Over a decade ago, when I was initially diagnosed with hypothyroidism, I was experiencing shooting pain in both of my hands and arms, and was eventually diagnosed with carpal tunnel syndrome (CTS).
My initial reaction was that it must be due to all of the writing I was doing at my job at the time. I had to write reports for my job for approximately one to two hours a day, so I got an ergonomic assessment at my workstation and started using dictation software instead of typing. While the dictation software gave me quite a chuckle at the things it came out with (for example, it reported that the client who was taking the medication “temazepam” was taking “a maze of ham”), the pain persisted.
I thought that perhaps it was my yoga class that was contributing, so I stopped going.
I took NSAIDs every day to deal with the pain, just so that I could get through the day. It got so bad at one point that I ended up wearing braces on both arms – all day and night – for about six months.
While many people think of carpal tunnel as a condition caused by repetitive keyboard use (I know I did at the time), it really isn’t. While computer use and other repetitive wrist movements can certainly exacerbate CTS, they are most often not the primary cause.
I subsequently learned that the risk of having carpal tunnel increases during pregnancy as well as in people with hypothyroidism, rheumatoid arthritis, diabetes, obesity, and other inflammatory and metabolic health conditions.
I know so many people who have had surgery for carpal tunnel syndrome, but I was hoping to avoid surgery if I could. I did some research and made just a few changes, and voilà – my carpal tunnel was gone within two weeks! Since then, I’ve been able to do 30-day yoga challenges and write five books. On a daily basis, I often spend far more than two hours writing (especially when I have a book deadline).
My ergonomic setup in my office isn’t perfect, yet I have had zero carpal tunnel for over ten years, except for a one-time occurrence in 2017. I repeated the same protocol, and it went away again within two weeks!
I’ll share my protocol, as well as the connection between thyroid hormones and carpal tunnel (in case you’re curious).
In this article, you will learn:
- The common symptoms and progression of carpal tunnel syndrome
- What causes CTS and risk factors
- The connection between Hashimoto’s and carpal tunnel syndrome
- Why conventional treatment often results in surgery
- My very simple carpal tunnel protocol
- The root cause approach to carpal tunnel syndrome
- Alternative treatments that may help support carpal tunnel symptoms
What is Carpal Tunnel Syndrome?
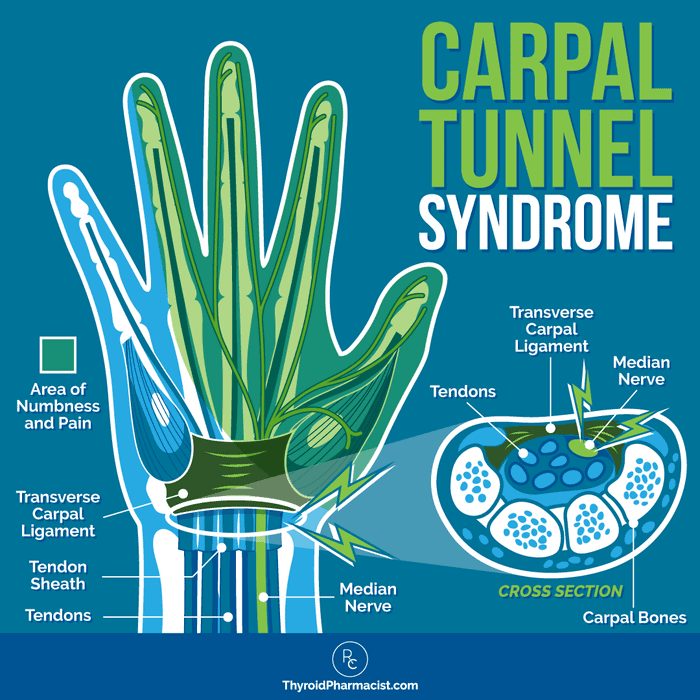
Carpal tunnel syndrome is named after the “tunnel” in the wrist, which is made up of a tough band of tissue and the bones of the wrist (see graphic). The median nerve runs through this narrow tunnel.
When this nerve gets squeezed or becomes inflamed, it can cause pain and irritation. There are other factors that can also lead to the nerve being compressed or irritated.
Carpal tunnel syndrome (CTS) is a condition where this nerve gets pinched, causing pain (nerve pain is referred to as neuropathy). It’s one of the most common issues that affects the nerves in the arms and hands, with an estimated 0.6 to 5.8 percent of the general population experiencing CTS. [1]
Any time a nerve is damaged in the body, we’re likely to experience pain, numbness, tingling, or weakness in the damaged area. Another common nerve condition you may have heard of is sciatica. The sciatic nerve runs from the lower back down each leg, and when this nerve is damaged or inflamed, it produces pain similar to that of CTS.
Symptoms of Carpal Tunnel
I mentioned earlier that I experienced shooting pain and tingling in my hands and arms — this is probably the most common symptom of carpal tunnel, and can range from mild to severe.
