We know that Hashimoto’s and other autoimmune conditions develop due to three things.
Genetic predisposition is one of those. The other two, intestinal permeability and autoimmune triggers, must also be present, and they are – thankfully – things we can actually address and improve upon through lifestyle interventions.
What’s common in Hashimoto’s and other autoimmune diseases is that triggers contribute to your body developing something called “a lack of self-tolerance.” This is when the body is no longer able to recognize its own tissue as part of itself, but instead starts viewing its tissue as a foreign invader. It is no longer “tolerant” of itself, and this is what leads to an autoimmune condition. How does this happen?
What happens can be described as a case of mistaken identity. First, some microbial triggers or bacterial cells from an infection actually do trigger the body’s immune system to attack the invading cells. But due to something called molecular mimicry, the body may then target other cells that resemble these invaders. This can result in the immune system attacking its own body.
Triggers can be food sensitivities, nutrient depletions, toxin exposures, chronic infections, a poor stress response, and a number of other things. Some triggers can actually also lead to intestinal permeability (leaky gut) issues as well, such as with what happens with gluten sensitivity.
In most cases of Hashimoto’s, this lack of self-tolerance starts to occur before thyroid function is affected- often before symptoms even occur.
When the body begins this breakdown of its immune tolerance, we’re initially going to see the presence of elevated thyroid antibodies.
We can test for thyroid antibodies, and when we identify their presence, we can put corrective actions in place, so thyroid disease doesn’t manifest or progress.
But My Doctor Said My TSH Level is Normal!
“My doctor said my TSH level is normal, so why should I worry about testing for thyroid antibodies?”
I can’t tell you how many times I hear this in my clinical practice and from readers. And I thought this myself many years ago. I spent almost a decade undiagnosed because I only had my TSH tested, and my thyroid diagnosis was completely missed. I had been told that my thyroid was normal even though my TSH was 4.5 μIU/mL. That left me struggling with progressively worse symptoms for almost ten years; symptoms like chronic fatigue, anxiety, depression, hair loss and many others.
By the time I was finally tested for TPO antibodies, they were in the 2000 IU/mL range. (To put that in perspective, the optimal range is less than 2 IU/mL) Plus, I had developed new onset panic attacks and was basically crippled by my poor health.
This is why I’m so passionate about advocating for you to get the proper tests and for you to understand your tests. Had I known then what was happening in my body, I could have taken on the lifestyle modifications and treatment steps necessary to not only alleviate my progressing symptoms but also prevent further damage to my thyroid.
Thyroid antibodies are going to be the first indication of a thyroid problem in many cases. They can be elevated for 5, 10, sometimes even 15 years before a change in TSH is even detected! Keep in mind that the presence of thyroid antibodies means that there is an active destruction going on against your thyroid.
Elevated thyroid antibodies, even in the presence of a “normal TSH”, means that it’s only a matter of time before your thyroid becomes destroyed to the point it can no longer produce sufficient amount of hormones.
For you to better understand how thyroid antibodies can be an early warning system before you start seeing thyroid symptoms, let’s talk first about the 5 stages that occur in Hashimoto’s as the disease progresses.
You’ll quickly see the importance of identifying the presence of thyroid antibodies.
Thyroid Antibodies – An “Early Warning” for Hashimoto’s
In Hashimoto’s, we know there are 5 stages relating to the initial development and also worsening of the disease. A quick review of these stages is helpful in understanding the importance of knowing your thyroid lab results.
It also really demonstrates the importance of specifically knowing your results relating to the presence of elevated thyroid antibodies.
Stage 1: The Genetic Predisposition
The first stage is when the person does not have any manifestations of Hashimoto’s. So, they are going to have a normal TSH and will have normal thyroid function. They will not have any elevated thyroid antibodies. If you were to biopsy their thyroid gland, it would be perfectly normal. They just have the genes at this point. Again, there are 3 requirements for the disease to progress: genetics, intestinal permeability, and one or more triggers.
Stage 2: The Breakdown of the Immune Tolerance (This is the early warning for Hashimoto’s!)
In the second stage, you start seeing the breakdown of the thyroid’s immune tolerance, and the person will start to have a white blood cell infiltration into the thyroid gland. Some of these immune cells are going to start grouping there. This is when we will also start seeing elevated thyroid antibodies. This stage can go on for many years – a decade or more – before a person moves on to stage 3 or 4, when we start to actually see symptoms and changes in thyroid function.
Stage 3: Subclinical Hypothyroidism Occurs
Stage 3 is when subclinical hypothyroidism occurs, and in this stage, people are going to have an elevated TSH in addition to having thyroid antibodies. They will also have immune cell infiltration into the thyroid gland, although their T3 and T4 levels are still going to be normal. Many people will have some symptoms of hypothyroidism or autoimmune symptoms at this stage.
Stage 4: Overt Hypothyroidism Occurs
Stage 4 is where we will start seeing overt hypothyroidism. There has likely been a lot of damage that has now occurred to the thyroid gland. The thyroid will no longer be able to compensate nor keep the thyroid hormone levels normal, and we will start seeing a change in T3 and T4 levels.
Stage 5: Hashimoto’s Progresses, and There is a Progression to Other Immune Disorders
In stage 5, as Hashimoto’s progresses, we unfortunately have a progression to other immune disorders as well. At this time, a person may get diagnosed with Rheumatoid Arthritis, Lupus or any of the other types of autoimmune conditions.
So as you look at the progression of disease, note that our earliest “warning” about Hashimoto’s, and our best opportunity for early intervention, is during Stage 2 when we initially find evidence of thyroid antibodies.
The Importance of Thyroid Antibodies Even in the Absence of Hypothyroidism
Thyroid antibodies have been connected to many symptoms even in the absence of hypothyroidism. When people are in stage 2 and they have thyroid antibodies, they may start to exhibit a whole bunch of different non-specific symptoms like fatigue, anxiety, stress, miscarriages, weight gain, and just feeling unwell.
Without verifying the presence of thyroid antibodies, these types of symptoms may not be associated with developing thyroid disease, and they may end up being misdiagnosed as other things such as anxiety, fatigue (perhaps even laziness!), depression, menopause, or even hypochondria. I have personally seen a number of clients who were diagnosed with depression and even bipolar disease as a result of being in stage 2 and already having elevated thyroid antibodies for years.
Remember, if these antibodies go unchecked, we are going to potentially start seeing a progression into stage 3, where we see subclinical hypothyroidism, stage 4 where we start seeing changes in TSH, and stage 5 which may include the progression of other autoimmune conditions.
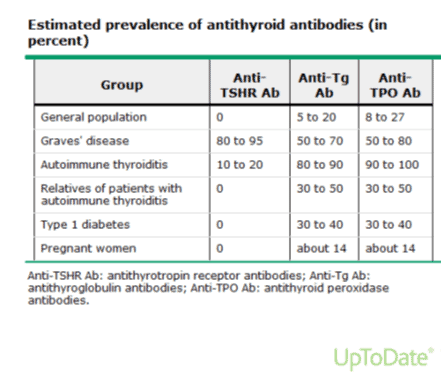
Note that a small number of antibodies may be present in normal individuals (the “general population”, as noted in my chart below) without thyroid disease. According to UpToDate, roughly 5-27 percent of the general population will test for extremely low levels of antibodies (“normal” is generally considered to be less than 35 IU/mL, although you’ll see that my view of an optimal range is much less). But, when you find elevated thyroid antibodies outside of this range, that is an indicator that the immune system is targeting the thyroid gland for destruction. (Please note that the UpToDate chart, shown below, shows the prevalence of thyroid antibodies as in 5-27 percent of the general population, but other studies have reported the prevalence of thyroid antibodies to be as high as 38 percent in some populations.)
Why Aren’t Thyroid Antibodies the Initial Screening Test Used for Thyroid Disease?
You might wonder why TSH is still the standard screening test for thyroid disease given that thyroid antibodies can be elevated for decades before any change in TSH may even be seen.
That’s a good observation and an even better question. Unfortunately, many traditional doctors ONLY test for antibodies after they see an elevation in TSH. It’s backwards from what it needs to be. That is why you need to be your own advocate and insist on thyroid antibodies testing. You can discuss this testing with your physician or you can also self-test, as the tests are not overly expensive. I’ll talk more about that below.
At some point, the medical community will pick up on the importance of antibodies as an early warning for Hashimoto’s. I also believe labs will start to incorporate newer findings. For example, the reference range for TSH itself has already been redefined by the American College of Clinical Endocrinologists. The reference range was lowered (from 0.2-8.0 μIU/mL to 0.3-3.0 μIU/mL), but most labs you get still use the old higher ranges as “normal”. That will hopefully change in the future.
On top of the reference ranges changing, we also know that a person with Hashimoto’s may fluctuate between high and low TSH readings. Reference ranges are also only average values, so even if your TSH reads as “normal”, you may not be. Remember, I was told my thyroid was normal when my TSH was 5.5 μIU/mL, and I was sleeping for 12 hours each night! TSH is not the screening tool we should be solely using.
TSH screening catches the later stages of Hashimoto’s. What we need to do is start testing for thyroid antibodies earlier.
What are the Thyroid Antibodies That Need to be Tested?
There are three main types of antibodies in Hashimoto’s that are potentially going to be present. Two of them are created by the immune system to target the thyroid gland as if it were a foreign invader like a pathogen, and those are Thyroid Peroxidase (TPO) and Thyroglobulin (TG) antibodies.
80-90 percent of people with Hashimoto’s will have either TPO or TG antibodies, or both. The more elevated the thyroid antibodies are, the greater the likelihood of developing overt hypothyroidism as well as possibly additional autoimmune conditions.
Where do these antibodies come from? The current scientific thinking is that activated B-cells in the thyroid gland and lymph nodes secrete these antibodies, and that they react solely as markers but don’t necessary attack the thyroid gland themselves. They likely activate T-cells, which then do the actual damage on the thyroid gland.
The third type of thyroid antibodies is TSH-Receptor (TSH-R) antibodies, including thyroid-stimulating immunoglobulin (TSI). This particular marker is elevated in more than 90 percent of people with Graves’ disease. TSH-R antibodies are also more common in people who have thyroid cancer.
Another TSH-R antibody is known as TSH-binding inhibiting immunoglobulin (TBII). This is elevated in >50 percent of people with Graves’ disease.
What if You Don’t Test Positive for Thyroid Antibodies, Can You Still Have Hashimoto’s?
Current medical reports state that 80-90 percent of people with Hashimoto’s will have TPO antibodies. That said, researchers at the University of Wisconsin’s Thyroid Multidisciplinary Clinic found that only half of the patients who tested positive for Hashimoto’s through cytology (when thyroid cells are withdrawn by a thin needle and then evaluated under a microscope) had TPO antibodies. This means that a person can have Hashimoto’s even if their thyroid antibody test is negative. This variant of Hashimoto’s is known as serum negative Hashimoto’s and is a less aggressive form of Hashimoto’s, so it will be slower developing.
Additionally, researchers have identified that the body may produce other thyroid antibodies, that are not yet available outside of research labs, but may also play a role in thyroid disease, including Sodium-iodine symporter (NISAb) and Pendrin (PenAb). The clinical relevance of these antibodies is not yet understood, but as with all emerging research, we just want to be aware of it. NISAb is found in 17 percent of people with Hashimoto’s and Pendrin is found in 11 percent.
I’ve included a chart from UpToDate that shows the estimated prevalence of these three antithyroid antibodies in various populations. Again, keep in mind that the more elevated these antibodies are, the more likely you are to progress to the stage that involves the destruction of your thyroid.
Image via UpToDate
Where to Get Tested and Optimal Ranges
Thyroid antibodies are tested through a simple blood test. If your physician is not receptive to testing your antibodies, you have the option of ordering your lab tests through Ulta Lab Tests. They offer self-order options with discounted panels that I set up with them, which can be ordered anywhere in the US. You will receive a lab order that can be taken to your local lab, and the results will be sent to you electronically.
In many cases, you can self-order the labs and then send the receipts for reimbursement to your insurance. (Please check with your insurance to ensure that they will accept this as well as to understand the required submission procedures).
The three tests can be found here:
Alternatively, you can opt for a full thyroid panel which includes tests for TSH, free T3, free T4, and two of the thyroid antibodies (TPO and TG).
For additional information on the full thyroid panel, you can also review this article.
I often get messages from readers asking me to comment on their personal thyroid labs. Unfortunately, I can’t provide medical advice through the internet without doing a personalized comprehensive case review. (This is for my readers’ own safety as well as complying with professional liability laws.) However, I created some lab interpretation information for them that I will share with you below.
If your doctor is ordering these labs for you, be sure to request a copy for yourself to ensure that they are interpreted correctly. Also, note that this information is based on optimal functional medicine ranges and my clinical experience, and may not be recognized by doctors who are not familiar with functional medicine.
Thyroid Panel Reference and Optimal Ranges
When I look at my clients’ labs, I focus on optimal reference ranges. Here’s a handy reference chart I use from the Institute of Functional Medicine.
Test Name | Standard Reference Range | Optimal Reference Range |
| TSH | 0.4-5.5 μIU/mL | 0.5-2 μIU/mL, 0.5-2.5 μIU/mL in elderly |
| Free T4 | 9-23 pmol/L | 15-23 pmol/L |
| Free T3 | 3-7 pmol/L | 5-7 pmol/L |
| Reverse T3 | 11-21 ng/dl | 11-18 ng/dl |
| TPO Antibodies | <35 IU/mL | <2 IU/mL |
| TG Antibodies | <35 IU/mL | <2 IU/mL |
You can see here that the normal reference range for TPO and TG antibodies is <35 IU/mL. According to conventional standards, this means that a person is not going to test for Hashimoto’s within this range. The optimal functional medicine range is less. We look for TPO and TG antibodies of <2 IU/mL.
Do Antibody Numbers Matter?
Some clinicians will say that once you have thyroid antibodies, you will always have thyroid antibodies, so the actual number doesn’t matter, as the antibodies can randomly fluctuate. I respectfully disagree. Antibodies fluctuate in response to triggers (some as common as stress), and in my exhaustive experience, they can be an incredibly helpful marker for tracking disease progression. That said, they should not be the only marker. We also want to look at your overall health… and the big picture… are you feeling better or worse?
What Number is Considered Remission?
Remission to me is a journey, not necessarily a destination. While researchers have labeled thyroid antibodies under 100 IU/mL as “remission status”, and thyroid antibodies above 500 IU/mL as “aggressive”, I would again caution to look at the big picture.
Remission is not the same as a cure, rather, remission is a respite from the disease, a reduction in the expression of the condition as well as a reduction in symptoms.
The definition for remission will thus vary with each person. Where were you when you got started on your journey?
If you started with thyroid antibodies in the 5000 IU/ml range and 10+ symptoms, improving your health to a point where your antibodies are 1000 IU/ml, and you only have 5 symptoms, may be your remission.
If, however, you started with antibodies in the 200 IU/ml range, and only had 3 symptoms to begin with, thyroid antibodies of 1000 IU/ml and 5 symptoms may be an exacerbation or worsening of the condition for you.
Thus, the goal of remission is for you to work on improving your health, and every small change that I recommend will hopefully result in an improvement for you. And yes, in some cases, a complete remission is possible, where you no longer test positive for any thyroid antibodies, don’t have a single symptom, and there is no evidence of damage to your thyroid gland.
How Often Should You Test Your Thyroid Antibodies?
I often hear from readers who say that their doctors refuse to retest their thyroid antibodies, stating that once a person is thyroid antibody positive, they will always be positive, so retesting the antibodies is useless. I disagree. Tracking your thyroid antibodies can give you an idea of how aggressive the attack is on your thyroid gland. While other lab markers and symptoms should be considered, generally, a lower thyroid antibody number indicates that your condition is improving, while a higher antibody number may indicate that you are having a flare-up or that your condition is worsening.
Tracking antibodies can give you an idea of whether the interventions you’re utilizing are working, i.e. is your change in diet leading to an improvement in your condition?
When implementing active interventions, you can check antibody levels every 1-3 months to see a trend; however, it will take anywhere from 3 months to 2 years to see the full impact of an intervention.
