried moderate fat, I’m always low carb. Most recently I tried the carnivore diet after coming across Mikhaila Petersons success at reversing her own autoimmune diseases but my body will NOT let me fast (I have Hashimotos and assume this could be why?) I get so weak exhausted and anxious I cant even take care of myself let alone my 2 kids. My gallbladder requires me to eat less, while my hashimotos demands I eat more frequently. I just feel at a total loss and am meeting with a surgeon next week re gb surgery and I’ve been working tirelessly to heal myself and reverse this. I dont do well on veggies as they bloat me..also looked into low oxalate (Sally K Norton). I previously read the book you suggested by Calbot and it was no help to me. I also followed the Andrea’s Moritz protocol for flushing out stones I did 3 flushes and never felt better after any. Please help me I’m desperate.
LV – thank you so much for reaching out and sharing your journey. I am so sorry to hear you are struggling with gallbladder issues. My heart goes out you. <3 I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It's a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
I’ve had hypothyroidism & high cholesterol for about 5 years and I had my gallbladder removed a month ago. Reading your article made me wish I’d done more to repair it before removal as I’m still having symptoms & even with my usual healthy diet, I’ve gained almost 5kg in a month. I have mild reactions to dairy & gluten so I’ve decided I will eliminate these from my diet. What would you suggest I take supplement wise to improve my gut health & help my body now it doesn’t have a gallbladder? Any advice I kindly appreciate!
Paige – thank you for reaching out and sharing your journey. <3 I believe that most nutrients should come from the diet. This is why I always list food sources in the book and on the blog, for most of the nutrients, vitamins, minerals. and probiotics that are depleted in Hashimoto’s. However, some may require or prefer supplements. I recommend getting tested for deficiencies to determine your need for a supplement as instructed in the book and blog. I also don’t recommend starting multiple supplements all at once. I recommend starting one at a time and then adding another a week or so later once it has been confirmed that the first supplement is not causing any harm. I do have a full supplements chapter in my books. Have you checked them out? Not everyone should be taking every supplement and any of these books will help uncover your root cause. This will help you figure out your supplementation. Here are the links
Hashimoto’s Root Cause:
http://amzn.to/2DoeC80
Hashimoto’s Protocol:
http://amzn.to/2B5J1mq
Hashimoto’s Food Pharmacology (this is my latest book):
https://www.amazon.com/Hashimotos-Food-Pharmacology-Nutrition-Protocols/dp/0062571591?tag=thyroipharma-20
I am living without my gall bladder. Since 1976. I keep wanting to learn as much as I can. I would like a print copy of this article. I don’t know Know how to do that from this Facebook post. Usually can find my way to safari. Having trouble.
Maureen – thank you for reaching out. <3 If you scroll to the bottom of the article, you should see a little printer icon so that you can print the article you could also email it to yourself and print from there if you are having trouble finding the print option. If you continue to have trouble please reach out to my team at info@thyroidpharmacist.com and they will be happy to help you.
Which is the dosage for inositol and taurine ?
Iulia – thank you for reaching out. For questoins about the supplements please email my team at info@rootcology.com and they will be happy to help. <3
Hi Dr. Wentz. What is gallbladder sludge and is there anything that can be done about it, besides removal?
Thank you.
Marie – thank you for reaching out. <3 If you are experiencing symptoms associated with fat malabsorption, if you know you have a gallbladder condition such as gallstones, gallbladder sludge or if you are at an increased risk for gallbladder disease, my Root Cause Approach may be helpful. Please check out the article above for my recommendations.
I have had my gallbladder removed AND have had gastric bypass. I’ve gained my weight back. Having the bypass has bypassed part of my intestines to help my body NOT to absorb so much fat. I’m sure that I have Hashimoto’s as well. I’m not entirely sure what to do related to getting things back on track and what I should be doing diet wise. Any guidance in this unusual situation is greatly appreciated.
Lisa – thank you so much for sharing. I’m so sorry you are struggling. <3 I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It's a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
Hello Dr Wentz.
I have Hashimoto’s Disease and have developed a number of other issues over the last 30 odd years including gastrointestinal problems (reflux, colitis and unexplained upper right quadrant abdominal pain).
As I am a vegetarian, I am not able to ingest the Rootcology Liver and Gallbladder Support due to the ox bile.
Is there a vegetarian option available?
Leanne – thank you for reaching out and sharing. ❤️ Intestinal permeability (aka leaky gut) is present in every case of autoimmunity and often precedes the development of Hashimoto’s. Symptoms of leaky gut may include bloating, diarrhea, constipation, stomach aches, acid reflux and irritable bowel syndrome. According to the Institute of Functional Medicine, many people develop IBS 5-10 years before an autoimmune diagnosis. I was one of them and didn’t take my gut health as seriously as I should have. Gut problems are often caused by infections like H. pylori, parasites like Blasto, SIBO, an imbalance of bacteria, and enzyme deficiencies or food sensitivities (especially to gluten, dairy, and/or soy). Even stress can be a factor in gut permeability. When it comes to the Rootcology Liver and Gallbladder support, I do not have a vegetarian recommendatin. You may want to discuss this with your practitioner who is familiar with your health history. Here is an article I hope you find helpful.