CTS symptoms typically begin gradually with aching discomfort in the hand, wrist, forearm, or arm. Symptoms can start off mild and become chronic. There is usually paresthesia (“pins and needles”) in the median nerve area on the palm side of the hand.
The symptoms may be further provoked (not caused) by extending or flexing the wrist, like when we use a keyboard and mouse, sleep with bent wrists, and perform other repetitive wrist motions.
In about half of cases, CTS starts in both hands, but it can also appear in just one hand (usually the dominant one). [2]
Symptoms occur in the specific areas shown shaded in blue (the thumb, index, and middle fingers, the palm side of the wrist, and the radial half of the ring finger). Sometimes (as happened to me), the pain will shoot up the forearm (and can radiate to the shoulder in rare cases).
Symptoms are often worse at night. Research has found that some 80 percent of people with CTS experience nighttime waking, and many have significant issues relating to sleep quality. [3] People will awaken with the sensation they need to shake out their hand in order to provide relief. This is referred to as the “flick sign” and occurs in the large majority of people (some 96 percent). [4]
There can also be a sense of the hand being painfully cold. Over time, there may be periods of remission, as well as worsening of the condition. [5]
People may self-diagnose carpal tunnel as a strain due to computer use or repetitive use of the hand, and many utilize home remedies such as NSAIDs, ice, and limiting computer use.
Wrist braces may help reduce irritation, and many wear them during computer use or at night, but they have not been shown to resolve the underlying inflammatory condition.
In people who do not receive treatment over an average of two years, about 29 percent experience continuing (yet stable) symptoms, about 23 percent will see symptoms worsen, and some 48 percent will show symptom improvements. [6]
Note that as the condition progresses, sensory complaints (pain, tingling) may evolve into serious motor problems, such as difficulty holding objects, weakness of the thumb, and clumsiness when using the hands.
Carpal Tunnel Syndrome: Causes and Risk Factors
Carpal tunnel syndrome is caused by compression resulting in pressure changes within the tunnel and on the median nerve. Any increase in pressure may irritate the nerve and surrounding structures, resulting in edema (excess fluid causing nerve swelling), as well as further restricting the movement of the nerve (the ligament becomes thicker and blood flow may be constricted).
This becomes a vicious cycle, leading to more irritation and inflammation with the structural integrity of the nerve and surrounding connective tissue. At this point, repetitive wrist motion will further injure the nerve. Any of the nine tendons traveling through the tunnel can also become inflamed and further compress the nerve. [7]
Studies have demonstrated a relationship between the duration and amount of pressure, and the extent of median nerve damage. [8] This is why it is important to address underlying inflammatory causes as soon as the condition is diagnosed.
Here are some of the physical factors that cause compression and the pressure changes that ultimately lead to the nerve dysfunction of CTS — it is usually a combination of more than one factor:
- Physical trauma or injury: A wrist fracture or arthritis can inflame or narrow the tunnel, resulting in increased pressure on the nerve. Cysts, scar tissue, infections, or a tumor can occur in the tunnel and increase pressure. [9]
- Stiffened connective tissue: Stiffened tissue can be the result of aging or previous injuries. This can impact joint motion, as well as the protective function of connective tissue. It is estimated that in normal individuals, the median nerve has a range of motion up to 9.6 mm — but in the presence of stiff connective tissue, this can be more limited and result in abrasive forces, which can lead to the nerve being stretched and inflamed. [10]
- Reduced nerve conduction: This is often seen in aging, hypothyroidism, and obesity. The median nerve is covered with a protective myelin sheath that is also responsible for nerve conduction. Increased pressure can impair the myelin (thinning it, changing its shape, causing lesions to form) and result in slower and dysfunctional nerve conduction. [11]
- Reduced blood flow supplying the nerve (ischemia): Compression may be caused by a thickening of the walls of the blood vascular supplying the peripheral nerve. [12]
- Changes in synovial fluid: A protective sheath known as the synovium covers tendons, keeping them lubricated with synovial fluid to reduce slide resistance between tendons (helping to maintain blood flow as well). This fluid can build up, resulting in swelling and inflammation. [13]
- Nighttime (bedtime) increases in pressure: Fluids in the body and resultant pressure in the carpal tunnel, may change during sleep due to being in a sleeping position (which redistributes fluids to the upper limbs), keeping the wrist in a bent position (common in people who sleep in the fetal position), a fall in natural cortisol levels, or increased blood pressure occurring in the late half of the night. [14]
Now, let’s talk about the genetic and lifestyle factors that may increase your risk of developing CTS.