THEA Score: Assessing Your Risk for Hypothyroidism
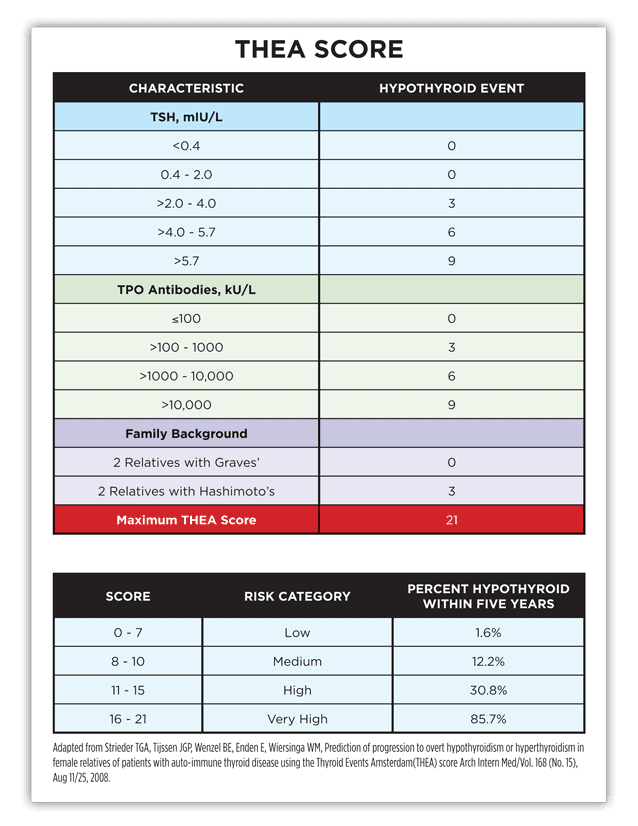
Once you have your lab results in hand, there is a great tool that your clinician can use to help determine the aggressiveness of your condition. The Thyroid Event Amsterdam (THEA) Score is a score that can help assess your risk of progression into hypothyroidism.
The THEA score is used to help estimate the risk of developing hypothyroidism within five years in people who have TPO antibodies, and can also help estimate the risk for those who have relatives with thyroid diseases.
Please note that thyroid antibodies make a very big contribution to the total THEA score.
How does THEA work? It applies a certain amount of points towards different measures. These measures consist of genetic predisposition as well as lab test results. I’ve included a chart (at the end of this article) that shows you how the scoring is made.
Genetic predisposition: We know there is a genetic component to developing Hashimoto’s, (remember the three conditions necessary: genetic predisposition, intestinal permeability and triggers) — and it tends to run in families. So, if you have relatives with Hashimoto’s, that increases your risk. And if you have been diagnosed with thyroid disease, there’s a greater chance that a loved one like your child, parent or sibling may be at risk as well.
Hashimoto’s can occur in two varieties: an organ wasting form (atrophic) associated with HLA-DR3 gene inheritance, and an enlarged thyroid (goitrous) form through HLA-DR5 inheritance.
People with these genes (which are common in the Caucasian population) and who have a relative with Hashimoto’s would get points. Someone with multiple relatives with Hashimoto’s would get additional points.
If they are showing high TSH levels, they will get points. If they have thyroid antibodies, they will get points; and the higher the level of antibodies, the higher the points.
What Does Your THEA Score Mean?
Ideally, we want a THEA score of 0. That is only possible without any genetic predispositions. With a genetic predisposition, the lowest score will always be a 2.
Low risk is considered in the 0-7 range. This means they are at a low risk of developing Hashimoto’s, or that their Hashimoto’s is not super aggressive at this point. Nonetheless, they are at risk. For a person with a genetic predisposition, with no other points – let’s say they score a 2 – they still have a 1.6 percent chance of being hypothyroid within 5 years. Keep in mind that if this same individual experiences more triggers, that will contribute to the disease progression.
The higher the score, the higher the aggressiveness rating, and the higher the chance of a person becoming hypothyroid within 5 years.
If we look at a score from 16-21, we know that the aggressiveness of the condition is very high and that they have about a 86 percent chance of becoming hypothyroid within 5 years. As we know that hypothyroidism is Stage 4 of Hashimoto’s, while other autoimmune conditions occur in Stage 5, higher thyroid antibodies may also predict a faster progression to other types of autoimmune conditions.
The THEA score can also be a great tool to measure progress in treating the disease. A person can’t remove the genetic predisposition score, but they can eliminate all their triggers and resolve intestinal permeability so that a reduction in thyroid antibodies – and an improved THEA score – is possible. I have seen some patients who no longer test positive for antibodies by eliminating their triggers. Plus, I have seen some patients actually be able to reduce their doses of thyroid medications or go off them completely.
What I hope for with my clients is that they can reduce their risk and eliminate their symptoms. And the best way to reduce the THEA score early-on is to reduce thyroid antibodies.
Thyroid Events Amsterdam (THEA) Score
So What’s Your THEA Score?
Do you know what yours is? If not, do a quick calculation now by taking the assessment — it is easy to do. Assign points as per the chart based on your TSH, TPO antibodies and family background. Again, low risk is considered in the 0-7 range. This means the Hashimoto’s is or would not be super aggressive. But, you are still at risk.
Once You Know Your THEA Score, How Can You Reduce It?
For a comprehensive answer to that question, read Part 2 of this article: Mechanisms to Reduce Thyroid Antibodies. I cover a wide variety of ways you can reduce one significant element of the THEA score: your thyroid antibodies.
References
- Wentz I. Top 9 takeaways from 2232 people with Hashimoto’s. Thyroid Pharmacist. https://thyroidpharmacist.com/articles/top-9-takeaways-from-2232-people-with-hashimotos/. Published June 22, 2015. Accessed June 26, 2015.
- Sategna-Guidetti C, Volta U, Ciacci C et al. Prevalence of thyroid disorders in untreated adult celiac disease patients and effect of gluten withdrawal: an Italian multicenter study. The American Journal of Gastroenterology. 2001;96(3):751-757. doi:10.1111/j.1572-0241.2001.03617.x.
- Bell DS, Ovalle F. Use of soy protein supplement and resultant need for increased dose of levothyroxine. Endocr Pract. 2001;7(3)193-4.
- Fruzza AG, Demeterco-Berggren C, Jones KL. Unawareness of the effects of soy intake on the management of congenital hypothyroidism. Pediatrics. 2012;130(3):e699-702. doi: 10.1542/peds.2011-3350
- Aghili R, Jafarzadeh F, Bhorbani R, Khamseh ME, Salami MA, Malek M. The association of Helicobacter pylori infection with Hashimoto’s thyroiditis. Acta Med Iran. 2013;51(5):293-296.
- Rajič B, Arapović J, Raguž K, Bošković M, Babić S, Maslać S. Eradication of Blastocystis hominis prevents the development of symptomatic Hashimoto’s thyroiditis: a case report. The Journal Of Infection In Developing Countries. 2015;9(07):788-791.
- Lauritano EC, Bilotta AL, Gabrielli M, et al. Association between hypothyroidism and small intestinal bacterial overgrowth. J Clin Endocrinol Metab. 2007;92(11):4180-4.
- Chatzipanagiotou, S., et al. Prevalence of Yersinia plasmid-encoded outer protein (Yop) class-specific antibodies in patients with Hashimoto’s thyroiditis. Clinical Microbiology and Infection. 2001;7(3): 138–143
- Shenkman L, Bottone EJ. Antibodies to Yersinia enterocolitica in Thyroid Disease. Ann Intern Med. 1976;85:735–739. doi: 10.7326/0003-4819-85-6-735
- Sterzl, Ivan I. Removal of dental amalgam decreases anti-TPO and anti-Tg autoantibodies in patients with autoimmune thyroiditis. Neuro-endocrinology letters. 2006;27 Suppl 1:25-30.
- Joung, Ji Young JY. Effect of iodine restriction on thyroid function in subclinical hypothyroid patients in an iodine-replete area: a long period observation in a large-scale cohort. Thyroid. 2014;24(9):1050-7256.
- Gärtner R, Gasnier BC, Dietrich JW, Krebs B, Angstwurm MW. Selenium supplementation in patients with autoimmune thyroiditis decreases thyroid peroxidase antibodies concentrations. J Clin Endocrinol Metab. 2002;87(4):1687-1691.
- Mazokopakis, Elias E et al. Effects of 12 months treatment with L-selenomethionine on serum anti-TPO Levels in Patients with Hashimoto’s thyroiditis. Thyroid. 2007:609-612.
- Rostami R, Aghasi MR, Mohammadi A, et al. Enhanced oxidative stress in Hashimoto’s thyroiditis: inter-relationships to biomarkers of thyroid function. Clin Biochem. 2013;46(4-5):308-12. doi:10.1016/j.clinbiochem.2012.11.021.
- Poncin S, Colin IM, Decallonne B, et al. N-Acetylcysteine
and 15 Deoxy-Δ12,14-Prostaglandin J2 Exert a Protective Effect Against Autoimmune Thyroid Destruction in Vivo but Not Against Interleukin-1α/Interferon γ-Induced Inhibitory Effects in Thyrocytes in Vitro. The American Journal of Pathology. 2010;177(1):219-228. doi:10.2353/ajpath.2010.091253. - Lee, Hae Sang HS. The natural course of Hashimoto’s thyroiditis in children and adolescents. Journal of pediatric endocrinology & metabolism. 2014;27(9-10):807.
- Höfling DB Low-level laser in the treatment of patients with hypothyroidism induced by chronic autoimmune thyroiditis: a randomized, placebo-controlled clinical trial. Lasers Med Sci. 2013;28(3):743-53.doi: 10.1007/s10103-012-1129-9.
- Nordio M, Basciani S. Myo-inositol plus selenium supplementation restores euthyroid state in Hashimoto’s patients with subclinical hypothyroidism. Eur Rev Med Pharmacol Sci. 2017;21(2 Suppl):51-59.
- Pegel K. MODUCARE® – A Brief History And Mode Of Action. Published in 2002. http://www.moducare.com/wp-content/uploads/2016/05/moducare-summary-of-research.pdf. Accessed February 1, 2018.
- Kvantchakhadze RG. Wobenzym® in the complex treatment of autoimmune thyroiditis. International Journal on Immunorehabilitation. 2002;4(1):114.
- Ott J et al. Dehydroepiandrosterone in women with premature ovarian failure and Hashimoto’s thyroiditis. Journal of the International Menopause Society. 2014.
- Schmeltz, Lowell R. Anatabine supplementation decreases thyroglobulin antibodies in patients with chronic lymphocytic autoimmune (Hashimoto’s) thyroiditis: A randomized controlled clinical trial. The Journal of Clinical Endocrinology and Metabolism. 2013;0021-972X.
- Wang J, Lv S, Chen G, et al. Meta-analysis of the association between vitamin D and autoimmune thyroid disease. Nutrients. 2015;7(4):2485-2498.
- Mackawy AMH, Mohammed AB, Mater AB. Vitamin D Deficiency and Its Association with Thyroid Disease. International Journal of Health Sciences. 2013;7(3):267-275.
- Chaudhary S, Dutta D, Kumar M, et al. Vitamin D supplementation reduces thyroid peroxidase antibody levels in patients with autoimmune thyroid disease: An open-labeled randomized controlled trial. Indian Journal of Endocrinology and Metabolism. 2016;20(3):391-398. doi:10.4103/2230-8210.179997.
- Antonelli A, Alberti B, Melosi A. Changes in markers of autoimmunity in patients with Hashimoto thyroiditis treated with intravenous immunoglobulins. Preliminary results. Clinical Therapeutics. 1992;141(9):37-42.
- Cornejo R, Venegas P, Goñi D, Salas A, Romero C. Successful response to intravenous immunoglobulin as rescue therapy in a patient with Hashimoto’s encephalopathy. BMJ Case Reports. 2010;2010:bcr0920103332. doi:10.1136/bcr.09.2010.3332.
- Drulović J et al. Hashimoto’s encephalopathy: a long-lasting remission induced by intravenous immunoglobulins. Vojnosanit Pregl. 2011;68(5):452-4.
- Nupur G, Arpeta G, Maria S, Robert TY. CALMING THE STORM – ROLE OF PLASMAPHERESIS IN THYROTOXIC CRISES. Presented as part of The Endocrine Society’s 95th Annual Meeting and Expo; June 15–18, 2013; San Francisco, CA.
- Boers P, Colebatch J. Hashimoto’s encephalopathy responding to plasmapheresis. Journal of Neurology, Neurosurgery, and Psychiatry. 2001;70(1):132. doi:10.1136/ jnnp.70.1.132.
- El-saadany H, Elkhalik MA, Moustafa T, et al. Thyroid dysfunction in systemic lupus erythematosus and rheumatoid arthritis: Its impact as a cardiovascular risk factor. The Egyptian Rheumatologist. 2014;36(2):71-78.https://doi.org/10.1016/j.ejr.2013.12.003
- Nevinsky, G. Effect of different drugs on the level of DNA-hydrolyzing polyclonal IgG antibodies in sera of patients with Hashimoto’s thyroiditis and nontoxic nodal goiter. Medical science monitor. 2001;7(2):201.
- Janegova A, Janega P, Rychly B, Kuracinova K, Babal P. Rola infekcji wirusem Epstein-Barr’a w rozwoju autoimmunologicznych chorób tarczycy. Endokrynologia Polska. 2015;66(2):132-136. doi:10.5603/ep.2015.0020.
- Kurozumi A, Okada Y, Arao T et al. Induction of thyroid remission using rituximab in a patient with type 3 autoimmune polyglandular syndrome including Graves’ disease and type 1 diabetes mellitus: A case report. Endocrine Journal. 2015;62(1):69-75. doi:10.1507/endocrj.ej14-0152.
- Gul Mert G. Hashimoto’s encephalopathy: four cases and review of literature. Int J Neurosci. 2014;124(4):302-6. doi:10.3109/00207454.2013.836706.
- Litwicka K et al. In women with thyroid autoimmunity, does low-dose prednisolone administration, compared with no adjuvant therapy, improve in vitro fertilization clinical results? J Obstet Gynaecol Res. 2014.
- Xu J, Bergren R, Schneider D, Chen H, Sippel RS. Thyroglobulin antibody resolution after total thyroidectomy for cancer. J Surg Res. 2015;198(2):366-370. doi:10.1016/j. jss.2015.03.094.
- Anita A. Kurmann et al. Regeneration of thyroid function by transplantation of differentiated pluripotent stem cells. Cell Stem Cell. 2015. DOI: 10.1016/j.stem.2015.09.004.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
I would really appreciate a response. I have struggled with this blooming disease for about 50 yrs, and am actually starting to lose the will to continue the fight, everything is just such an effort. I would really like to know what it is like to have energy ! !
Veronica- When I was first diagnosed with Hashimoto’s, I felt so alone. My doctor didn’t think it was a big deal, and none of my friends or co-workers had it. It wasn’t until I started to research online that I found others who were going through the same thing.
A couple of years after my diagnosis, I found Hashimoto’s 411, a closed Facebook group run by Alice Berry McDonnell. This group is amazing! It is comprised of an army of highly motivated, smart, supportive women and men (now 45,000+ strong), and each of them sharing ideas of what worked for them, things they were planning to try, and offering support to one another. The comfort I received from knowing that there were others going through the same challenges as I, was enormous.
https://www.facebook.com/groups/hashimotos411/
Ask questions. Post your thoughts. Scan the files. It is an absolutely amazing resource. Best of all it’s kept private from spammers.
Hi Izabella,
Re Veronica’s query, I have the same – my TPO is dropping (1300 in 2013 to 59 last month) however my TG has gone up from 209 in 2013 to 484 last month. I am not asking for a diagnosis, only information on the role of TG and the implications of rising levels.
Cheers
Michele
Michele – thank you for reaching out. <3 I wish I could give you more direct advice but, each person is different. I would advise you to ask your personal pharmacist or a trusted clinician who’s care you are under. I am not able to respond directly to these types of questions here.
My tsh was .01and my antibodies were 134 what does this mean? I’m tired all of the time, constipated and have had heart burn like crazy
Sheri – thank you for reaching out. I am so sorry you are struggling with fatigue. <3 Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Fatigue was the most debilitating symptom I experienced with Hashimoto’s. It actually started 8 years before I was finally diagnosed in 2009 after I got Mono (Epstein-Barr Virus) in college. I needed to sleep for 12 hours each night to be able to function, and by “function” I mean after hitting the snooze button on my alarm clock for two hours (ask my poor husband), I would drag myself out of bed and then had to drink 46 cups of caffeine everyday to keep myself awake. I often had Red Bull and Pepsi for breakfast, and was the epitome of “wired but tired”. I hope my articles help you get started 🙂
OVERCOMING THYROID FATIGUE
https://thyroidpharmacist.com/articles/top-10-tips-for-overcoming-hashimotos-fatigue
THIAMINE AND THYROID FATIGUE
https://thyroidpharmacist.com/articles/thiamine-and-thyroid-fatigue
Dearest Dr. Izabella Wentz,
At 39 I had problems with a lack of energy, dry brittle hair and nails (and, oddly, I was unable to wash hair dye out of my hair, with my hair simply feeling slimy), plus I experienced my first ever weight gain in my life! I’d spent my entire life underweight, being put on special diets to try and get me to gain weight from about age ten. My father and baby sister both had Hashimoto’s and diabetes, so I asked my internist to test me for thyroid disease and diabetes, pointing out my family history and my lifetime inability to gain weight (post baby, I was 6’ tall and weighed 125–and ate like a pig; I had no worries about the number of calories I put into myself). Rather than test me, at each of three successive appointments that occurred as I went from 135 to 253 {at diagnosis), he insisted my weight gain was due to my age— he was only a resident a little over ten years younger than I). In fact, I was 180 when he finally tested me, and when I next saw him I weighed 253, and when he opened my file he looked shocked when telling me, “How about that! You DO have hypothyroidism!” He so believed his theory about my age, despite evidence in front of him, that he never even checked my test results before then!