6 DIFFERENT ROOT CAUSES
https://thyroidpharmacist.com/articles/6-different-hashimotos-root-causes/
Hi Dr Wentz
I have been dealing with gallbladder issues for the past year. No gallstones from ultra sound, h.Pylori negative, non Hashi’s hypothyroid – . HiDA scan showed a 0% ejection fraction. I have been trying various dietary changes, low fat, gluten free, supplements, enzymes, accupuncture etc. A lot of what you have discussed above. I’m at the end of my rope with the pain/discomfort, nasuea and fatigue. Have you ever seen someone recover from a 0% ejection fraction rate?
Tracey – thank you for sharing your journey. ❤️ I’m so sorry you are struggling with all of this. Gut healing is a journey; you may need various interventions like removing reactive foods and infections, taking enzymes and probiotics, and balancing nutrients. Remember, be kind to yourself and learn to listen to your body so that you can support and feed it properly! I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
IMPORTANCE OF GUT HEALTH
https://thyroidpharmacist.com/articles/importance-gut-health/
Hello, how do you dissolve gallstones?
Will your Liver and Gallbladder support still help if you do not have a gallbladder?
Leah – thank you so much for following! Yes, Liver & Gallbladder Support can be taken by those without a gallbladder! ❤️
After having my gall bladder removed 20 years ago, and suffering subsequent chronic diarrhea for the last 20 years….I was finally diagnosed with Bile Acid diarrhea. I didn’t see this mentioned in your article as something to look out for. A 6 month course of a bile acid sequestrant has completely resolved my issue. I wish more doctors knew to look out for this in their patients after gall bladder removal.
Sarah – thank you so much for sharing this with me! ❤️ This is something I am adding to my list to research further! Thank you!
I have the same exact problem! I’m curious as to what Dr. Wentz can find out about this.
I’m wondering why you don’t mention TUDCA with zinc and selenium? I’ve tried all the things you’ve listed, for months, but no success. My symptoms got worse. I’ve been on TUDCA 3 weeks and my hair loss stopped, bowels moving better, sleep amazingly, skin less dry. Looking forward to what the next few months holds for this very well documented supplement. The Chinese have used TUDCA for liver so long they even have bear farms (not humane practices though), for the prized substance.
Ann – thank you for reaching out. I’m so glad to hear you have found TUDCA to be helpful! TUDCA, a specific form of bile acids (derived from taurine), to target oxalates. Here is an article that you might find interesting:
https://thyroidpharmacist.com/articles/oxalates-affect-thyroid-health/
What about those with a higher than normal ejection fraction rate? How would one support an overactive gallbladder? I’m asking because the foods that are “good” for gallbladder are my major sensitivities, spinach, brussels, banana and ect. All give me gallbladder pain when I eat them. And yes I am aware that those are high histamine foods.
Thank you for your answer!
Jessica – I’m so sorry you are struggling with this. Gut healing is a journey; you may need various interventions like removing reactive foods and infections (such as an elimination diet), taking enzymes and probiotics, and balancing nutrients. Listen to your body so that you can support and feed it properly. I also highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources I hope you find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
IMPORTANCE OF GUT HEALTH
https://thyroidpharmacist.com/articles/importance-gut-health/
You mentioned avoiding milk thistle if one has uterine fibroids. Is there a gallbladder and liver support formula that is safe for those individuals to use?
Shelly, thank you for following. I don’t currently have an option that excludes milk thistle to recommend.
Thank you for sharing all you knowledge and research. I need your books. Feels overwhelming but as I get older I know I need to make healthy changes. I had my gallbladder removed and recently my pancreas 😏. I’ve been on a journey with my gut health.
Erica – My pleasure. Here are some links to my books so you can check them out.
Hashimoto’s Root Cause
https://amzn.to/2XXCqcQ
Hashimoto’s Protocol
https://amzn.to/3cJ89T4
Hashimoto’s Food Pharmacology
https://amzn.to/2x6GRXW
Adrenal Transformation Protocol
https://amzn.to/3VawIAc
What is first from your experience ? Hypothyroid or gallbladder problems? Thank you.
Jirina, From my experience, hypothyroidism often precedes gallbladder issues, particularly in individuals with Hashimoto’s. Low thyroid function can slow down metabolism, including the digestion and flow of bile, which can contribute to gallbladder dysfunction over time. However, it’s important to remember that each individual is different, and both conditions can influence each other. Working with a healthcare provider to address both thyroid health and gallbladder function is key to restoring overall wellness.