You’ll see that several of these risk factors are also common root causes for Hashimoto’s and other autoimmune conditions. This isn’t surprising when you consider that CTS is an inflammatory condition that has also been tied to autoimmunity. [15]
Note that there are many factors that you have control over. That’s very empowering! Here are the risk factors for CTS:
Age and Gender
CTS is more common in women, with a female-to-male ratio of approximately 3 to 1. [16] One reason for the increased risk for women may be that they are more likely to have a smaller or narrower wrist, and there are also hormone-related (estrogen) influences relating to CTS (more on this below). CTS is more prevalent in adults between the ages of 40 and 60.
Obesity
Studies have found an association between greater body mass index (BMI) and CTS. [17] One study found that those with a BMI greater than 29 had a 2.5 times greater risk for CTS than individuals with a BMI under 20. [18]
Another study found that with every unit increase in body mass, there was an eight percent increased risk of CTS. [19] The mechanism could be related to increased fatty tissue in the tunnel and/or increased fluid pressure within the carpal tunnel. [20]
Additionally, obesity, as a component of the metabolic syndrome (a group of conditions that includes hypertension, insulin resistance, pre-diabetes, and diabetes), is already associated with increased risk for peripheral neuropathy conditions in general, including CTS. [21]
Genetics
Genetic factors include molecular or structural differences (narrowness of the carpal tunnel, shape of the wrist, connective tissue characteristics), pain mechanisms within the body, or a predisposition to underlying inflammatory disease states such as hypothyroidism, diabetes, or obesity. [22] One study on female twins found that genetic factors accounted for nearly half of the risk of developing CTS in women. [23]
Hormonal Fluctuations (Female)
A woman’s fluctuating sexual hormones appear to be associated with CTS, with increasing occurrence seen at times of hormonal transition such as pregnancy and menopause, as well as with the use of oral contraceptives, oral estrogen hormone replacement therapy (HRT), and aromatase inhibitors (medications that stop the production of estrogen in postmenopausal women at risk for breast cancer). [24]
Bilateral oophorectomy (removal of the ovaries resulting in surgical menopause) has also been associated with increased risk, although research on both oophorectomy and HRT effects has been mixed. [25] In these instances of hormonal fluctuation, there appear to be changes in fluid equilibrium within the tunnel and around the nerve (leading to inflammation, swelling, and compression). Estrogen may have an effect on the collagen composition of synovial tissue in the tunnel. [26]
Estrogen and progesterone receptors have been found in biopsies of carpal tunnel ligaments and tissues, so there is evidence that these hormones have a direct effect on the median nerve and surrounding tissue. [27]
Pregnancy
Carpal tunnel symptoms often appear in the last trimester of pregnancy and most often subside after delivery. However, about half of those affected may still complain of symptoms beyond pregnancy. Anywhere between 0.34 to 25 percent of pregnant women experience CTA. [28]
Poor Ergonomics and Occupational or Environmental Motor Factors
Repetitive use of the flexor muscles (or prolonged use of the wrist outside of the neutral position), excessive wrist extension or flexion, or exposure to vibration can worsen the condition by increasing pressure on the nerve. [29]
Extension of the wrist may increase the pressure to more than 10 times its initial level, while flexion of the wrist causes an eight-times increase in the pressure. [30] With that said, little research has found that the use of computers is related to an increased risk of developing CTS (only exacerbating it). [31]
Smoking
Smoking is inflammatory, negatively affects the body’s immune system, and has been found to be a risk factor for CTS. [32]
Food Sensitivities
The typical “Western diet,” rich in sugar and processed foods, promotes inflammation by triggering the production of free radicals, histamine, interleukins, and other pro-inflammatory compounds. At the same time, it lacks essential nutrients and antioxidants. [33]
Food sensitivities and joint pain are common for those with Hashimoto’s. Removing foods such as gluten and dairy, which are common reactive foods for those with Hashimoto’s, can reduce neuropathic pain (as well as decrease thyroid antibodies). [34]
Chronic pain can be a result of this type of persistent pro-inflammatory state.
Stress
Chronic stress is very inflammatory and known to be a trigger for Hashimoto’s. [35] There has been limited research on stress and its effects on CTS, but in one study, women with severe carpal tunnel syndrome were found to have higher concentrations of cortisol, and an imbalance in the hypothalamic-pituitary-adrenocortical (HPA) axis, suggesting stress may play a role in CTA symptoms. [36]
Underlying Inflammatory Health States
Certain health conditions such as hypothyroidism, gout, congestive heart failure, kidney failure, diabetes, rheumatoid arthritis, amyloidosis, and connective tissue diseases may cause fluid changes or affect the lining of the tendons, causing inflammation, swelling, and compression of the nerve. [37] Metabolic syndrome is also highly associated with CTS.
Conditions That Cause Nerve Damage
There are also neuropathic factors that can directly increase the risk of median nerve damage:
- Diabetes: Diabetic patients have an increased risk of developing CTS since they are at a greater risk of nerve damage (as well as being more sensitive to compressive-related factors such as blood vessel inflammation, stiffening connective tissue, and damage due to high blood sugar). One study found that while the lifetime risk for CTS in the general population is 10 percent, this increases to 84 percent in patients with diabetes. [38] Dysregulated blood sugar is a common trigger in Hashimoto’s as well.