Is it possible to be hyperthyroid and then have Hashimoto’s make its entrance into your life? I was constantly tested for diabetes given my low weight (5’7” and 80 pounds at 13 and 5’10” and 104 at 15 for example) and my father having Juvenile Diabetes. I also have a younger sister with Graves. Is it common to have this combination in the same family?
Elizabeth – thank you fo reaching out and sharing your journey. <3 Graves and Hashimoto's are both autoimmune conditions that affect the thyroid. They are thought to be closely related. Sometimes one turns into the other. The difference is the site of the antibody attack. In Hashimoto's, the antibodies are found to thyroglobulin (in 80%) and thyroid peroxidase (TPO) enzyme (in 95% of people) Hashimoto's results in hypothyroidism and is usually treated with Synthroid and replacement hormone.
The same antibodies may be present in a smaller percentage of people who have Graves, but the main antibody is to the TSH Receptor (TSHR-Ab). Usually, people with Graves have hyperthyroidism, and they are treated conventionally with thyroid suppressing drugs (methimazole) or radioactive iodine to destroy the thyroid. At that point, the thyroid will no longer produce hormones on its own, and these people end up on Synthroid as well. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target.
Oftentimes patients will have additional autoimmune conditions. Most autoimmune conditions have common root causes, and a lot of times the things that are recommended for one autoimmune condition will help with others. Conditions that I have found to respond really well to the Hashimoto’s protocols have been rheumatoid arthritis, lupus, Celiac disease, irritable bowel syndrome, eczema, asthma, Graves’, premature ovarian failure, psoriasis, Alopecia Areata, and Sjogrens. I have also seen the protocols help with Fibromyalgia, chronic fatigue syndrome, PCOS, as well as Type 2 diabetes, Crohn’s, and Ulcerative colitis.
I hope this helps! You may find these resources helpful as well.
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Hashimoto’s Food Pharmacology
https://www.amazon.com/Hashimotos-Food-Pharmacology-Nutrition-Protocols/dp/0062571591?tag=thyroipharma-20
Hi doctor i have tpo results 388.82ui/ml
Where tsh is 4.850
Serum t3 1.39
Serum t4 6.90
Can you please tell me what is elevated tpo means to my body ? Everything ok or not?
Maryam – thank you for reaching out. <3 About 95% of people with Hashimoto's have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body's response.
Some people with Hashimoto’s test negative for thyroid antibodies because their overall immune health is so weak, they do not produce enough antibodies. I tested negative for antibodies several times. Now, I insist on a thyroid ultrasound. A thyroid ultrasound can be used to detect changes in the thyroid, associated with Hashimoto's. Given that Hashimoto’s is one of the leading causes of hypothyroidism worldwide, it's best to be certain, one way or another. I have written several articles about how to best decrease thyroid antibodies.
Here are some articles I think you might find helpful:
HASHIMOTO'S AND THYROID ANTIBODIES: PART 1
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
Hey, thank you so much for this article it is so informative and truly will help so many people. October last year I was told my thyroid levels were low again (I had previously been diagnosed with hypothyroidism 7 years prior with no fluctuations since) and quite low infact. It then took until February this year to reach the right dosage of lethyroxine. During that period I suffered with very heavy and prolonged menstrual cycles (sometimes lasting whole months to 6 weeks) fatigue and depression. Despite my tablets being correct in February I continued experiencing heavy menstruation until about late April where my nurse advised I had no choice but to go on Noriday. After weeks this sorted out my problem until i THINK I caught a virus from a spa and was ill for over 10 weeks with a cough, even more extreme fatigue, coughing, sore throat. Turns out my thyroid was actually enlarged which looking back I think this may have been the root of my cough and sore throat. I have no idea if I actually caught something or what happened but all I know is no anti biotics helped and I was very very ill. I somewhat recovered but had to get my thyroid looked at further due to the enlargement. I’ve just been told that I have thyroiditis and having done some research stumbled across hashimotos and I have never felt more sure of something my whole life. It makes the most sense to me, as to my symptoms… After all this is the second massive random decline my thyroid has had now in 7-8 years and the symptoms that have followed have matched hashimotos exactly. Unfortunately, I feel super unheard by my current ENT doctor who is currently referring me to a sleep specialist but has clearly noted I have thyroiditis. I have checked my medical records and stumbled across an anti body test (the only anti body test ever done) and my TPO was 2000. This was when I was just diagnosed with hypothyroidism yet nothing was ever done. To me that is a clear indication that I have experienced a hashimotos flare up and I am in the process of demanding another test be done to confirm my concerns.
It has been a stressful, lonely and testing time for me the past near enough year! I am done with the willy nilly, the going round the houses I want answers so I can move on with my life.
If you have any thoughts I would massively appreciate them from you.
Thank you again xxx
Lucy – thank you so much for sharing your journey. ❤️ I understand how hard it is to find a practitioner who will listen! I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources I hope you find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
WHERE DO I START WITH HASHIMOTO’S
https://thyroidpharmacist.com/articles/where-do-i-start-with-hashimotos/
OVERCOMING HASHIMOTO’S
https://thyroidpharmacist.com/articles/overcoming-hashimotos-in-the-new-year
The THEA score is very interesting – I’d love to know how often you’d have someone do this? would you have them do it when they first start addressing their thyroid issues and then redo it say every 3-6 months? Also, what if they do it initially when TSH is low and then a few weeks later TSH is now high (because they do have Hashimotos) i.e. TSH may be a changing number
Jewell- Hashimoto’s is a complicated condition with many layers that need to be unraveled. While conventional medicine only looks at each body system as a separate category, and is only concerned with the thyroid’s ability to produce thyroid hormone, Hashimoto’s is more than just hypothyroidism. I wanted to pass along these articles that I wrote. I hope they help 🙂
WHERE DO I START WITH HASHIMOTO’S
https://thyroidpharmacist.com/articles/where-do-i-start-with-hashimotos/
OVERCOMING HASHIMOTO’S
https://thyroidpharmacist.com/articles/overcoming-hashimotos-in-the-new-year/
Victoria- Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically, is ‘dead’, or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target. We need to re-balance the immune system to prevent this (sometimes the autoimmunity can be reversed as well). The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition.
HASHIMOTO’S ROOT CAUSE BOOK
http://www.amazon.com/gp/product/0615825796?ie=UTF8&camp=1789&creativeASIN=0615825796&linkCode=xm2&tag=thyroipharma-20
Thank you Izabella for clarifying. I’ve been following your posts after I found your book at the library. I had my thyroid removed 12 years ago due to difficulties with swallowing because of a nodular goiter and it was said at the time that there was Hashimotos found as well as a small cancer which wasn’t treated due to its small size. This is the first time I’ve read that I could still be affected by Hashimotos even without a thyroid. I’ll take the information you share more seriously now and look at root cause info too. Thank you!
Dora – you are very welcome! Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target.
We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are the links to my books:
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Carol- I’m very hesitant in recommending iodine in Hashimoto’s. Although iodine serves as fuel for our thyroid and is very important in iodine deficiency hypothyroidism, Hashimoto’s is a different mechanism. It’s like pouring gas into an engine that’s on fire… that’s essentially what’s happening in Hashi’s, thyroid inflammation, and adding iodine to the mix before putting out the fire and fixing the engine may result in further damage to the thyroid. In those with a predisposition to autoimmunity, this has been documented time and time again, animal and human studies. I have spent 4 years researching this and have seen too many people suffering the consequences of adding iodine too soon. My approach is, let’s fix the engine first (usually a gut issue), and then add the fuel once we know that the engine is no longer on fire. Hope that you will check out my book. I have a whole chapter on the iodine controversy that references numerous studies as well as the work of Abraham and Brownstein.
AMAZON
http://www.amazon.com/gp/product/0615825796?ie=UTF8&camp=1789&creativeASIN=0615825796&linkCode=xm2&tag=thyroipharma-20
How do you feel about Iodine supplement if blood test results are low?
My Iodine result is 49 (52-109)
Thanks,
Richard S
Richard – thank you for following this page. While iodine can be a trigger for Hashimoto’s and can exacerbate Hashimoto’s, some people may be deficient and may benefit from a low dose iodine supplement (up to 250 mcg has been well tolerated in people with Hashimoto’s. Most multi and prenatal vitamins will contain anywhere from 150-250 mcg). I have more information about iodine in the Advanced Protocols in Hashimoto’s Protocol.
Hashimoto’s Protocol
thyroidpharmacist.com/protocol
Michelle- Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically, is ‘dead’, or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target. We need to re-balance the immune system to prevent this (sometimes the autoimmunity can be reversed as well). The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition.
HASHIMOTO’S ROOT CAUSE BOOK
http://www.amazon.com/gp/product/0615825796?ie=UTF8&camp=1789&creativeASIN=0615825796&linkCode=xm2&tag=thyroipharma-20
Carla- Most conventional physicians use the TSH test to determine if one has a thyroid disorder and to dose thyroid medications.
However, this test can often times be misleading, as levels of circulating hormones may fluctuate at different times, such as in Hashimoto’s, the person affected may fluctuate between highs and lows.
Additionally, when scientists first set the “normal” ranges of TSH for healthy individuals, they inadvertently included elderly patients and others with compromised thyroid function in the calculations leading to an overly lax reference range.
This resulted in people with underactive thyroid hormones being told that their thyroid tests were “normal,” based on this skewed reference range.
WHAT TO DO IF YOUR TSH IS NORMAL AND YOU ARE ANYTHING BUT
https://thyroidpharmacist.com/articles/what-to-do-if-your-tsh-is-normal-and-you-are-anything-but
Here are the tests you need for diagnosis. Most endocrinologists don’t run them all so you will have to request them. Make sure to request a copy of your labs as well.
TOP 6 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests
Dr. Isabella! I listened to all of your Thyroid Secret series. I have never been tested for thyroid other than just the normal blood tests. I really don’t believe I have a thyroid issue (don’t have most of the thyroid symptoms). My question here is, my husband has alopecia universalis (as of age 15 & now going on 53). His issue is he gets sweats (just sitting at the table- not referring to typical sweats caused by exercise etc). He breaks out in sweat beads over his bald head & his eyes just automatically open wide. I can tell from his eyes he is about to break out in a sweat. All very annoying for him! He is going to do an elimination diet (cave man diet). What blood tests do you recommend? Won’t do the blood tests til Autumn 2017. Thank you for all of your assistance and everything you went through yourself while trying to discover thyroid issues!
Katlynn – thank you for following this page.
Did you know that if you live in the United States, Australia, Europe and most developed countries that add iodine to the salt supply and take thyroid medications, there’s a higher probability that you do have Hashimoto’s?
Depending on the source, estimates are that between 90-95% of those with hypothyroidism have Hashimoto’s.
But most doctors will never tell people that they have Hashimoto’s, or that their own immune system is attacking their thyroid. People are told that their “thyroid is sluggish”, and that these things happen with age and “Just take this pill, you’ll be fine.” I hope you check out these articles that I wrote.
ARE YOU DOING EVERYTHING FOR YOUR THYROID BUT NOT YET WELL?
https://thyroidpharmacist.com/articles/are-you-doing-everything-for-your-thyroid-but-not-yet-well/
DO YOU HAVE HYPOTHYROIDISM OR HASHIMOTO’S OR BOTH?
https://thyroidpharmacist.com/articles/do-you-have-hypothyroidism-or-hashimotos-or-both/
Here are the tests you need for diagnosis. Most endocrinologists don’t run them all so you will have to request them. Make sure to request a copy of your labs as well.
TOP 6 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
This link, for the tests is taking me to an error message. Please update the link. Thank you!
Loop
Vivienne – thank you for following this page. All links are functioning properly. Should you still require assistance, please, contact info@thyroidpharmacist.com, and they’ll be happy to help. 🙂
Carla- I highly recommend that you work with a functional medicine clinician. It’s a whole medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
Matty- There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication you are looking for, ask your local pharmacist for doctors in your area who prescribe the medication you are looking to try. Have you read these articles?
WHICH THYROID MEDICATION IS BEST?
https://thyroidpharmacist.com/articles/which-thyroid-medication-is-best/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
Dianne- There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication you are looking for, ask your local pharmacist for doctors in your area who prescribe the medication you are looking to try. Have you read these articles?
WHICH THYROID MEDICATION IS BEST?
https://thyroidpharmacist.com/articles/which-thyroid-medication-is-best/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
Diane- These are the recommended labs from my book, page 32.
RECOMMENDED THYROID FUNCTION TESTS
TSH
TPO Antibodies
Thyroglobulin Antibodies
Free T4
Free T3
Reverse T3 (Optional)
Have you read my book, Hashimoto’s The Root Cause? Here’s the link in case you’re interested.
http://www.amazon.com/gp/product/0615825796?ie=UTF8&camp=1789&creativeASIN=0615825796&linkCode=xm2&tag=thyroipharma-20

HOW TO GET ACCURATE LAB TESTING WHEN TAKING MEDICATIONS
https://thyroidpharmacist.com/articles/how-to-get-accurate-lab-tests-when-taking-thyroid-medications
Hi Izabella,
I was wondering if you knew anything about the new lab test assay for TPOAb from Beckman Coulter (see https://www.beckmancoulter.com/wsrportal/bibliography?docname=DS13437A%20Access%20TPO%20Ab%20WW%20Data%20Sheet.pdf). I used to get my labs done with the ranges you have on this page (I believe it is the Siemans assay – normal is < 20 IU/mL). Then the lab switched to Beckman Coulter which is measured differently (0-0.9 IU/mL is normal range). I've not found anything online that compares the tests. One lab suggested that patients get both assays done to do a one-time comparison to get a baseline. The Beckman Coulter test came up a lot in searches where people were talking about how it is used for Thyroid cancer patients. I was wondering if you had heard about this new assay and if you had any information about comparing Siemans to Beckman Coulter. Thanks for all the great work and information! Cheers, Jill
Jill- I’ve negotiated better pricing with Direct labs for the Facebook group Hashimoto’s 411. You will get them here cheaper than going through most other places. If you would like to order your own labs, you can use the link below.
DIRECT LABS AND HASHIMOTO’S
https://www.directlabs.com/thyroidrx/OrderTests/tabid/29159/language/en-US/Default.aspx
Also, much of the information required to get your health back is covered in my book, Hashimoto’s: The Root Cause. You might be interested in checking it out.
http://www.amazon.com/gp/product/0615825796?ie=UTF8&camp=1789&creativeASIN=0615825796&linkCode=xm2&tag=thyroipharma-20
Hi Jill,
I have the exact same question. Did you find any answers to this..? If so, it will be useful for me if you could share.
Hi, I am just looking for a little advice. I have had hypothyroid symptoms for 10 years, including weight gain and an inability to lose weight (despite intense exercise 6-7 days/week and calorie intake of ~1800-2000 kcal), thinning head hair, muscle cramps and weakness, fatigue and brain fog, feeling like my memory is much worse than it used to be even though I am just 24, always feeling cold, etc. My TSH was 1.28 in 2008, 2.0 in 2014, 3.5 this month (Jan 2017). My doctor said these are just normal variations and everything was fine. After developing episcleritis a couple times in the past two months, I pushed for antibodies (feeling, like others, like my doctor thought I was a hypochondriac and nothing is wrong) and my TPO ab was normal at 3 IU/mL (ref. range <9 IU/mL) but my Tg ab was elevated at 5 IU/mL (ref. range <1 IU/mL). My doctor just said everything was fine. Do you think Hashimoto's is a possibility here? Seems like others who have eleveated antibodies have numbers 1-3 orders of magnitude higher than the reference range upper limit, so mine does not really seem 'that' high, but I feel like something is wrong and just do not know what.
Celena – thank you so much for following this page.
Did you know that if you live in the United States, the UK, Australia, Europe and most developed countries that add iodine to the salt supply and take thyroid medications, there’s a higher probability that you do have Hashimoto’s?
Depending on the source, estimates are that between 90-95% of those with hypothyroidism have Hashimoto’s.
But most doctors will never tell people that they have Hashimoto’s, or that their own immune system is attacking their thyroid. People are told that their “thyroid is sluggish”, and that these things happen with age and “Just take this pill, you’ll be fine.” I hope you check out these articles that I wrote.
ARE YOU DOING EVERYTHING FOR YOUR THYROID BUT NOT YET WELL?
https://thyroidpharmacist.com/articles/are-you-doing-everything-for-your-thyroid-but-not-yet-well/
DO YOU HAVE HYPOTHYROIDISM OR HASHIMOTO’S OR BOTH?
https://thyroidpharmacist.com/articles/do-you-have-hypothyroidism-or-hashimotos-or-both/
Here are the tests you need for diagnosis. Most endocrinologists don’t run them all so you will have to request them. Make sure to request a copy of your labs as well.