- Alcohol: The toxic effects of alcohol have been found to increase the risk for CTS. A study involving 1,464 workers found a 75 percent greater history of alcohol abuse in the workers with CTS. [39]
- Toxin Exposure: Studies have found that neurotoxic chemicals (such as lead, mercury, insecticides, weed killers, trichloroethylene, paints and varnishes, white spirit (mineral spirits), cellulosic diluent, inks, and dyes, are associated with a greater incidence of CTS and decreased peripheral nerve function. [40] There have been several interesting studies focused on dentists to assess their cumulative mercury exposure (from dental amalgams); these have shown a significant positive association with decreased peripheral nerve function. [41]
- Nutrient Deficiencies: Low levels of a number of micronutrients, such as zinc, magnesium, vitamins B1, B3, B6, B12, and D, and omega-3 fatty acids, are associated with chronic neuropathic or inflammatory pain, and many of these have been found to be deficient in CTS patients (as well as in those with Hashimoto’s). [42] In many cases, improvements in diet or supplementation with these nutrients can contribute to the alleviation of chronic pain of various types.
The Connection Between Hashimoto’s and Carpal Tunnel Syndrome
Over the years, I’ve learned that anything that adds to our body’s inflammation level or impacts our metabolism (whether that be reactive foods or a lack of nutrients, blood sugar, toxins, stress, hormone imbalances, infections, or other disease states), can not only trigger Hashimoto’s, but also lead to inflammatory conditions like carpal tunnel syndrome.
The thyroid gland plays an important role in tissue development and metabolism, with thyroid hormones exerting a number of effects on the neuromuscular system. Neuromuscular complaints, including muscle weakness, are found in some 20 to 80 percent of people with Hashimoto’s. [43]
Peripheral neuropathy is also associated with hypothyroidism, with carpal tunnel syndrome being the most common cause of peripheral nerve damage. [44]
In one 2000 study, researchers found that 79 percent of patients with hypothyroidism had neuromuscular complaints, with 42 percent of those experiencing sensory symptoms and pain, and 38 percent experiencing muscle weakness. Additionally, 29 percent had CTS. [45]
In several smaller studies involving people with hypothyroidism, the percentage of those with CTS has been found to be even higher (32.5 to 37.5 percent). [46]
In my own clinical observation, I have seen a high prevalence of muscle complaints, including weakness, cramps, and joint pain, in those with Hashimoto’s.
Due to the strong connection between the two conditions, some research has suggested that people with CTS should be screened for undiagnosed hypothyroidism. [47]
Mechanism of Action
Hypothyroidism may lead to the accumulation of mucinous material around the median nerve, resulting in increased fluid and swelling in the soft tissues within the carpal tunnel. This results in compression around the nerve, along with swelling and degeneration of the nerve (and reduced nerve conduction), which may lead to CTS development. Synovial thickening has also been found in cases of uncontrolled hypothyroidism. [48]
The weight gain seen in many hypothyroid patients may in part result in fluid retention (and explain why BMI is a risk factor for carpal tunnel syndrome). [49]
One study found that an increase in cross-sectional area (CSA) of the median nerve can be caused by autoimmune hypothyroidism, and that thyroid treatment resulting in target levels of TSH and free T4 reversed this. [50]
In one study involving 75 patients with hypothyroidism and musculoskeletal symptoms, 72 percent had joint pain, and 61.3 percent had CTS. Patients also had high frequencies of co-occurring disease conditions, including diabetes (16 percent), hypertension (13.3 percent), obesity (46.7 percent), cardiovascular disease (2.7 percent), and chronic renal failure (2.7 percent). The musculoskeletal issues disappeared with L-thyroxine administration in 66.6 percent of patients. [51]
Most (but not all) research and clinical observations have found that treatment of hypothyroidism improved (and in some cases resolved) CTS symptoms. Given the positive results seen, some studies have recommended that thyroid hormone replacement therapy always be considered prior to surgical intervention. [52]
Research specific to Hashimoto’s has also found that CTS symptoms resolved when optimal levels of TSH and T4 levels were achieved via thyroxine therapy. [53]
Why Conventional Treatment Often Results in Surgery
Conventional doctors will diagnose CTS based on a review of specific CTS symptoms (tingling, numbness, specific region of symptom development), looking for a history of arthritis or wrist fractures, and a clinical examination involving a variety of tests such as the Tinel test (where the doctor presses the median nerve eliciting a tingling or painful sensation as a positive indicator of the condition) and the Phalen test (a wrist flexion test in which tingling or numbness is a positive indicator of CTS). [54]
Electrodiagnostic tests may be used, where electrodes are placed on the hand and wrist, or inserted into a muscle, to measure nerve function and potential damage. Ultrasound imaging can show abnormal size of the median nerve.
These tests would likely be performed by an integrative doctor as well.
The biggest difference between conventional and integrative diagnosis and treatment, however, is the focus on the underlying cause of an individual’s carpal tunnel condition.
Conventional physicians will focus on mechanical and motor causes (repetitive wrist motion, computer use, and occupational use explanations) rather than underlying medical conditions (such as diabetes and hypothyroidism) or potential triggers (food sensitivities or nutrient deficiencies).
The frustrating thing about this is that there is research from as far back as the 1970s that has shown that common medical diseases (inflammatory, metabolic, or degenerative conditions) were 40 to 75 percent more common in those with CTS. [55] Much of the research and clinical findings at the time found that many people with CTS had diabetes, hypothyroidism, or rheumatoid arthritis, or were obese. However, in conventional medicine, these conditions are still not viewed as relevant to treatment of carpal tunnel.
I read a 1998 research publication that spoke of a workers’ compensation claim by a 59-year-old woman. I feel this case study illustrates the fundamental issue when a physician doesn’t focus on underlying causes! This particular patient had held her job for 38 years, and after much pain, was diagnosed with CTS due to the mechanics of her job. Her physician put her on permanent disability given he viewed the condition as solely a repetitive use motor issue. The woman desperately wanted to continue working. It was only later that her serum TSH level was found to be 24 mIU/L! [56]
Since conventional doctors typically focus solely on repetitive movements, they will suggest wrist splints, rest from the offending movement, over-the-counter drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs), or prescription corticosteroids (such as prednisone). But as these are really treatments that mask symptoms and pain, the condition will likely worsen, and surgery is often recommended. Carpal tunnel surgery (carpal tunnel release) is one of the most common surgical procedures in the U.S.
Integrative physicians, on the other hand, will focus on and correct the true root causes of inflammation or the metabolic issues causing the condition.
Root Cause Solutions for Carpal Tunnel
While I do feel wrist splints and over-the-counter pain meds have their place when addressing carpal tunnel (to help with short-term inflammation and pain), these pain meds can lead to further problems with gut health, can have side effects if used long-term, and don’t correct the root cause. And let’s be honest – wrist splints are so not glamorous!
That’s what I had to do back when I was first diagnosed with carpal tunnel. While my doctor recommended wrist splints and had me take NSAIDs, and the nurses at work told me to consider surgery, I found a simple protocol that helped me and hundreds of others in just two weeks.
My Very Simple Carpal Tunnel Protocol
Here’s the surprisingly simple protocol that I have found helps most cases of CTS:
- Avoid Dairy: Early on in my healing journey with Hashimoto’s, I had a food sensitivity test done that revealed that I had numerous food sensitivities, most notably, gluten and dairy. I cut these foods out of my diet and in just three days, my acid reflux, bloating, and IBS got much better. My carpal tunnel syndrome got much better, too, but wasn’t completely eliminated. The improvements I saw with changing my diet did give me the courage to dig deeper. Dairy is a common carpal tunnel trigger in many of my clients, so dairy elimination is a great place to start! Please note, this does include cow’s milk, A1/A2 milk, goat’s milk, sheep’s milk, butter and ghee. When I say all dairy, I do mean it!
- Take a P5P (B6) Supplement: In my research, I came across an article from 1987 that spoke about using vitamin B6 for carpal tunnel resolution. [57] The doses were high, which made me worry about neuropathy (yes, ironically, too much B6 can cause neuropathy, but too little may also contribute to CTS). There is a version of B6 called the pyridoxal 5′-phosphate version (P5P), which is much better absorbed and has fewer risks of side effects, so that is the version I opted for. Research suggests that B6 may improve symptoms of CTS because some underlying nerve conditions may be related to a B6 deficiency, or possibly because B6 can raise pain thresholds by acting as an analgesic. [58] I took 50 to 200 mg daily of P5P for 12 weeks, and this further improved my CTS symptoms. (Read my article on B6 for more information.)
- Chiropractic Adjustments: I had three chiropractic adjustments over a period of two weeks, and found them to be very helpful for my CTS symptoms. Chiropractic adjustments may help alleviate symptoms by improving joint alignment, enhancing nerve function, reducing tension in soft tissue, and reducing pressure on the median nerve. [59] I recommend finding an experienced chiropractor who has experience with CTS.
Once I had all these interventions in motion, my carpal tunnel vanished! I was able to write my first book, Hashimoto’s: The Root Cause, which entailed hours and hours of writing. To decompress from my day job and writing, I would go to yoga multiple times each week (I happened to have a yoga studio across the street from my home in Chicago).
Interestingly, when I was writing my second book, Hashimoto’s Protocol, I had a big carpal tunnel flare up, and I wasn’t sure what was causing it. I was on a strict book deadline, so I thought it was all of the writing.