TOP 6 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
If you have time, does a TPO Ab result of 44 indicate hashimoto’s? I am hearing women talking about their levels being in the 1000s. 44 seems pretty benign comparatively. (Incidentally, if it helps, my TAA Ab were 19, FT3 – 3.4, Total T3 – 1.23, Free T4 – 1.29, Total T4 – 10.6). I am 46, and have been having low thyroid symptoms for at least 15 years. Thank you for all you’ve done!
(Sorry, missed the ones on the next page! TSH was 1.26, and Triiodothyronine resin uptake (T3RU) was 34.6. I haven’t had a thyroid ultrasound.)
Laurie – I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
WHAT TYPE OF DOCTOR SHOULD YOU SEE IF YOU HAVE HASHIMOTO’S
https://thyroidpharmacist.com/articles/what-type-of-doctor-should-you-see-if-you-have-hashimotos
10 THINGS I WISH MY ENDOCRINOLOGIST WOULD HAVE TOLD ME
https://thyroidpharmacist.com/articles/10-things-i-wish-my-endocrinologist-would-have-told-me
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
I will read, these, thank you. There’s a DC near me who specializes in thyroid. I’ve been seriously thinking about working with him. He’s been highly recommend to me. Thank you.
What did you find out about that TPO level, Laurie? Mine is 35 with a lab range <101 so my doctor says I'm negative but I'm seeing elsewhere that's positive.
My almost 16 year old daughter was seen in ER twice in early December… Air hunger (yawning, sighing, having to force self to take deep, satisfying breath), palpitations, short of breath with activity… in late fall had a root canal… was concerned about endocarditis…blood cultures and echo negative… ekgs, cxr, cbcs and chemistries WNL.. had noticed in late fall she also looked to have a puffy face, weight gain in abdomen, acne on chin, constipation, menstrual cycle just slightly irregular, napping in afternoons, joint pain (she is a dancer and horseback rider, had her tested for lymes which is negative so far) thyroid gland slightly more noticable on neck… other labs..b12 439, freet4(direct)1.26, T3 138,tsh 4.49, TPO 7… Md presumed hashis but antibodies low.. treating for a thyroiditis with armour… she is feeling much better but wondering if hashis still possible with negative antibodies.. would she benefit from ultrasound?? since summer fluctuates constipation and diarrhea..thought maybe lactose intolerance.. since late december hiccups frequently… since starting meds energy much better.. air hunger and palpitations gone..able to exercise again…
Jen – my heart goes out to you and your daughter. 🙁
I highly recommend that you work with a functional medicine clinician. It’s a whole medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
WHAT TYPE OF DOCTOR SHOULD YOU SEE IF YOU HAVE HASHIMOTO’S
https://thyroidpharmacist.com/articles/what-type-of-doctor-should-you-see-if-you-have-hashimotos
10 THINGS I WISH MY ENDOCRINOLOGIST WOULD HAVE TOLD ME
https://thyroidpharmacist.com/articles/10-things-i-wish-my-endocrinologist-would-have-told-me
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
So ive been trying to get pregnant for the last year. Husbands sperm is not exactly the best so hes in the midst of changing lifestyle and taking vitamins to improve it. However while waiting for his sperm to improve ive had my thyroid tested, the results are as follows :
Thyroid Stimulating Hormone [TSH]
RESULT 1.94
RANGE 0.32-4.00mIU/L
Thyroxine Free [Free T4]
RESULTS 13
RANGE 9-19pmol/L
Triiodothyronine Free [Free T3]
RESULT 3.8
RANGE 3.1-6.2pmol/L
Thyroglobulin Antibody
HI
RESULTS 469
RANGE < 40kIU/L
Anti-Thyroglobulin antibody values up to 800
kIU/L may be seen in healthy people without
demonstrable thyroid disease.
Thyroperoxidase Antibody
RESULT 31
RANGE < 35 kIU/L
Does this indicate a thyroid issue? something that needs to be solved before trying to get pregnant?
I am a 32 year old female and i have an 8 year old son, not sure if that changes anything.
Thanks in advance!
Cortney – thank you for following this page.
Please, understand that due to liability issues, I am unable to answer specific medical questions.
I highly recommend that you work with a functional medicine clinician. It’s a whole medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
WHAT TYPE OF DOCTOR SHOULD YOU SEE IF YOU HAVE HASHIMOTO’S
https://thyroidpharmacist.com/articles/what-type-of-doctor-should-you-see-if-you-have-hashimotos
10 THINGS I WISH MY ENDOCRINOLOGIST WOULD HAVE TOLD ME
https://thyroidpharmacist.com/articles/10-things-i-wish-my-endocrinologist-would-have-told-me
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
Cortney Farrell, I’m wondering if you were able to obtain a diagnosis? I’m in a similar situation, been TTC for almost 2 years, 29 years old, otherwise healthy, but recent blood work indicated elevated prolactin, and thyroid Antibodies came back with numbers very similar to yours.
I haven’t got a call from the endocrinologist’s office, hoping to do a follow up, as I don’t really understand these numbers.
Wondering how you’re doing now, and if you were able to get any info on this? Thanks in advance 🙂
Hi Izabella,
My TPO came back as 9.57 (0.00-34.00) and TGAB 470.00 (0.00-115.00).
I have hyperthyroid symptoms but GP says the antibody results are normal. Is this correct?
TSH 3.17 (0.27-4.20)
T4 62 (59.00-154.00)
T3 3.43 (3.10-6.80)
Many thanks
Shcl85 – thank you for following this page.
Graves and Hashimoto’s are both autoimmune conditions that affect the thyroid. They are thought to be closely related. Sometimes one turns into the other. The difference is the site of the antibody attack. In Hashimoto’s, the antibodies are found to thyroglobulin (in 80%) and thyroid peroxidase (TPO) enzyme (in 95% of people)-Hashimoto’s results in hypothyroidism and is usually treated with Synthroid and replacement hormone.
The same antibodies may be present in a smaller percentage of people who have Graves, but the main antibody is to the TSH Receptor (TSHR-Ab). Usually, people with Graves have hyperthyroidism, and they are treated conventionally with thyroid suppressing drugs (methimazole) or radioactive iodine to destroy the thyroid. At that point, the thyroid will no longer produce hormones on its own, and these people end up on Synthroid as well.
Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target.
We need to rebalance the immune system to prevent this (sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition.
Hashimoto’s Root Cause
http://www.amazon.com/gp/product/0615825796?ie=UTF8&camp=1789&creativeASIN=0615825796&linkCode=xm2&tag=thyroipharma-20
Hashimoto’s Protocol
thyroidpharmacist.com/protocol
Thank you for all you do to help those of us finding our way through the fog of Hashimoto’s Disease!! I also have MTHFR and can not absorb Vitamin B’s and take them sublingually. I also have lipid deposits on top and bottom of my eyelids and increasing since my diagnosis almost two years ago. Still searching to determine my trigger! Do you have any suggestions for either or both and I do have a wonderful functional medicine doctor but thought you might know something helpful? I continue to feel rotten… My thanks again. Jan
Jan – thank you for following this page and for your support. <3
When I was first diagnosed with Hashimoto’s, I felt so alone. My doctor didn’t think it was a big deal, and none of my friends or co-workers had it. It wasn’t until I started to research online that I found others who were going through the same thing.
A couple of years after my diagnosis, I found Hashimoto’s 411, a closed Facebook group run by Alice Berry McDonnell. This group is amazing! It is comprised of an army of highly motivated, smart, supportive women and men (now 45,000+ strong), and each of them sharing ideas of what worked for them, things they were planning to try, and offering support to one another. The comfort I received from knowing that there were others going through the same challenges as I, was enormous.
https://www.facebook.com/groups/hashimotos411/
Ask questions. Post your thoughts. Scan the files. It is an absolutely amazing resource. Best of all it’s kept private from spammers.
Hi Dr Wentz,
I love your work, you are amazing!
My TPO antibodies went from over 10,000 to 120 in 14 years, but my need for thyroxine pills didn’t change. Now they’re only 20! I don’t know how that happened, but I still officially have Hashimoto’s right? Is it in “remission”, even though I’m dependent the Natural Dessicated Thyroid that I now take?
Thank you so much for your incredible research and outreach.
Suzie – thank you for following this page.
Thyroid tissue can regenerate, but the rate at which it does is not always predictable. Thus, some are able to stop the autoimmune attack on their thyroid and regain normal thyroid function. Others can reduce the dose of medications, and others will need to stay on the medications indefinitely. I’m currently working on some protocols to help with tissue regeneration.
Reversing Hashimoto’s means different things to different people. For some, it means a reduction in symptoms, and for others, it means a reduction in your antibodies. I had both. Here a few articles that might be helpful for you 🙂
IS IT POSSIBLE TO RECOVER THYROID FUNCTION IN HASHIMOTO’S
https://thyroidpharmacist.com/articles/is-it-possible-to-recover-thyroid-function-in-hashimotos
REVERSING AUTOIMMUNITY? AND THE PERFECT STORM
https://thyroidpharmacist.com/articles/reversing-autoimmunity-and-the-perfect-storm/
HASHIMOTO’S SELF CARE, GETTING AND STAYING IN REMISSION
https://thyroidpharmacist.com/articles/hashimotos-self-care
Hello,
I was diagnosed with SIBO last year but have had numerous symptoms relating to SIBO and gut dysbiosis for years. I truly believe that having two parents who smoked in the house while I was little contributed to that. Additionally mold was found in my bedroom years ago. I have been on herbal antibiotics and allicin for about a year on and off. I have suspected Hashimoto’s disease for years and experience things like fatigue, complete loss of eyebrows, brittle hair (although no hair loss). Some of my symptoms have gotten much better after the elimination of Gluten, Dairy, Soy, Preservatives, etc like my eyebrows have started growing back. The fatigue however is horrible at different times of the day and the acid reflux has never really gone away completely depending on what I eat! The biggest roadblock to my recovery is the lack of cooperation from Canadian doctors. I live in Canada and I received my SIBO test and diagnosis from a Practitioner based in the US as 4 doctors here all told me that this bacteria is controversial and is not considered by OHIP to be first course of treatment. They ALL wanted to treat me with proton inhibitors for Acid Reflux (which I still have) but refused to test me for SIBO. In the US, if you make a compelling argument for why you need a test, the doctors will work with you. In Canada this is not the case. Is there anything I do to obtain these tests on-line in order to start towards my road to recovery…..
Thank you so very much for your help
Lella – thank you for following this page and for sharing.
I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
Thank you Izabella, for all the information you put out there for us! The information on this page is exactly what I needed to interpret my lab results. My GP said I have early Hashimoto’s and wants to do another blood test in three months , but only TSH (now 4,5) and T4 (now 10,4), because according to him it won’t matter anymore what the antibodies’ number is (now 421). He will offer no treatment, so he basically leaves me waiting for worse to come. Since I have suffered severe fatigue and many other symptoms that feels like being left out in the woods by conventional medicine. But… I’m glad to also start working with a doctor for integral medicine and very happy to be a much better informed patient thanks to your work. I will buy your books but already got started with the information on your website and elsewhere on the internet, like the podcast with Robb Wolf – very informative, I listened to it twice!
Els – thank you for following this page and for your support.
I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
Thanks! I will do that and check out those pages. I’m so happy I do not have to ‘just wait’, but there is help, information and lots of things I can do myself.
I found my practitioner in the Netherlands with some difficulty, but I feel understood and am confident we can work together towards better health for me.
Els – I’m so glad you found someone who can work with you! I hope you find this article helpful as well:
10 MOST HELPFUL DIY INTERVENTIONS FOR HASHIMOTO’S
https://thyroidpharmacist.com/articles/10-most-helpful-diy-interventions-for-hashimotosaccording-to-my-clients
Do you think nutritional/ supplement intervention is enough to treat/ reverse Hashimoto’s and hypothyroid symptoms?
I got my blood test result back (TSH 3.88, fT3 2.38, TPOab 12 iu) but a local doctor says TPOab is not enough to put me on medication.
I have little time left in the United States and I doubt there is anybody in my own country who would take me seriously.
I have looked at your clinician list but it doesn’t list my country.
Robin I have a 12 week online program called Hashimoto’s Self-Management Program that covers all of the strategies that I go through with my one-on-one clients, in a self-paced format, so that participants have access to all of the things I’ve learned about Hashimoto’s without having to schedule costly consults with me or another practitioner. In addition, any person that goes through the program will get access to a Quick search Q&A Database of 1000+ questions asked by past program participants, Root Cause Assessment based on 100’s of my clients’ root causes and triggers, 2-week Meal Plans, recipes, and shopping lists to get you started on the following diets: Paleo, Autoimmune Paleo, SIBO, Candida. Also, Discounts on lab tests, high-quality supplements, and consultations and much more to support you in your journey! There are a few requirements that you should pay attention to, such as my book is a required read. Hashimoto’s Self-Management Program http://hackinghashimotos.com/ I also have a team of consultants who I’ve personally trained on the protocols outlined in my books and program. Generally, the team will give priority for consultations to those who have read the book and completed the program. You can find out more about my team and consulting services here. https://www.thyroidpharmacistconsulting.com/pages/meet-the-thyroid-pharmacist-team
Hi Izabella,
I have TSH = 0.014
T3 : 1.58
T4 : 3.58
Anti TPO IGG : 119
What do you recommend ? Why the values are like this ?
Mithun – Thank you for following this page. Please, understand that due to liability issues, I am unable to answer specific medical questions, but I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
Thank you so much Dr Izabella for all this useful info! I suspected I have Hashimotos (many of the symptoms, issues conceiving/miscarriages, and mother who has it). My TSH is 2.3, my TPO is 16. My obgyn says those numbers are fine. Would you recommend getting a second opinion? Also my progesterone was low (1.4 mid luteal phase). Should I focus on progesterone, thyroid, or both? Do they affect each other? I just don’t know where to start, and we just want to have a baby! Thanks!
Annelies – thank you for following this page. I understand how frustrating this can be and my heart goes out to you! <3 Here are some article you might find helpful.
KAREN'S HASHIMOTO'S SUCCESS STORY
https://thyroidpharmacist.com/articles/karens-root-cause-of-thyroid-symptoms
PREGNANCY
https://thyroidpharmacist.com/articles/hashimotos-and-pregnancy
I have done a blood test recently.
TSH : 6.59 mIU/L
Thyroglobulin Ab : 33.07 IU/mL
Thyroid Peroxidase Ab : 516.00 IU/mL
Is this a sign of Hashimoto?
Dev – Thank you for following this page. Please, understand that due to liability issues, I am unable to answer specific medical questions, but I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
Hello There Dr Izabella~!
I am leaving a reply in hopes to find some help… I have told my Dr for 2 years+ that I KNOW my thyroid is off. While my T4-Free has been in what she would call the “high normal range” she would NEVER test further and treat me like I was some sort of hypochondriac. It took a random event over the summer while on vacation where I gained 20-lbs of water weight to have a Dr run all my panels that I was afraid of because I had no underlying heart condition to have this happen….
SO my question is this- with all of my labs I have SEVERAL concerns that point to several autoimmune disorders.
My Thyroid Peroxidase Antibodies is at an 84 (eighty-four) where it says high is <9 IU/mL
DNA (DS) AB, High Avidity 12.3
Complement Component C3C was 144
Complement Component C4C 17
Myeloperoxidase Antibody was <1.0 (AI) Active or detected
Then at the end of this it lists 5 different things this "could" be such as microscopic polyangitis, etc all the way to Wegners Granulomatosis.
My Angiotensin-1-Converting Enzyme @67
Anti Mulleriam Hormone Assessr at 1.82 (I am 35 years old and so it says I should have a number greater than 9.24)
I tested positive for several "molds"?
Cladosporium Hebarum (M2) IgG @ 35.5 (14.7=max)
Penicillium Notatum (M1) IgG @ 26.3 (17.5=max)
Phoma SPP IgG @ (10.4) (6.6=max)
Aureobasidium Pullulans (M12) IgG @ 12.1 (13.6=max)
Alternaria Tenuis IgG @8.9 (13.6=max)
Truchoderma Viride (M15) IgG @ 6.2 (13.4 max)
Pullulans IgG (did not say what it was at, only that it was present)
Alternata (M6) IgG (did not say what it was at, only that it was present)
asp.fumigatus IgG 22.7
*I was tested for "Valley Fever" and that came up as negative (or so I am reading- if I am interpreting what it is stating.
I had en echo, doppler, ct with contrast, lumbar ct scan and xtray. I had 2 nodules in my lungs that caused for the EXTENSIVE panel of bloodwork. My echo showed some leakage in my heart valve (the intake valve- sorry for the non medical terminology) and my ejection fraction was approximately 60%. My degenerative disc disease that was "diagnosed" when I was 28 is now full arthritis in my lower spine (and my neurologist suspects my knees as well) I have 53% conductivity in the nerves from my spine to my toes (I am on gabapentin for this).
WITH ALL OF THIS- My dr is not taking me seriously. I had these labs done 2 days before flying back to the Pac NW) and when I came back it was brushed off. So I saw another Dr in the same office to see if anything will change with my full care- I am seeing a pattern here…. I had bloodwork to once again do "basic" thyroid levels (per the phlebotomist) on Friday 10/27 (non-fasting!?!?)