I lived in Colorado at the time, so I tried some of the “local remedies”… and while they helped the pain, they didn’t help me focus on my writing. 😂 A few hours in, I would totally lose my focus and just look for snacks.
I then realized that I had been eating butter in a gluten-free pie I had purchased from a local vendor! I reviewed my notes on carpal tunnel, got off dairy, restarted P5P, and saw the chiropractor (I was lucky enough to have a wonderful one as a next door neighbor back then). Fortunately, the carpal tunnel went away within a week or so, and I was able to go back to my writing.
These three simple things have helped a TON of people I have worked with, and they’re generally a great place to start.
I should also mention that my thyroid hormones were already optimized when I did those three things, so that would of course be a great place to start if you haven’t yet.
Here are some additional recommendations based on my clinical experience and research.
Optimize Thyroid Medication and Hormone Levels
The research tells us there is a connection between higher TSH and carpal tunnel nerve dysfunction (thickened nerve, etc.), and that when TSH and free T4 levels are normalized, CTS symptoms will likely improve or completely resolve.
If a client has carpal tunnel symptoms, the first thing I do is assess their thyroid labs to see if their medication may need further optimization. I have found that I, as well as many other people with thyroid conditions, feel best when TSH is between 0.5 and 2 μIU/mL.
If you have a low T3 and T4, along with a high TSH, this can indicate higher levels of inflammation in the body, contributing to your CTS symptoms, and can often be addressed with a dosage adjustment. An elevated reverse T3 can also lead to carpal tunnel symptoms.
You can read about thyroid lab tests, optimal levels, and how to self-order tests if your doctor won’t, here in the linked article. Note that reverse T3 is a separate blood test.
There are many interventions that can help optimize your thyroid hormone levels and your medication’s effectiveness, as well as your body’s ability to absorb and convert your thyroid hormones (T4 to the more active T3). Many people do not convert well. Please review the linked articles for more information, or you can download my eBook Optimizing Thyroid Medications, FREE for a limited time!
Eat an Anti-Inflammatory Diet and Avoid Reactive Foods
Reducing inflammation levels can improve pain in the body as well as promote healing. As mentioned earlier, eating a “Western” diet high in sugar and processed foods is inflammatory and lacks supportive nutrients.
While there has been limited research on food sensitivities related to CTS, I have found eliminating dairy in particular to be helpful for CTS symptoms. For those with Hashimoto’s, it’s likely this is a reactive food. Gluten is another commonly reactive food in those with Hashimoto’s, and eliminating it may also help in reducing CTS symptoms. In my 2015 survey of people with Hashimoto’s, 88 percent felt better on a gluten-free diet, and 26.37 percent noted a reduction in pain.
It is worth noting that a lot of over-the-counter and steroid painkillers that people may take for CTS actually may contain fillers such as lactose. Reactive fillers, including gluten and lactose, can often be found in thyroid hormone medication as well!
The best place to start when trying to identify your own particular food sensitivities is with an elimination diet. The first step will be to remove gluten, dairy, and other foods that you suspect you may be reactive to. Some diets have also been found to reduce pain, including the gluten-free diet (47 percent), the grain-free diet (43 percent), an egg-free diet (40 percent), low FODMAPs diet (48 percent), and the Autoimmune Paleo diet (50 percent).
If you’d like to complete a food sensitivity test, Alletess is a great option that can be self-ordered. There are two options to test for the most commonly eaten foods:
- The 96 Food Panel test checks for IgG (a branch of the immune system that mediates food sensitivities as well as Hashimoto’s) reactions to 96 common foods. You can order this test through my Rupa Health or MyMedLab.
- The 184 Food Panel test checks for IgG reactions to 184 common foods. You can order this test through my Rupa Health or MyMedLab.
One additional note about leaky gut and pain — there has been some interesting research related to neuropathic pain and the gut microbiome. The research reported that the specific gut microbiota found in rats with neuropathic pain were different from that of normal rats. In particular, the ratio of Firmicutes to Bacteroidetes (F/B ratio) bacteria was significantly higher in the group having neuropathic pain than in the normal group. The F/B ratio is an indicator of health and is thought to reflect the degree of dysbiosis (bacteria imbalance) in the gut. [60]
A stool test called the GI-MAP can help you identify imbalances in gut bacteria. (Read more about the GI-MAP test here.)
Live an Anti-Inflammatory Lifestyle
Reducing inflammation goes well beyond diet. A few other important reminders as to things that can increase your overall inflammation include poor sleep, chronic stress, toxin exposure, vices (smoking, alcohol), and a sedentary lifestyle. All of these increase one’s risk for carpal tunnel (as well as being triggers for Hashimoto’s).
Address Common Nerve Pain-Related Nutrient Deficiencies
As mentioned earlier, a vitamin B6 deficiency may be related to carpal tunnel symptoms, and I’ve found P5P supplementation to be super helpful.