I was told when I was young I had endometroisis… however the problems persisted after giving birth to my one and only child 8.1 years ago. Now the drs "think" I have PCOS
My mom has lupis and is Stage 4 (I am leaving in 5 days to be with her- may not make it to Christmas) Leiomayosarcoma (Smooth muscle tissue cancer). My 15 year old brother died from Osteosarcoma that metastasized into his lungs. My sister who is 2 years younger than I has rheumatoid arthritis, a prolapse heart valve and a prolapse uterus.
HELP? What would you say is going on based on those labs?
Natasha – Thank you for following this page. Please, understand that due to liability issues, I am unable to answer specific medical questions, but I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms. Here are some links which might help:
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
MY RECENT CHALLENGES AND FINDING DR. RIGHT
Hi, dr Wentz. To me, one intervention was extremely important. Actually first I cut out gluten (I made my bread and everything that required flour with a flour mix that contained: corn flour, rice flour and buckwheat flour). My ATPO dropped from around 1400 to 600. Then several months I kept cutting gluten. Then found out about the Paleo diet, so I cut into half the amount of Gluten free flour with Paleo flour(so I used a mix of 1/2 Gluten free flour: corn flour, rice flour and buckwheat flour, and 1/2 Paleo flour that containd a mix of sweet potato flour+sesame flour+ cocnut flour+ psyllium husk). The result was amazing: my ATPOs dropped from around 600 to around 300. Unfortunately I can’ cut the gluten free flour as I get really hungry – I have 2-3 days/ week when I eat completely vegan, and the rest meals that contains meat. Do you have any idea about the science behind cutting grains/ why do grains stimulate the creation of antibodies? PS: I keep my anti-thyroglobulin under control by taking 200mcg of Selenium with 400 UI of vitminE, but, to me increasing vitamin D did not decrease my ATPOs.
Ionela – thank you for following this page. I always recommend starting with the diet. Are you gluten, dairy, corn and soy free? Are they eating a nutrient dense diet with fermented foods? Did you know that reactive foods trigger an inflammatory response in the GI tract, leading to malabsorption of nutrients (gluten sensitivity, in particular, has been implicated in causing a Selenium deficiency, a well-known risk factor for Hashimoto’s), and can also produce intestinal permeability whenever they are eaten?
Most people will see a dramatic reduction in gut symptoms, brain symptoms, skin breakouts, and pain by eliminating the foods they are sensitive to. Some will also see a significant reduction in thyroid antibodies! An additional subset of people will actually be able to get their Hashimoto’s into complete remission just by getting off the foods they react to, normalizing their thyroid antibodies, and some even normalizing their thyroid function! Here are a couple of articles you may find helpful.
FOOD SENSITIVITIES AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/food-sensitivities-and-hashimotos
AUTOIMMUNE PALEO DIET
https://thyroidpharmacist.com/articles/autoimmune-paleo-diet
Hi Dr. Izabella…..this info is quite helpful, thanks!
I would highly appreciate if you can provide your thoughts to my case. My father has recently been facing memory loss issues where a few neurologists concluded it to be Dementia. Thats when some doctor recommended him the THYROID ANTIBODIES SERUM BLOOD TESTS. So as per the reports, his Anti-Thyroglobulin Antitbodies is 209.60 and Anti-Thyroid Peroxidase Antibodies is > 1300.00, which is exceptionally high. The method adopted for both was Chemluminescence? What can we conclude from this? what do these high levels mean? Is this related to the memory loss issues also?
Thanks so much!
regards,
Kriti – thank you for following this page. Please understand, I am not able to respond directly to these types of questions here. I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
Here are some articles you might find interesting as well.
TOP 10 THYROID TESTS AND HOW TO INTERPRET THEM
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
SUBCLINICAL HYPOTHYROIDISM DESERVES CARE AND TREATMENT
https://thyroidpharmacist.com/articles/patients-subclinical-hypothyroidism-deserve-care-treatment/#
WHAT DOES IT FEEL LIKE TO HAVE THYROID DISEASE?
https://thyroidpharmacist.com/articles/what-does-it-feel-like-to-have-thyroid-disease
Is it possible for someone with hashimo’s to have both an under active thyroid and then when retested 3-6 months later fall within the “normal” range?
Miranda – Thanks for reaching out ! I do recommend starting off with these thyroid function tests:
¨ TSH
¨ TPO Antibodies
¨ Thyroglobulin Antibodies
¨ Free T4
¨ Free T3
¨ Reverse T3 (optional)
¨ Thyroid Ultrasound (optional)
It’s always best to speak to your functional medicine practitioner to evaluate your specific case, and whether you need more testing. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
I recently read this article by dr Alan Christiansen; https://drchristianson.com/the-4-things-you-need-to-know-about-thyroid-antibodies/.
It speaks of how the antibodies can go up and down and not be related to any specific changes/interventions you may and may not do. It makes it obviously very hard for those of us implementing changes to track if something is in fact having an effect on our conditions. Do you have any advice or suggestions to go around this problem?
Titti – thank you for following this page. IgG subclass antibodies have a half-life of 21 days, and stick around on immune cells for about two to three months. They need constant “reminders” in the form of an antigen so that their production continues. If the antigen is removed, the antibodies will go away as well. The time period required for them to completely forget about the antigen and disappear is nine to twelve months.
The following things need to be in place for the antibodies to forget about the thyroid:
1) The thyroid stops expressing TPO.
2) The thyroid cells are not damaged and able to regenerate.
3) There are no substances that look like TPO (glandulars, gluten, infections, other triggers).
4) The immune system is balanced.
5) The autoimmune cells are confused by a decoy.
Some of these requirements are quick and easy, and others will take some time …
The thyroid will stop expressing TPO for two reasons. One of them is thyroid destruction, which we do not want; the other is thyroid suppression. Thyroid suppression is induced by limiting iodine and taking a thyroid supplement to bring TSH to 1 mIU/L or so. This can take up to three months
In the case of autoimmune conditions, traditional and alternative medicine practitioners may focus on rebalancing the immune system (i.e. steroids and immune-modulating drugs used in traditional medicine, or else herbs, supplements, or acupuncture used in alternative medicine).
While this approach may be helpful for taming the immune system in the short term or overcoming autoimmune flares, it is often a temporary solution and the immune system may become imbalanced again once the medications, acupuncture, and herbs and supplements are stopped if the underlying issue that lead to the immune system imbalance is not addressed. Thus we can say that immune modulation treats only the symptoms, and not the root cause.
As we can’t change genes, our approach to addressing the root cause of Hashimoto’s is threefold:
1) Reducing triggers
2) Eliminating intestinal permeability
3) Providing the body with nutrients to regenerate
Identifying and eliminating triggers and toxins will likely take a few weeks to a few months. Providing the thyroid with the nutrition needed to help rebuild and detoxify will likely take three to six months.
Rebalancing the immune system by addressing the root cause of autoimmunity (intestinal permeability, gut dysbiosis, infections) may take one to three years, but in the meantime, we can modulate the immune system and throw our thyroid antibodies a decoy. Hope this helps!
https://thyroidpharmacist.com/articles/hashimotos-and-tpo-antibodies/
I’d like to add that it can be very expensive to test for antibodies! It cost me over $100 for each antibody test, which really shocked me considering my bill for other thyroid tests was under $50 total! For those of us on a budget and paying out of pocket (high deductible insurance!), it would be helpful to know how often is really necessary to have them tested, not just what is ideal. Unfortunately a lot of us can’t afford the ideal. Thanks for all you do to get this information out there, Izabella!
Joanna – you are very welcome! It’s always best to speak to your practitioner to evaluate your specific case, and whether you need more testing. I know from experience that sometimes it can be challenging to get your doctor to do comprehensive thyroid testing for you. Ulta Lab Tests is an amazing new resource where you can order your own blood tests, allowing you to really be your own advocate!
You will want to make sure you get all important thyroid panels such as TSH, Free T4, Free T3, TPO antibodies and TG antibodies, and much more—without a doctor’s order! Ulta Lab Tests offers blood tests and panels at a significant discount, and you can even submit the labs to most insurance companies for reimbursement.*
This option is also fantastic for people who do not have insurance or who have a high deductible plan. For more information, and my top recommended labs for thyroid disease, visit Ulta Lab Root Cause Thyroid Panel. https://www.ultalabtests.com/thyroidpharmacist/Item/Item/TP-Root-Cause-Thyroid-Panel-1
Hello
Is it strange to have TPO Antibodies going down but Thyroglobulin Antibodies going up?
TPO Antibodies
2/22/16-1993
11/7/16-900
3/27/17-809
Thyroglobulin Antibodies
2/22/16-33
11/7/16-35
Yiskah – thank you for following this page. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress.Every six weeks is usually a good schedule for testing your thyroid hormones. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Dr Izabella,
I’d like to thank you for very informative article. I have one question to you. My Thyroglobulin Antibodies were measured by Beckman Coulter Methodology (reference range 0.0-0.9 IU/mL) I am wondering if these results can be somehow comparable to the reference range you mentioned in the article?
Thanks.
Marzena – thank you for following this page. Different labs use different ranges based on environmental factors that can affect the local population and affect their ranges. I would advise you to ask your trusted clinician who’s care you are under. <3
Thank you for the article! It’s very informative but it doesn’t say how to impact antibodies level once they are high.
Elena – thank you for reaching out. IgG subclass antibodies have a half-life of 21 days, and stick around on immune cells for about two to three months. They need constant “reminders” in the form of an antigen so that their production continues. If the antigen is removed, the antibodies will go away as well. The time period required for them to completely forget about the antigen and disappear is nine to twelve months.
The following things need to be in place for the antibodies to forget about the thyroid:
1) The thyroid stops expressing TPO.
2) The thyroid cells are not damaged and able to regenerate.
3) There are no substances that look like TPO (glandulars, gluten, infections, other triggers).
4) The immune system is balanced.
5) The autoimmune cells are confused by a decoy.
Some of these requirements are quick and easy, and others will take some time …
The thyroid will stop expressing TPO for two reasons. One of them is thyroid destruction, which we do not want; the other is thyroid suppression. Thyroid suppression is induced by limiting iodine and taking a thyroid supplement to bring TSH to 1 mIU/L or so. This can take up to three months
In the case of autoimmune conditions, traditional and alternative medicine practitioners may focus on rebalancing the immune system (i.e. steroids and immune-modulating drugs used in traditional medicine, or else herbs, supplements, or acupuncture used in alternative medicine).
While this approach may be helpful for taming the immune system in the short term or overcoming autoimmune flares, it is often a temporary solution and the immune system may become imbalanced again once the medications, acupuncture, and herbs and supplements are stopped if the underlying issue that lead to the immune system imbalance is not addressed. Thus we can say that immune modulation treats only the symptoms, and not the root cause.
As we can’t change genes, our approach to addressing the root cause of Hashimoto’s is threefold:
1) Reducing triggers
2) Eliminating intestinal permeability
3) Providing the body with nutrients to regenerate
Identifying and eliminating triggers and toxins will likely take a few weeks to a few months. Providing the thyroid with the nutrition needed to help rebuild and detoxify will likely take three to six months.
Rebalancing the immune system by addressing the root cause of autoimmunity (intestinal permeability, gut dysbiosis, infections) may take one to three years, but in the meantime, we can modulate the immune system and throw our thyroid antibodies a decoy. Hope this helps!
ANTIBODIES
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
My lab (Kaiser) uses a different unit of measurement, Ng/dL. Do you have a reference chart for those units? In spite of physical symptoms over many years that have continued to worsen, Kaiser insists that my thyroid is perfect in every way.
Kim – thank you for reaching out. Different labs will have different ranges. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress.Every six weeks is usually a good schedule for testing your thyroid hormones.
Hi Izabella,
I haven’t officially been diagnosed with Hashimoto’s – my doctor didn’t even call me with my results even though my TPO was 590, probably because my TSH was 2.2. What I wanted to ask is do I have Hashimoto’s? This was my first antibodies test. A couple of years ago I was extremely tired and went for my first thyroid test and my TSH was 89. I managed naturally to bring it down to about 2.5 but they next year I had terrible anxiety which at the time I didn’t attribute to my thyroid but now I suspect it was. My TSH stayed around 2.5 but 6 months ago (last test since this latest one with TPO tested) it had spiked to 4.9 – which my doctor thought was fine even though the lab pointed out it was high. At that point I was starting to experience anxiety again after it had subsided for 5 months. To get to the point I don’t feel like I fit into any of the stages above, and since this is the first time I’ve had antibodies tested I guess I could’ve had them from the start. Is it possible to go in and out of hypothyroidism and not have Hashimoto’s?
Charlotte – thank you for following this page. I am sorry to hear you still trying to get a diagnosis. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress.Every six weeks is usually a good schedule for testing your thyroid hormones. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
I also highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms. Here are some links which might help:
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://www.thyroidpharmacistconsulting.com/clinician-database.html
MY RECENT CHALLENGES AND FINDING DR. RIGHT
https://thyroidpharmacist.com/articles/my-challenges-and-finding-dr-right/
Hi, I am so very grateful for you! What awesome information and links. Thank you so much for your passion to help others walking through this valley. I had TPOa reading of 252 at my highest. I started taking selenium with Inositol and 1 drop of Iodine. I didn’t check my thyroid numbers a month and a half later, but I did have my TPO antibodies checked. They had dropped down to 167. That was November 2017. I received my blood tests results yesterday and my TSH went from 2.98 to 8.01. My TPOa was 462. I was so floored! I was taking all kinds of supplements, including
“Restore” and George’s Aloe for my leaky gut. I don’t do gluten, dairy, sugar etc. I was so disheartened by this. After reading some of your material about iodine, I am totally stopping it. I feel the same as I have always felt, no worse. So, my boiled-down question is this – why did my TPO antibodies go to the moon in about 6 months? Dr. Brownstein says in his books about Iodine and Thyroid that TSH will go up but should go back down once the body gets used to having iodine. I don’t recall anything said about TPOa. Thank you for any information about this. God bless!
Peggy – thank you for sharing your journey! I am very hesitant in recommending iodine in Hashimoto’s. Although iodine serves as fuel for our thyroid and is very important in iodine deficiency hypothyroidism, Hashimoto’s is a different mechanism. It’s like pouring gas into an engine that’s on fire… that’s essentially what’s happening in Hashi’s, thyroid inflammation. Adding iodine to the mix before putting out the fire and fixing the engine may result in further damage to the thyroid. In those with a predisposition to autoimmunity, this has been documented time and time again, in animal and human studies.
I have spent 4 years researching about this issue, and have seen too many people suffering the consequences of adding iodine too soon. My approach is, let’s fix the engine first (usually a gut issue), and then add the fuel once we know that the engine is no longer on fire. Hope that you will check out my books. I do have a chapter on the iodine controversy that references numerous studies as well as the work of Abraham and Brownstein. Here are the links to my books:
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
I so appreciate your response! I purchased the Hashimoto’s program you offer and I am very happy I did!! It has so much incredible information in it and I am grateful for your passion to help others. Thank you a gazillion! God bless!! Peggy
Peggy – you are very welcome! I appreciate your kind words and support! I hope you keep me posted on your progress. <3
Dr Izabella,
Do you know if any info regarding a connection between hashimoto’s and chronic urticaria?
Jennifer – thank you for reaching out. Our skin is a window to our internal health. It is the body’s largest elimination organ, and also a canvas where toxicities, nutrient deficiencies, food sensitivities and hormonal imbalances can show up. Women with Hashimoto’s and autoimmune conditions are more likely to have dry, dull skin, rashes, hives, pre-menstrual acne and facial swelling, especially if their thyroid levels are not optimized and they are not absorbing vitamins and nutrients correctly. Here is an article which you may find helpful.
THE COMMON ROOT CAUSE OF HASHIMOTOS HIVES AND IBS
https://thyroidpharmacist.com/articles/the-common-root-cause-of-hashimotos-hives-and-ibs/
I would like to thank all the help provided to the community.
Is Propolis Extract Beneficial for Hashimoto?
Mike – thank you so much! I wish I could give you more direct advice but, each person will react differently. I would advise you to ask your personal clinician who’s care you are under.
I’m going in for an appointment with a new endocrinologist this week and I am taking my results showing my antibodies just under 6000, are there specific questions I should be asking. The last endocrinologist at this office told me antibodies mean nothing/don’t matter. I want to be direct with the new one I am seeing but obviously respectful.
Rebecca – thank you for reaching out. I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Here are some articles you might find helpful.