Research indicates that vitamin B6 may help alleviate symptoms of carpal tunnel syndrome (CTS), potentially due to its role in addressing underlying nerve issues linked to B6 deficiency, or its ability to raise pain thresholds by acting as a natural analgesic. P5P, at a dose of 50 to 200 mg daily for 12 weeks, may help improve CTS symptoms.
Other nutrient deficiencies to look into:
- Vitamin B1: Vitamin B1 (also known as thiamine) plays a vital role in nerve health, as it supports nerve function and helps maintain the protective covering of nerves (myelin sheath). [61] A deficiency in B1 can lead to nerve damage or dysfunction, potentially contributing to conditions like CTS. Thiamine also helps regulate nerve signaling and reduces oxidative stress, which may alleviate pain and inflammation in CTS. I prefer the benfotiamine form, as it is highly absorbable; two high-quality supplements I like are Rootcology Benfotiamine and BenfoMax by Pure Encapsulations.
- Vitamin B12: B12 is associated with nerve health, and research has shown it can improve nerve conduction and help with neuropathic pain. [62] I recommend supplementing with methylcobalamin (the active form of vitamin B12) like Pure Encapsulations B12, which comes in a convenient liquid form for optimal absorption.
- Alpha-lipoic acid: Some research suggests that alpha-lipoic acid may help protect nerves, reduce pain sensitivity, and act as a powerful antioxidant. It has been shown to ease symptoms and improve function in people with carpal tunnel syndrome (CTS). [63] It may also be effective for nerve damage caused by diabetes. Animal studies suggest it might boost blood flow to nerves and improve how motor nerves send signals. [64] Pure Encapsulations makes a high-quality alpha-lipoic acid supplement (a dose of 600 mg per day is used in most studies that have shown benefit, though occasionally the dose needs to be higher).
- Vitamin D: A 2020 study found that 95.8 percent of patients with carpal tunnel syndrome had a vitamin D deficiency, and with every unit increase in serum vitamin D levels, the odds of having CTS were decreased by 1.22 times. [65] A deficiency in vitamin D has also been linked to increased neuropathic pain in patients with diabetes. [66] High-quality vitamin D supplements include: Pure Encapsulations Vitamin D 5000 IU (without vitamin K) or Designs for Health Vitamin D Supreme (with vitamin K). You can purchase these through Fullscript. If you don’t have a Fullscript account, you can sign up with my credentials here.
- Magnesium: Magnesium is needed for more than 300 biochemical reactions in the body, including supporting nerve and muscle function. Studies have found magnesium to be an effective treatment for neuropathic pain. [67] Those with Hashimoto’s are often deficient in magnesium. Magnesium can be taken in supplement form as well as applied topically.
- Omega-3 fatty acids: Omega-3 fatty acids can help with inflammation, nervous system function, and pain. They are supportive of healthy joints and connective tissue. Research shows that compared with NSAIDs such as ibuprofen, omega-3 fatty acids could equally reduce arthritic pain and be a safer alternative. [68] Unfortunately, many people don’t obtain enough from their diet, so supplementation is often helpful.
If you’re interested in testing your levels of nutrients, I recommend the Spectracell Micronutrient Test.
A Note About Vitamin B6 Supplementation
**There are two cautionary notes relating to taking B6 supplementation. First relating to the dose, most studies resulting in improvements in CTS symptoms were based on doses ranging from 50 to 300 mg daily, with no adverse symptoms seen for people with an intake of less than 500 mg/day. If a person’s intake starts to approach 500 mg/day, they should be monitored for worsening neuropathy symptoms such as irritability, impaired memory, fatigue, depression, headaches, bloating, and difficulty walking.
The second caution is also related to overdosing, but points to the fact that everyone is incredibly unique. Some people may have the MTHFR gene variation, for example, in which case they may be more prone to toxicity in general. For instance, I heard from one reader who had this issue relating to various supplements containing B6, where levels of B6 built up in her system, and she wasn’t detoxing the B6 properly. She also provided me with some research relating to how lactic acid bacteria found in a few foods (some cheeses, yogurt, and fermentations) as well as the human gut, can synthesize certain B vitamins, including B6 (as well as riboflavin, folate, vitamin B12, and niacin). [69]
If you have the MTHFR gene variation, you should discuss the potential toxicity effects and the monitoring of your B6 levels with your practitioner.
Read my article on B6 for more information.
Alternative Treatments
- Chiropractic adjustment (exercises)
- Acupuncture
- Yoga
- Arnica (topical)
- Amol
- Low-level laser therapy (LLLT) or cold laser
- Platelet-rich plasma
- Herbs
- CBD
- Systemic enzymes
Chiropractic Adjustment
Studies have found chiropractic adjustment to be an effective and conservative treatment for carpal tunnel. [70] It is one of the three treatments that most helped my carpal tunnel condition.