10 THINGS I WISH MY ENDOCRINOLOGIST WOULD HAVE TOLD ME
https://thyroidpharmacist.com/articles/10-things-i-wish-my-endocrinologist-would-have-told-me/
THE BEST KIND OF DOCTOR FOR HASHIMOTO’S
https://thyroidpharmacist.com/articles/what-type-of-doctor-should-you-see-if-you-have-hashimotos/
HOW TO DIAGNOSE HASHIMOTO’S
https://thyroidpharmacist.com/articles/4-steps-to-diagnose-hashimotos-and-monitor-treatment/
Your site is great and with so much information! I was told I had Hashimoto’s about a year ago, with no need yet to treat. At my last test 6 months ago I had thyroid antibiodies of 457 and a TSH of 3.58. I go in for another check soon. While everything I see here says I’m in early stages I have many symptoms including a significant loss of hair. My doctor didn’t want to start me on any medications because she said once I start I’d be on them for life. She put me on iron and b12 supplements because I was really low in those areas as well. The iron has helped slow down the hair loss but not stopped it yet. What should I do? Keep waiting until my numbers get worse or ask her to start me on some thyroid medication to control my symptoms? This is just my general practitioner. Should I ask her about seeing specialist? I don’t want to upset her if she finds out I went somewhere else for thyroid treatment next time I go see her for my normal care.
Stephanie – thank you for reaching out. It took me three years to get into remission, but every change can bring huge benefits. There are 5 stages to thyroid disease. A conventional doctor won’t look at stopping the autoimmune attack progressing. What we usually see is that a person with only thyroid antibodies and normal TSH is considered to be in Stage 2 of thyroid disease, a person who has an elevated TSH with normal T4/T3 with or without thyroid antibodies, is in Stage 3 of thyroid disease, a person with elevated TSH, lowered T3/T4 +/- thyroid antibodies is in Stage 4 of thyroid disease, regardless if she/he has thyroid antibodies or not. Stage 5, is when the person progresses to other types of autoimmune disease. Functional medicine doctors really aim to find and treat underlying causes and prevent serious chronic disease rather merely treat disease symptoms.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid/
10 THINGS I WISH MY ENDOCRINOLOGIST WOULD HAVE TOLD ME
https://thyroidpharmacist.com/articles/10-things-i-wish-my-endocrinologist-would-have-told-me/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
You may also like to check out the doctors that other patients recommend on this list:
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
I beginning to think that a diagnosis of hypothyroidism or Hashimoto’s disease are based on guesswork alone. My Free Thyroxine (1.17 to 1.22), TSH (1.1 to 3.4) and TPO results (only one time but a mere 9 IU/ml) seem perfectly normal, yet I’m on levothyroxine and have both “hypothyroidism” and “Hashimoto’s thyroiditis” on my patient record. While it is true that both my sister and my mother have “thyroid” problems (my sister had hers surgically removed), the odds are against it for me: I’m male, I have an issue with CIU that makes hypothyroidism a handy diagnosis, and as stated above, the numbers just don’t bear it out. I appreciate the article above, but it just convinces me even further that hypothyroidism is a blanket –and sometimes convenient–diagnosis.
Garth – thank you for reaching out and sharing. Thyroid hormones can fluctuate from normal to outside of range back and forth for years which is why symptoms must also be taken into account. Some people with Hashimoto’s test negative for thyroid antibodies because their overall immune health is so weak they do not produce enough antibodies. I’ve tested negative for antibodies several times. Now I’ve insisted on a thyroid ultrasound. Given that Hashimoto’s is one of the leading causes of hypothyroidism worldwide, I wouldn’t stop until I know one way or another. Family history is a very good indicator that thyroid disease is likely. Here are some articles you might find interesting.
IS HASHIMOTO’S HYPOTHYROIDISM GENETIC?
https://thyroidpharmacist.com/articles/is-hashimotos-genetic
THYROID DISEASE IN MEN
https://thyroidpharmacist.com/articles/thyroid-disease-in-men/
My TPO Ab Test came back as 10 UI/mL. Would that be considered normal?
Patricia – thank you for reaching out. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Dear Dr. Wentz,
After reading this article I am more convinced now, than ever, that I have have Hashimoto’s disease. I just want to clarify one thing. My TPO came back at 31, my TSH was 264.43. This is not a typo, nor do I assume that the lab made a mistake. If I understand what you are saying, even if the TPO is in the “normal” range, but because I present all of the symptoms, I have Hashimoto’s? I have been dealing with this now for about 20 years, most likely longer, and I can’t seem to find any answers and lately no doctor wants to even discuss it with me. I finally resorted to seeing a Naturopath who suspects, and I do as well, that I have multiple food sensitivities including gluten for starters. We both think that if I can get my diet on track and get rid of the foods that are making me ill, that over time my symptoms will improve or go away. I get sick a lot as well. I’m just wondering what your thoughts on this would be. Thank you in advance for your time.
Wendy – thank you for reaching out. I am happy to hear you have found a practitioner and are taking charge of your health. The gold standard or the most accurate test for uncovering reactive foods and individual food sensitivities is actually the elimination diet. In contrast to other diets that simply exclude common problematic foods, an elimination diet is done to determine what particular food intolerances the individual may have. An elimination period of at least 2-3 months is a good starting place, but you may want to continue if you feel that you still have more healing to do. Then you can try a new food every 4 days and monitor yourself for reactions. Going through an elimination diet will help you figure out your own individual food triggers and your specific response to each trigger food. Here is an article I hope you find interesting!
https://thyroidpharmacist.com/articles/elimination-diet-for-hashimotos
My TPO is 14. I’m having trouble getting pregnant and miscarrying is an issue. Every panel of everything else we run is normal. A thermography scan done showed inflammation and the technician said this is often a sign of Hashimoto. So I did a full T4 panel and it’s normal. Is it possible this is early stages and why I can’t get pregnant? The Fertility clinic has had me on synthroid for 2 years to keep my T3 number between 1 and under 2. Any suggestions?
Ginger – thank you so much for sharing your journey. I am so sorry to hear you are struggling with all of this. I understand how hard it is. <3 There are 5 stages to thyroid disease. A conventional doctor won't look at stopping the autoimmune attack progressing. What we usually see is that a person with only thyroid antibodies and normal TSH is considered to be in Stage 2 of thyroid disease, a person who has an elevated TSH with normal T4/T3 with or without thyroid antibodies, is in Stage 3 of thyroid disease, a person with elevated TSH, lowered T3/T4 +/- thyroid antibodies is in Stage 4 of thyroid disease, regardless if she/he has thyroid antibodies or not. Stage 5, is when the person progresses to other types of autoimmune disease. Functional medicine doctors really aim to find and treat underlying causes and prevent serious chronic disease rather merely treat disease symptoms. Here are some resources you might find helpful:
THE 5 STAGES OF HASHIMOTO'S THYROIDITIS
https://thyroidpharmacist.com/articles/5-stages-hashimotos-thyroiditis/
10 THINGS I WISH MY ENDOCRINOLOGIST WOULD HAVE TOLD ME
https://thyroidpharmacist.com/articles/10-things-i-wish-my-endocrinologist-would-have-told-me/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
You may also like to check out the doctors that other patients recommend on this list:
CLINICIAN DATABASE
http://www.thyroidpharmacistconsulting.com/clinician-database.html
Hello, I have been fighting with thyroid symptoms for most of my life. My tpo is 18.2 all other thyroid tests are normal. My doctor wants me to get all this allergy testing done with a company that does not take Insurance. I have been having increased allergic reactions to things examples vitamins, makeup, shampoos., conditioner, lotion, body washes. I had a massive reaction to my vape a butterfly rash all over my neck. All I can trace it to is vegetable glycerin allergy. Through the years my reactions seem to be getting worse. I get hives all the time for no apparent reason.
Jessica – thank you for reaching out. I am so sorry you are struggling with all of this. I’ve found that many Hashimoto’s patients also have the gut infection Blastocystis hominis, which has recently been connected to irritable bowel syndrome, hives AND Hashimoto’s. In the last few years, I’ve noticed that getting rid of the Blastocystis hominis infection can help people to get their Hashimoto’s into remission. Read more about it in my Blastocystis article:
A COMMON ROOT CAUSE OF HASHIMOTO’S, HIVES AND IBS
https://thyroidpharmacist.com/articles/the-common-root-cause-of-hashimotos-hives-and-ibs
THE THYROID AND SKIN
https://thyroidpharmacist.com/articles/the-thyroid-and-skin
Hi. A blood test I had a while back came through normal. However, it wasn’t till recently that in reviewing my test, my doctor noted an unusually high anti-TPO reading. She tried to find some literature on it, but the only thing she came across appeared to be inconclusive as to what it means. Anyway, she didn’t seem too concerned about it, but she definitely wanted to keep track of this with the next blood test I’m due for. Basically, the reading I got was:
Anti-TPO 129.3 IU/ml with a Reference Value of 0.00-9.00. It came with an Abnormal Flag of High and a Result Status of F (but the F referred to Final, I believe, if I recall correctly, and not Fail, as I originally thought).
Now, if the Reference Value, or normal reading, is between 0.00-9.00 and I got a reading of 129.3, shouldn’t I be dead by now? It was the same joke I used on my doctor and she said no, because clearly I was still alive. So, out of curiosity, I thought I’d see if I could find something about this on the net and came across this site as the first result. It should be noted, that a few years ago during an examination I was found to have “shoddy lymph nodes” in my upper left thigh, but the the doctor then, a urologist, wasn’t too concerned about it. As well, I was diagnosed with Parkinson’s just over two years ago, but this is now being re-evaluated as some things don’t seem to be fully adding up to that diagnosis. Other than that, I don’t feel like I’m anywhere near death’s door, although shedding some light on this apparently ultra-high anti-TPO reading and what it would might mean would most certainly be greatly appreciated and maybe something I could bring to the attention of my doctor for her to investigate further. Thanks in advance.
Walter – thank you for reaching out. About 95% of people with Hashimoto’s have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body’s response. Some people with Hashimoto’s test negative for thyroid antibodies because their overall immune health is so weak, they do not produce enough antibodies. I tested negative for antibodies several times. Now, I insist on a thyroid ultrasound. A thyroid ultrasound can be used to detect changes in the thyroid, associated with Hashimoto’s. Given that Hashimoto’s is one of the leading causes of hypothyroidism worldwide, it’s best to be certain, one way or another.
Here are some articles I think you might find helpful:
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
Thank you a million times over, for this amazing library of information. I stay up into the wee hours of the night, reading everything.
Antibody +Iodine question: I started taking a multi vitamin (Pure Encapsulations 950), about 2 months ago. I didn’t realize until a few days ago (reading ingredient list closer), that the formula included iodine (100 mcg).
My Thyroid Peroxidase antibodies, jumped from 606 IU/ml (test date of Oct 2018), to 743 IU. (test date of Jan 2019) .
Strangely, my Thyroid Globulin Antibodies, decreased slightly, during this same period of time. From 14 IU/mL, to 10 IU/mL.
Have you ever seen these thyroid antibodies, fluctuate like this? Is it possible that the iodine in the supplement, is affecting the TPO ab level? I have eliminated all other sources of iodine (eg, seaweed, kelp salads, iodized salt, etc.).
Thank you for your thoughts.
Mack – thank you for sharing. <3 I am very hesitant in recommending iodine in Hashimoto's. Although iodine serves as fuel for our thyroid and is very important in iodine deficiency hypothyroidism, Hashimoto's is a different mechanism. It's like pouring gas into an engine that's on fire... that's essentially what's happening in Hashi's, thyroid inflammation. Adding iodine to the mix before putting out the fire and fixing the engine may result in further damage to the thyroid. In those with a predisposition to autoimmunity, this has been documented time and time again, in animal and human studies.
I have spent 4 years researching about this issue, and have seen too many people suffering the consequences of adding iodine too soon. My approach is, let's fix the engine first (usually a gut issue), and then add the fuel once we know that the engine is no longer on fire. Hope that you will check out my books. I do have a chapter on the iodine controversy that references numerous studies as well as the work of Abraham and Brownstein. Here are the links to my books :
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
Dr. Izabella,
It was discovered that I had Hashimoto’s in November 2017. The official diagnosis came in January 2018 when I went to an Endocrinologist. Because I had to wait for a month to get an appointment, I searched online for possible natural remedies and came across your site along with Dr. Amy Myers. Leading up to that appointment, I ate strict AIP for the month and to the dismay of the physician, when my blood was tested again in January 2018, the Hashimoto’s had been completely reversed and the results were in normal range. The past year has been a delicate dance with food to find the specific items that cause inflammation and need to be eliminated permanently and those I can have occasionally, etc.
My thyroid antibodies have been tested every 6 months by my gynecologist, which brings me to my question. Before this week, all of my previous blood tests have been done at my gynecologist’s office. He checks my TPO and TG levels. This week, he provided me with an order to have the blood drawn at my place of employment to save time but the results are listed differently and I wondered if you might be able to explain why. In July 2018 my TPO level was 39 IU/mL (range 0-34), which was slightly elevated and the TG was less than 1 IU/mL.
My current results are listed at Thyroid Peroxidase Antibodies – 2 and have a range of 0-9 IU/mL and they apparently did not test for TG because it was not even on the paper. This is the 4th time my thyroid antibodies have been checked and I have never seen a TPO range of 0-9 and wonder if this is the same test I have had in the past or if it is different somehow. Are there multiple tests for TPO that would render different results?
Thank you.
Lesa – thank you so much for reaching out and sharing your journey. I am so proud of you for taking charge of your health! <3 Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. It's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. I recommend these thyroid function tests:
¨ TSH
¨ TPO Antibodies
¨ Thyroglobulin Antibodies
¨ Free T4
¨ Free T3
¨ Reverse T3 (optional)
¨ Thyroid Ultrasound (optional)
Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
While I have my TSH, Free T3, and Free T4 checked each time I test for the antibodies, I am specifically curious about the test for TPO. Are there 2 different tests for TPO antibodies that render different results? The first 3 tests had a range of (0-34 IU/mL) and the 4th test’s range was (0-9 IU/mL). Why do I have different ranges on my results? Is one more precise than the other?
Lesa
Lesa – thank you for reaching out. About 95% of people with Hashimoto’s have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body’s response.
Some people with Hashimoto’s test negative for thyroid antibodies because their overall immune health is so weak, they do not produce enough antibodies. Dr. Wentz has tested negative for antibodies several times. Now, she insists on a thyroid ultrasound. A thyroid ultrasound can be used to detect changes in the thyroid, associated with Hashimoto’s. Given that Hashimoto’s is one of the leading causes of hypothyroidism worldwide, it’s best to be certain, one way or another.
Here are some articles I think you might find helpful:
TOP THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests
HASHIMOTO’S AND TPO ANTIBODIES
https://thyroidpharmacist.com/articles/hashimotos-and-tpo-antibodies/
Best article ever.. and part 2 is awesome as well. Thank you so much for what you do for the community of people who have this disease.
Now if we could only get more doctors on board….
Peace and love to you.
Tara – thank you so much for your support! I agree!
Hi Dr. Isabella, Thank you so much for this article! This helps me understand my test results:
December TSH 2.1, TPO 280.
March TSH 2.2, TPO 365.
Despite 3 months of eating completely AIP, my TPO is still rising! I also most days feel symptoms of hypothyroidism (every once in a while a hyper swing), so I am probably in stage 2 of developing Hashis.
What do you recommend doing when you catch it at stage 2?? What else can I do besides the AIP diet to reverse this shit?!? Help!!!
Hannah – thank you for reaching out and sharing your journey. <3 I understand how frustrating this can be. Did you know that if you live in the United States, Australia, Europe and most developed countries that add iodine to the salt supply and take thyroid medications, there’s a higher probability that you do have Hashimoto’s?
Depending on the source, estimates are that between 90-95% of those with hypothyroidism have Hashimoto’s.
But most doctors will never tell people that they have Hashimoto’s, or that their own immune system is attacking their thyroid. People are told that their “thyroid is sluggish,” and that these things happen with age and “Just take this pill, you’ll be fine.” I hope you check out these articles that I wrote.
5 Stages of Hashimoto's
https://thyroidpharmacist.com/articles/5-stages-hashimotos-thyroiditis/
ARE YOU DOING EVERYTHING FOR YOUR THYROID BUT NOT YET WELL?
https://thyroidpharmacist.com/articles/are-you-doing-everything-for-your-thyroid-but-not-yet-well/
DO YOU HAVE HYPOTHYROIDISM OR HASHIMOTO'S OR BOTH?
https://thyroidpharmacist.com/articles/do-you-have-hypothyroidism-or-hashimotos-or-both/
Hi. Your site has been a huge help and resource for information. I was recently told I have Hashimoto’s by my doctor after discovering it through routine bloodwork. I’m waiting to see an endocrinologist for more possible tests but can’t get in for over a month. My TSH is 8.12, T4 is .75, T3 is 3.3 but antibodies are high: anti-TPO 197 and thyroglobulin 22.7. But I don’t feel bad. I am not overly tired/fatigued, plenty of energy, no horrible brain fog, actually losing weight. My only symptoms would be cold sensitivity, some joint pain and I’ve noticed my skin and hair to be more dry. But it’s also winter! Or maybe I just think this is my “normal.” 🙂 My doctor prescribed 50 mcg Levothyroxine but I haven’t taken yet. My question is whether I’m full blown hypo yet and should be on medication or am I in the early stages/subclinical enough to where maybe with diet and supplements I can get it under control? I’m afraid to take medicine that I don’t necessarily need. But also afraid of not taking it and having more damage done. I get an ultrasound of my thyroid this week. I thought my antibodies seemed very high but reading the above referencing numbers in the thousands I’m now questioning whether I’m full blown or not.
Jessica – thank you for reaching out and sharing your journey. <3 Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. Here are some research articles which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
THE 5 STAGES OF HASHIMOTO'S THYROIDITIS
https://thyroidpharmacist.com/articles/5-stages-hashimotos-thyroiditis/
Should I be concerned????
My TSH is 11.3 mIU/L, T4 is 13, pmol/L and T3 is 11.4 pmol/L
My GP has said there is nothing to be concerned about since I am 65 and there were no previous signs of thyroid issues over the past 10 years. I am tired and fatigued, I have also lost my eyebrows as well. Also my antibody testing is in the normal range.
DD
Deborah – thank you so much for reaching out and sharing. I am so sorry you are struggling. <3 Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
I just had a TPO test and the results are given in WHO Units (not iu). Is there a way to convert this to iu? Or is there an optimal range somewhere? I’m told I’m in the normal range, but just want to be sure I’m also in the “optimal” range. Thanks!
Jen – thank you for reaching out. I understand how frustrating this can be. Different labs will have different ranges. Here is a link to a free downloadable e-book that will help you understand your thyroid lab results and how to optimize your thyroid hormones.
https://thyroidpharmacist.com/checkout/?product_id=4702
Hello. I am 27 yrs old and my thyroid is enlarged. I recently had labs done through my Endocrinologist. My T4 Total was 10.2, My Thyroid Peroxidase Antibodies was 584. Graves Disease does run in my family. Also I do have alot of the symptoms for Hashimotos. Should I be concerned. My doctor said that my labs were normal and is not wanting to prescribe me medications.
Adrienne – thank you for reaching out and sharing your journey. <3 Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
After 12 years of Hashimoto’s and psoriasis, I’m fed up with my treatment and I’m searching for answers. My TSH is normal on levothyroxine, but I still have hair loss and some brain fog. So glad to find your website! Scary, though — I just looked back at my initial diagnosis from 2006 and my TPO was >6500!!! My doctor only has ever tested TSH since then. I’m going to get a TPO test today and will test my antibodies again in 3 months after trying the AIP diet. Thanks for all the great info.
Jenna – thank you for following this page. I am so proud of you for taking charge of your health! I hope you will keep me posted on your progress. Here is an article you might find helpful when you received your lab results.
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Hello,
I am a 54 years old male with the following results after a doctor’s visit during which my doctor detected something in my neck.
Tg Ab = 315 lU/ml (High)
TPO= 5.6 lU/ml
TSH= 3.1 ulU/ml
Free T4= .86 ng/dl
I see a lot of comments and results from others about high TPO in this website, but not about Tg Ab being high, and in my case, that seems to be the case. Also, is being a male a factor to anything?
They are describing it as a “nontoxic” goiter. What does that mean?
Thank you.
A.R. – thank you for reaching out. About 95% of people with Hashimoto’s have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body’s response. Here are some articles I think you might find helpful:
HASHIMOTO’S AND TPO ANTIBODIES
https://thyroidpharmacist.com/articles/hashimotos-and-tpo-antibodies
HASHIMOTO’S AND THYROID ANTIBODIES: PART 1
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
Thank you for an informative article. I have been on a three year journey where I had cancer (not thyroid related), followed by ongoing higher than normal thyroid antibodies but normal readings for T3 and T4 hormones. My GP convinced me I was depressed and refused a referral to an endocrine. My GP told me that I would have to wait ten years on observation before she would consider thyroxine and further assistance.
I have been facing ten years in my thirties with weight gain, fatigue, hair loss, temperature sensitivity and a bloated face. My GP also put me on diet pills and told me to eat less – when my diet is 1500 calores a day with no sugar, alcohol or processed foods.
I have a very strong family history of thyroid cancer and hashimotos on both sides of my family. Only after seeing a combined fertility and endocrine specialist, that I was told I should have been on thyroxine years ago – and would have to be on thyroxine prior to IVF. The relief I felt all at once was wonderful – and it was soon followed by frustration.
I am extremely angry that from the age of 32-35 I allowed myself to be shamed by a GP and allowed myself to be convinced that my weight gain and symptoms were my own fault through diet and lifestyle – which is simply not the case when I went through gruelling exercise regimes with personal training twice a week, walking 5 kms a day and spin classes and weight training three times a week, food restrictions and ultimately a poor quality of life (I went from being a fit and bubbly person to refusing to have my photo taken on holidays and spending my time panicking over food choices in the supermarket, and memorising countless food item calories). This is on top of trying to live a life free of cancer and keep it all together.
You are absolutely right that the medical community has a LONG way to come.
Thank you for shining a light on this. It makes another isolated person feel much better.
MJ – awe… I am so sorry you have had to go through all of this. <3 My heart goes out to you. I am happy to hear you are taking charge of your health and have found a practitioner. A couple of years after my diagnosis, I found Hashimoto’s 411, a closed Facebook group run by Alice Berry McDonnell. This group is amazing! It is comprised of an army of highly motivated, smart, supportive women and men (now 45,000+ strong), and each of them sharing ideas of what worked for them, things they were planning to try, and offering support to one another. The comfort I received from knowing that there were others going through the same challenges as I, was enormous.
https://www.facebook.com/groups/hashimotos411/
Hello i just got my bloodwork back and had Thyroid peroxidase Antiobodies 231 H all other tests TSH, T4, T4 FREE, T3 FREE, T3 Total in normal limits. My doctor put me on LEVOTHYROXINE 25 mcg i told him had extreme fatigue, hair loss, weight gain. I also have UVEITIS inflammation of the eye. My family doctor referred me to Rheumatologist which i have not seen till next month. Should i ask for a specialist to take over to review my meds and labwork for my thyroid. My dad has Hashimotos (cancer in thyroid had it removed) sister diagnosed with Graves Disease. I have started medication LEVO 3 weeks ago feel worse so far should i even be on the medication yet the general doctor started me on the medication. I have been having numbness in my body, pain and aches in joints, anxiety, feeling of head fullness, feeling faint at times. My body is suffering right now im trying to hold up hard being a mom of autistic boys and wife want to be here for the longrun for them i love life just hate suffering but i know im not alone! Just any suggestions advice wanted thank you.
Melinda – thank you for sharing your journey with me. I am so sorry you are struggling. I do understand how hard and overwhelming it can be. Hashimoto’s is often a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better.
Hashimoto’s is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission.
You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto’s. Once you do, you will know what types of changes you need to implement to make yourself feel better.
If you need further support, please check out the list of lab tests inside the “Testing” chapter of my book, Hashimoto’s Root Cause. I also offer a 12-week program, Hashimoto’s Self Management Program. Here are some resources I hope you find helpful as well.
BUILDING YOUR OWN HEALTH TIMELINE
https://thyroidpharmacist.com/sample-health-timeline/
Hashimoto’s Self-Management Program
https://thyroidpharmacist.com/enroll-in-hashimotos-self-management/
Hello Doctor, I have been suffering from fatigue , hair loss, memory loss, difficulty concentration, muscle and joint pain since I gave birth 3 years ago. I have always had TPO antibodies elevated since I was young. My mother had to have her thyroid removed because she had a lot of benign nodules. My sister had thyroid cancer. I suffered from thyroiditis postpartum but my thyroid levels went back to normal after a year. I get labs done every 6 months. My last labs came up normal, only TPO 122 but I have a lot of symptoms like extreme fatigue, exercise intolerance, depression and anxiety. My doctor ordered an ultrasound and in the ultrasound they say they could see I have hashimotos. Apparently my thyroid didn’t look enlarged ( in a previous ultrasound last year I was told my thyroid was enlarged) and didn’t have nodules but she said I have hashimotos because of the cells characteristics that she saw in the ultrasound. I also have mild vit D deficiency 29 ng/ ml . She says there is nothing they can do now, and I should retest in a year. What do you think? is it possible to see in the ultrasound that I have hashimotos ? Thank you !
Rebecca – thank you for reaching out and sharing your journey. <3 About 95% of people with Hashimoto's have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body's response.
Some people with Hashimoto’s test negative for thyroid antibodies because their overall immune health is so weak, they do not produce enough antibodies. I tested negative for antibodies several times. Now, I insist on a thyroid ultrasound. A thyroid ultrasound can be used to detect changes in the thyroid, associated with Hashimoto's. I recommend getting an ultrasound done at least once every 1 to 5 years, if everything looks normal. If you have nodules, you may want to do that more often—once every two years. I have written several articles about how to best decrease thyroid antibodies.
Here are some articles I think you might find helpful:
HASHIMOTO'S AND THYROID ANTIBODIES: PART 1
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
back in 2017 I did a full blood panel and got this result
Component Your Value Standard Range
THYROGLOBULIN AB 63.3 IU/mL 0.0 – 0.9 IU/mL
I was told I have a nodule in my thyroid and did a sonogram to view it.
and then nothing.
are these levels something I should be worried about?
Natali – thank you for reaching out. <3 About 95% of people with Hashimoto's have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body's response.
Some people with Hashimoto’s test negative for thyroid antibodies because their overall immune health is so weak, they do not produce enough antibodies. I tested negative for antibodies several times. Now, I insist on a thyroid ultrasound. A thyroid ultrasound can be used to detect changes in the thyroid, associated with Hashimoto's. Given that Hashimoto’s is one of the leading causes of hypothyroidism worldwide, it's best to be certain, one way or another. Nodules and goiters are often the result of toxicity and/or the autoimmune process. So, doing interventions to reduce the autoimmune attack on the thyroid, and toxicity, can be helpful to reduce them.
Here are some articles I think you might find helpful:
THYROID NODULES
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-nodules/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 1
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
Hi Dr. Wentz,
I have been reading your blog here and I appreciate you taking the time in your busy schedule to help people with thyroid issues and concerns. My recent lab test results are as follows:
TSH: 8.4
T4: 1.29
TPO: <6 (standard range: 0 – 34)
I currently don't seem to have any symptoms. What are your recommendations for someone like me?
Thanks again,
Michelle
Michelle – thank you for reaching out and sharing. <3 Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. There are 5 stages to thyroid disease. A conventional doctor won't look at stopping the autoimmune attack progressing. What we usually see is that a person with only thyroid antibodies and normal TSH is considered to be in Stage 2 of thyroid disease, a person who has an elevated TSH with normal T4/T3 with or without thyroid antibodies, is in Stage 3 of thyroid disease, a person with elevated TSH, lowered T3/T4 +/- thyroid antibodies is in Stage 4 of thyroid disease, regardless if she/he has thyroid antibodies or not. Stage 5, is when the person progresses to other types of autoimmune disease. Functional medicine doctors really aim to find and treat underlying causes and prevent serious chronic disease rather merely treat disease symptoms. Here are some articles I hope will help.
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
5 STAGES OF HASHIMOTO’S THYROIDITIS
https://thyroidpharmacist.com/articles/5-stages-hashimotos-thyroiditis/
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid/
Hello. This is a great resource and guide!!! Do you have something similar on Graves’Disease? I was diagnosed 9 months ago and my levels aren’t leveling consistently. Infact I’ve only been in normal FT4 and FT3 range for 2 months.
Katie – thank you for reaching out. <3 I understand how hard this can be. My protocols are designed to help those with thyroid autoimmune disease heal by focusing on gut health, nutrient deficiencies, and root cause discovery and treatment. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Hashimoto’s is a complicated condition with many layers that need to be unraveled. While conventional medicine only looks at each body system as a separate category and is only concerned with the thyroid’s ability to produce thyroid hormone, Hashimoto’s is more than just hypothyroidism, it's an autoimmune disease that needs to be managed. Whether you have all, part or no thyroid, the autoimmunity still persists in most cases. We need to re-balance the immune system which begins in the gut. With the exception of discussing proper thyroid medication dosing, the majority of my website and book's focuses on balancing the immune system. The info I present is based on my own research and journey overcoming my autoimmune thyroid condition. If you have any questions about my protocols you are welcome to email my team at info@thyroidpharmacist.com and they will be happy to help as well.
Here are some articles I think you might find helpful:
IMPORTANCE OF GUT HEALTH
https://thyroidpharmacist.com/articles/importance-gut-health/
WHERE DO I START WITH HASHIMOTO’S
https://thyroidpharmacist.com/articles/where-do-i-start-with-hashimotos/
I was diagnosed march 2017 with Hoshimotos. But for the past 9 months I have been loosing handfulls of hair and also excessive amount of weight (10-15lbs) in 1 maybe two months. I can’t gain weight and when I do finally gain I loose it right away and it can be up to 5 and at times 10lbs in just a few days. I asked my doctor to do the following tests because I don’t feel right and my body feels as if I just cant do anything. I asked for TSH and it was 2.410 uIU/ml , T3 Total it was 134ng/dl, T4 free it was 1.68ng/dl, TPO antibody it was 208 IU/ml. My doctor wrote that, Thyroid funtion is normal, you have antibodies to thyroid that can be seen in Hashimotos (underactive thyroid) and Graves (overactive thyroid)… No treatment needed as of yet.
To me that should be enough proof that treatment should start and it’s not the 1st time my antibodies were high and I am not well as well as having trouble swalloing and my thyroid is swollen (goiter). My mom and her identical twin had their thyroids removed at 16yrs old as did her 2 brothers. My sister was diagnosed with Hashimotos 5 years ago and on medication. I also have many other health issues and was diagnosed 15yrs ago with autoimmune disease. What would your advise be regarding my levels and should I request other testing?
Thank you so much!!
Cheryl Kump
Cheryl, thank you so much for sharing your journey. I’m so sorry you are struggling with all of this. I understand how frustrating it can be. There are 5 stages to thyroid disease. A conventional doctor won’t look at stopping the autoimmune attack progressing. What we usually see is that a person with only thyroid antibodies and normal TSH is considered to be in Stage 2 of thyroid disease, a person who has an elevated TSH with normal T4/T3 with or without thyroid antibodies, is in Stage 3 of thyroid disease, a person with elevated TSH, lowered T3/T4 +/- thyroid antibodies is in Stage 4 of thyroid disease, regardless if she/he has thyroid antibodies or not. Stage 5, is when the person progresses to other types of autoimmune disease. Functional medicine doctors really aim to find and treat underlying causes and prevent serious chronic disease rather merely treat disease symptoms.
I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid/
10 THINGS I WISH MY ENDOCRINOLOGIST WOULD HAVE TOLD ME
https://thyroidpharmacist.com/articles/10-things-i-wish-my-endocrinologist-would-have-told-me/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
You may also like to check out the doctors that other patients recommend on this list:
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
Sorry to bother you. I tried asking my doctor what thus means and she really didn’t give me a answer other than don’t worry about that. I ache all over and I dread waking up as my whole body hurts. Nobody believes me. I’m getting annoyed getting no answers. In December this number was 1542. I’m not understanding what it means. I’m at my wits end.
Thyroid peroxidase antibody
Your Value
3,782 IU/mL
Standard Range
<6 IU/mL
Flag
H
Casey – thank you for reaching out. I’m so sorry you are struggling and not feeling well. My heart goes out to you. <3 About 95% of people with Hashimoto's have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body's response.
Some people with Hashimoto’s test negative for thyroid antibodies because their overall immune health is so weak, they do not produce enough antibodies. I tested negative for antibodies several times. Now, I insist on a thyroid ultrasound. A thyroid ultrasound can be used to detect changes in the thyroid, associated with Hashimoto's. Given that Hashimoto’s is one of the leading causes of hypothyroidism worldwide, it's best to be certain, one way or another. Here are a couple articles you might find helpful:
HASHIMOTO'S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Hi Dr.Izabella
sorry for bothering but i have question regarding my thyroid function tests that i did it in june 11,2020 my tsh was <0.01 normal .32-4.00
and my free t4 was 19 normal 9-19
,my TPO was <9 normal < 35 i am f ,40 years i am always tired ,gain weight fast 10 kg in 3 months start to have belly fat although i have 2 kids with cesarean section delivery and did not have belly fat before. have joint pain start after gain weight ,memory is not good and has hair loss .what is your recommendation about my case what i am suffering from?
thanks alot.
Emi – thank you for reaching out and sharing. <3 I understand how hard this all is. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Hi Dr. Wentz! Thank you so much for this incredible article. I just got my blood test results because I had a feeling I may be leaning towards hypothyroidism. My mother has had it for years. Should I have fasted for the test? I had eaten that day, and wondered if this affected the results, but anyway here they are.
My TSH was 6.7!!
I had blood work done 1 year and half ago and it was 3.9. I was shocked to read that.
But then I noticed they checked my Thyroid Peroxidase was 13,000!!!! What in the world?! This has given me anxiety all day long and I’ve been researching like crazy!
My T3 and T4 were both in normal ranges.
What does this mean and am I dying?? I will see my primary doctor on Monday, I feel so anxious.
Amelia – thank you so much for sharing your journey. I do recommend that you discuss your results and questions with your practitioner who’s familiar with your health history. Here are some articles that you may find helpful as well:
HASHIMOTO’S AND THYROID ANTIBODIES: PART 1
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
I really need some help. 7 years ago I had a TPO test through LabCorp while seeing a functional medicine doctor. My level was 2534. I’ve recently been changing diet, lifestyle and incorporating supplements to reduce my antibodies. But I cannot find a lab that will give a TPO with a specific number if it is greater than a certain amount. Labcorp is now greater than 600, Quest is greater than 900, Ulta is greater than 900. Do you know of any other labs that may be able to give a specific number without a limit? It’s hard to see the progress if there’s no way to reference it. My doctor is helpful at the moment either. Thank you.
Desire – thank you so much for sharing your journey. I do understand! This is an issue I’ve had as well and I’m sorry but I do not have another lab option at this time that will go higher. Please let me know if you find another.
Hello Dr. Wentz, thank you for the incredible article, I learned a lot! I have a family history of Hyperthyroidism, my grandma, my aunt and my mom all had it when they were in their 40’s. And I recently found out my TPO AB is positive with 34IU/ml, with normal TSH level, even though it’s not super high but I am afraid it’s going to be worse soon since it runs in the family. I read online that people who follow a gluten free diet see improvements in their antibody level as well as TSH levels, is it true? Should I start to eat gluten free? What are your suggestions for natural remedies to lower the antibody if there’s any? Thank you so much!
Sirena – thank you for reaching out! ❤️ Going gluten free is always the first step that I recommend. Through my research, I’ve found that a good percentage feel better off gluten. About 20% will actually go into remission by doing so. Some researchers have found that three to six months on a gluten-free diet can eliminate organ-specific antibodies. When it comes to lowering antibodeies, the IgG subclass antibodies have a half-life of 21 days and stick around on immune cells for about two to three months. They need constant “reminders” in the form of an antigen so that their production continues. If the antigen is removed, the antibodies will go away as well. The time period required for them to completely forget about the antigen and disappear is nine to twelve months.
The following things need to be in place for the antibodies to forget about the thyroid:
1) The thyroid stops expressing TPO.
2) The thyroid cells are not damaged and able to regenerate.
3) There are no substances that look like TPO (glandulars, gluten, infections, other triggers).
4) The immune system is balanced.
5) The autoimmune cells are confused by a decoy.
Some of these requirements are quick and easy, and others will take some time …
The thyroid will stop expressing TPO for two reasons. One of them is thyroid destruction, which we do not want; the other is thyroid suppression. Thyroid suppression is induced by limiting iodine and taking a thyroid supplement to bring TSH to 1 mIU/L or so. This can take up to three months
In the case of autoimmune conditions, traditional and alternative medicine practitioners may focus on rebalancing the immune system (i.e. steroids and immune-modulating drugs used in traditional medicine, or else herbs, supplements, or acupuncture used in alternative medicine).
While this approach may be helpful for taming the immune system in the short term or
overcoming autoimmune flares, it is often a temporary solution and the immune system may become imbalanced again once the medications,acupuncture, and herbs and supplements are
stopped if the underlying issue that lead to the immune system imbalance is not addressed. Thus we can say that immune modulation treats only the symptoms, and not the root cause.
As we can’t change genes, our approach to addressing the root cause of Hashimoto’s is threefold:
1) Reducing triggers
2) Eliminating intestinal permeability
3) Providing the body with nutrients to regenerate
Identifying and eliminating triggers and toxins will likely take a few weeks to a few months. Providing the thyroid with the nutrition needed to help rebuild and detoxify will likely take three to six months.
Rebalancing the immune system by addressing the root cause of autoimmunity (intestinal permeability, gut dysbiosis, infections) may take one to three years, but in the meantime, we can modulate the immune system and throw our thyroid antibodies a decoy. Hope this helps! Here are a couple articles you might find helpful:
IS GLUTEN THE ROOT CAUSE OF YOUR THYROID CONDITION?
https://thyroidpharmacist.com/articles/gluten-root-cause-thyroid-condition/
HASHIMOTO’S AND THYROID ANTIBODIES
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
My brother was just diagnosed with Hashimoto disease but has had hypothyroidism for years, from the article it sounded like Hashimoto diagnosis was the first step and then you acquired hypothyroidism. I believe the reason they tested his antibodies is because he was symptomatic that’s my thoughts I enjoyed your article very much thank you. I also have hypothyroidism I’ll be asking to have my antibodies tested
Hope – thank you so much for sharing your journey as well as your brothers! I’m so glad you found this article helpful and I hope you will keep me posted on your progress. ❤️
Dear Izabela Wentz,
Just like you, I was diagnosed with Hashimoto and no further options were offered except to wait and react to any complications. Whilst being an individual scientist and analyst myself in other areas I also decided to further investigate my condition and help myself naturally through a diet. I read Hashimoto’s protocol and now I found this comprehensive article on Thyroid antibodies. I put myself on a grain-free diet since December 2020. My TPO antibodies started going down each month (Dec-774, Feb-662, Mar 618, ) but my Thyroglobulin antibodies keep on going up Dec-303, Feb-300, Mar 345, Apr 2021 – 405. I had a strict diet for one month (Jan) and this is the only time when the Tryroglobulin antibodies dropped by 3 points. Then I started to lessen my diet. Any clues on why TPOs go down whilst AGabs go up? Thank you.
Evgeniy – thank you so much for sharing your journey. ❤️ About 95% of people with Hashimoto’s have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body’s response. Here is an article you might find interesting:
HASHIMOTO’S AND THYROID ANTIBODIES
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
Dear Izabella Wentz,
I have been struggling with unexplainable fatigue, gut issues, muscle pain and cramps – all of which have been crippling my life since almost a decade. I learnt about the antibody test by chance and did this to receive results ranging above 1500 U/ml but unfortunately my doctor still says there’s nothing to worry about as my Tsh levels are normal. I know there’s a problem but honestly I have no idea how to convince a doctor that my symptoms are genuine. Can you please advise on my test results and provide any guidance?
Thanks so much.
Amy – thank you for reaching out. I’m so sorry you are struggling with all these symptoms. They are common symptoms of thyroid disease. Unfortunately, I am not able to advise you on your test results and options without a comprehensive health assessment. I recommend that you discuss this with your personal doctor who is familiar with you health history. I do have some articles that I hope you will find helpful:
11 STRATEGIES TO OVERCOME HASHIMOTO’S FATIGUE
https://thyroidpharmacist.com/articles/strategies-overcome-hashimotos-fatigue/
6 DIFFERENT ROOT CAUSES OF LEAKY GUT
https://thyroidpharmacist.com/articles/root-causes-leaky-gut-and-autoimmunity/
PAIN MANAGEMENT AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/pain-management-and-hashimotos/
My TSH, T4 and T3 were all with in normal range. But my TPO was 72 which is above the 35 but far below some of peoples comments I have seen. Should I be concerned?
Janice – thank you for reaching out. ❤️ Amazing to hear that your antibodies are dropping! The question is, are you still struggling with symptoms? If so then you may want to consider digging deeper and find out what could be causing them. The article above as well and the Part 2 of this may be helpful for you.
Dear Izabella,
I find the table “Thyroid Panel Reference and Optimal Ranges” superbly helpful to rationalise correlation between my symptoms (mainly fatigue) and my blood test results. Would you have a more precisely weblink to IFM for the source? Or is that restricted to practitioner’s access?
I think I am at stage 2 / 3 as defined in your book. I’ve managed to calm down my TPOAb to within “standard” reference range, but my TSH swings around the optimal range, and my FT3 & FT4 have been firmly in the sub-optimal ranges. Combined with chronic iron deficiency anaemia (IDA), fatigue episodes can happen “unexpectedly”.
To your knowledge, would iron supplementation alone help to redress both conditions, or would thyroid hormone replacement warrant a trial at this stage?
Thanks a million for clearing the fog for all of us.
Ivy – thank you for reaching out. ❤️ Certainly if your iron is low you would want to consider ways to bring that up. As for medications, if your thyroid hormone levels are not optimal, thyroid medications can help you optimize them. Taking thyroid medications can also help reduce symptoms and thyroid antibodies. I’m a big fan of using everything we can to get ourselves better. That said, many people find that thyroid medications do not eliminate all of their symptoms, and they need to address their personal root causes of Hashimoto’s in order to feel better. It’s important to note, however, that some people are able to wean off thyroid medications once they figure out their triggers and address them. Here are a couple articles you might find helpful as well:
MEDICATIONS FOR HASHIMOTO’S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/
12 STRATEGIES TO OVERCOME HASHIMOTO’S FATIGUE
https://thyroidpharmacist.com/articles/12-strategies-overcome-hashimotos-fatigue/
I’ve had Hashimoto’s twice. First time, it was caused by the Mirena IUD. It took 5 years (2017-2021) to get the TPO down from 396 to 20. Dec 2021, I was diagnosed with a UTI, and given antibiotics. I felt off during Christmas, and asked for my thyroid to be tested in Jan 2022. My TPO shot up from 20 to 325. Got my 6 month lab results back today, and TSH dropped to 7 from 19, free T4 raised slightly, free T3 is fine, and TPO went from 325 to 143. I know it was a combo of the UTI and antibiotics that caused my TPO to go back up, and my doctor agrees with me. I did lower the amount of iodine I take from 50mg to 12.5-18mg (do not have any side effects from iodine), because I don’t need 50mg, anymore. I cannot take Synthroid or Levothyroxine, because I am allergic to acacia gum and it causes vitiligo. I do not take any other thyroid med, because I really don’t have any systems. We must advocate for ourselves. All my Endocrinologist wanted to do is throw Levothyroxine at me, and tell me, she is not Dr. Google. I’m so glad for my new PCM who will not force me on medication.
Jennifer – thank you so much for sharing your journey. I’m so glad to hear you have found a practitioner who will listen and that you are feeling better. ❤️ Please keep me posted on your continued progress.
Thank you so much for this. It’s pretty sad that I had to beg my Dr to test for more than the basic T amount. I only have had the PTO now which was 277.7 while the usual test was normal. Why should I have to beg to have a test done when I tell them my symptoms of extreme exhaustion and excessive hair loss among other things. We know our bodies and they just don’t listen. It’s incredibly frustrating. Now I know what else I need to insist on. Thank you again
Kim – you are very welcome. ❤️ I understand how hard it is to find a practitioner who will listen. I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
I got a blood panel back and before I was told I was borderline low for my thyroid. But now that I have numbers, no one has gone over numbers with me.
T3 2.99pg/mL (range 2.18-3.98)
TSH sensitive 0.752 uIU/mL (range 0.358-3.740)
T4 total.EPI 6.79 (range 4.5-11.7)
Thyroid peroxidase AB.EPI <15 IU/mL (range <15-35)
I’m most curious about the last…so does that mean I’m out of range and what does that mean?
Thank you!!!
Amanda – Since you are under 35, then you are no longer considered to “have Hashimoto’s on a blood test.” I like to think of remission as a journey, not necessarily a final destination. As far as the difference between remission and having no antibodies, remission is when you are no longer symptomatic. ❤️
Hello Dr. Wentz. I am at my wits end. I’ve been feeling bad for way over a year now, extreme fatigue, irregular and very heavy periods, body odor, dry hair and brittle nails. I’ve had my tsh level tested every year as I’ve been on thyroid medicine for 19 or so years. It always comes back ok. I finally had my doctor run other tests including Estradiol, progesterone, Luteinizing Hormone, Follicle-Stimulating Hormone, DHEAS, cortisol, Thyroid-Stimulating Hormone, free T3, free T4, Thyroid Peroxidase Antibodies, and free testosterone. Everything came back normal except Thyroid peroxidase antibodies. Those were 228. My doctor says it’s not my thyroid because my T3 and T4 are ok and swears it’s my hormones. What do you think? Where should I go from here? Thank you for your input!
Leanne – thank you for reaching out. Antibodies are a sign of an autoimmune attack on the thyroid, which indicates an autoimmune thyroid disease like Hashimoto’s or Graves’. If the attack on the thyroid gland persists, the damage done to the thyroid will progress, and symptoms may appear as you progress from the early to later stages of Hashimoto’s. But the good news is we can reverse this progression and put autoimmune disease into remission by addressing the underlying root causes of it, such as food sensitivities and infections. Here are some articles I think you might find helpful:
HASHIMOTO’S AND THYROID ANTIBODIES: PART 1
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
This is a great article, i have just had my TPO-Ab test come back as 225 iu/ml (UK based). this has been investigated as we are going through fertility with 2 failed embryo transfers.
I was put of levothyroxine to bring my TSH down to <2 based on optimisation for fertility. I have been on 75mcg of levothyroxine for the past 4ish months, however left wondering if the levo medication should have brough the TPO-Abs down or if i need to adjust the medications even though my TSH is 1.2
Jane – Thank you so much for your feedback! According to the American Thyroid Association, Trimester-specific reference ranges for TSH are recommended as the following: first trimester, 0.1–2.5 μIU/mL; second trimester, 0.2–3.0 μIU/mL; third trimester, 0.3–3.0 μIU/mL, and TSH levels should be monitored every 4 weeks during the first half of pregnancy and dose adjustments to medications (if they are being used) should be adjusted as needed and then checked at least once again between 26 and 32 weeks of gestation. I have an article here that I hope you find helpful: https://thyroidpharmacist.com/articles/hashimotos-and-pregnancy/
Hello Dr. Wentz, I just curious if a person has had higher than optimal TSH and both free T3 and free T4 in the lower half of normal range, particularly free T4 0.9 with normal starting at 0.8 and free T3 was 2.8 with normal starting at 2.3 and positive for tpo antibodies was does this mean according to the 5 stages of Hashimoto’s? I have had elevated TSH over normal ranges and almost every time over optimal range in the last 10+ years I have been checked. I believe I have seen my TSH at 1. something only one time during all these years, every other time always over 2 with numbers generally ranging in the 3 something range or higher. I was told many years ago I had subclinical hypothyroidism based on elevated TSH. I can’t seem to figure out what stage I fall under due to inconsistent thyroid numbers.
Thank you for your time.
Tracey – thank you for reaching out and sharing your journey. Antibodies are a sign of an autoimmune attack on the thyroid, which indicates an autoimmune thyroid disease like Hashimoto’s or Graves’. If the attack on the thyroid gland persists, the damage done to the thyroid will progress, and symptoms may appear as you progress from the early to later stages of Hashimoto’s. But the good news is we can reverse this progression and put autoimmune disease into remission by addressing the underlying root causes of it, such as food sensitivities and infections. Here are is an article I hope you find helpful:
5 STAGES OF HASHIMOTO’S THYROIDITIS
https://thyroidpharmacist.com/articles/5-stages-hashimotos-thyroiditis
Hi Dr. Wentz,
I’ve been diagnosed with hypothyroidism since 2014, I’m 32 years old. I recently found a cyst on my thyroid, and have been having more symptoms. And after begging my doctor to get the antibody tests done, she finally did. (Thyroid issues run in the family and my sister has Hashimotos). My antibody test came back positive for antibodies at a current level of 81, while my TSH, T3 & T4 were in “normal” ranges. When I went to get a specialist’s opinion, he only asked me about childhood trauma and said there was no point to the antibody test because it’s treated the same. So, now I feel like I’m crazy, even though it still feels wrong inside. It’s been months of fighting with doctors to listen, and now after seeing a specialist I’m more confused than ever. Do you have any advice?
Thank you,
Emily
Emily – thank you for sharing your journey. I understand how confusing this can be. Nodules and goiters are often the result of toxicity and/or the autoimmune process. As for antibodies, they are a sign of an autoimmune attack on the thyroid, which can definitely lead to symptoms. Addressing the root causes of the autoimmunity can help reduce symptoms. Here is an article you may find helpful.
THYROID NODULES
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-nodules/
so i have high TPO and normal TSH and doctors wont do anything. I have had palpatations and pulsations around my chest and neck for over a year. I dont know what to do?
Imran – I’m so sorry you are struggling. Some have benefitted from magnesium or selenium to help with palpitations. I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
Good Morning,
Thank You for the article. It was very nice to be able to understand what is going on with this.
I have a TPO ab of 430 and TSH T4 of 3.4.
So if the earliest “warning” about Hashimoto’s, and our best opportunity for early intervention, is during Stage 2 when we initially find evidence of thyroid antibodies, then what interventions can I do to prevent this from progressing?
Because from what I read most Doctors with my findings, will just keep checking the TSH on and off as the form of treatment for having high TPO ab and normal TSH…
Thank You!!
Maria
Maria – thank you for reaching out. Here is an article that I hope is helpful: https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
I have <1 Iu/ml antibodies but my TSH has been mildly elevated 3.5-4.5… my RF factor also high. Not sure what is the issue since I dont have any hashimoto related antibody.