While carpal tunnel surgery alleviates the pressure by creating more room for the median nerve, chiropractic treatment is more conservative and works to address the underlying cause of the pressure and pain.
Sometimes there may be an issue with your upper (cervical) spine, which results in increased inflammation on the median nerve. Massage therapy at the wrist can reduce inflammation and related symptoms. A chiropractor can provide exercises that can reduce pressure on the nerve, stretch the carpal ligament, help in soft tissue release, as well as help improve your range of motion and hand function (while removing pressure around the nerve). Ultrasound therapy may also be used.
Acupuncture
I have also used acupuncture for pain relief. In my survey, 61 percent of people with Hashimoto’s said that acupuncture had helped with their pain relief.
The National Institutes of Health (NIH) states that acupuncture may be an acceptable alternative for managing carpal tunnel syndrome, or useful as an adjunct treatment. [71]
While some findings have found no benefit, several have found CTS symptom relief using acupuncture. One more recent study found that acupuncture results were similar to, and in some cases better than, conventional treatment with Celebrex. [72] Another study found that acupuncture improved measured parameters related to CTS better than ibuprofen. [73]
Yoga
I love yoga, as it is a great way to engage in low-impact movement, work up a sweat, and release toxins. I especially love it out in the sun with my son. Yoga is a great way to clear the mind, strengthen your mind-body connection, and get some vitamin D.

It has also been found to provide benefits relating to carpal tunnel (specifically improvements to pain and grip strength), neurological disorders, diabetes, and pain. [74] A 2004 review found that yoga was effective as a conservative treatment modality for CTS. [75]
However, it’s important to note that this isn’t the case for everybody. Yoga as an intervention for CTS is actually quite controversial, as it may make symptoms worse for some people. It may be best to start with some of the other interventions to get symptoms under control, then engage with yoga to support long-term joint and pain support.
Arnica (Topical)
Arnica is an herbal remedy extracted from an alpine plant, Arnica montana, and has been used for the treatment of bruising, swelling, stiffness, pain, and a wide variety of inflammatory conditions, including arthritis and carpal tunnel syndrome.
Studies on its effectiveness have been mixed, but a few have found it to be effective for CTS pain, as well as in reducing pain after carpal tunnel release surgery. In that study, 37 patients found that arnica (a 5 percent solution) used for two weeks, significantly reduced pain after carpal tunnel release surgery. [76]
Many versions of topical arnica can be purchased over-the-counter and is an easy-to-try adjunct pain reliever for carpal tunnel pain and inflammation. I’ve heard many positive comments about it from readers and clients. Note that I do not recommend oral arnica tablets, as they can be toxic.
Amol
Amol has been the “all-purpose” tonic used in Poland for longer than I can remember. Depending on the product, it may contain cinnamon, clove, peppermint, lemon oil, lavender oil, citronella, and alcohol.
It is commonly used for the internal and external treatment of muscle pain, headache, sore throats, the common cold, and indigestion, as well as to promote restful sleep.
You can purchase Amol on Amazon (where you can also read many reviews). You can use it topically to relieve carpal tunnel symptoms, and for everything else that ails you – at least, this is the case according to my mom and grandma! 😉
As with arnica, it may be useful to try as an adjunct treatment option for carpal tunnel.
Low-Level Laser Therapy (LLLT)
Low-Level Laser Therapy (LLLT), or cold laser therapy, utilizes specific wavelengths of light applied with a laser to help accelerate wound healing, pain relief, peripheral nerve regeneration, and further reduction of inflammation.
Several studies have found LLLT to help with carpal tunnel syndrome. In one 2014 study of 66 patients with mild to moderate CTS, improvements were significantly greater in the LLLT-treated group. [77] A more recent study evaluating 531 patients with mild to moderate CTS found that LLLT improves hand grip and sensory nerve symptoms. [78]
Most studies have found short-term benefits and not reported on longer-term outcomes; however, it is a non-invasive procedure that may be helpful to some people.
If you’re on Instagram, I might be giving away two red light therapy devices for the next week or so. 😉 Lumebox and Orion. Check out my 12 days of Christmas giveaway here!
Platelet-Rich Plasma (PRP)
This therapy focuses on the self-healing properties of the body and is still considered very novel.
PRP is thought to reduce overall inflammation and promote neuronal regeneration in musculoskeletal conditions. Blood is taken from an individual, and platelets are removed and then reinjected into the affected area – such as into the carpal tunnel itself. Platelets are blood cells that cause blood clots, but also are involved in growth-healing functions.
Studies on PRP and CTS are limited. One small 2019 study found there were short-term improvements in carpal tunnel symptoms with a single PRP injection into the carpal tunnel, resulting in improved electrophysiological findings and symptoms. [79]
A 2020 review also found that PRP resulted in CTS improvements, but concluded that more research (to assess long-term regenerative effects in particular) was needed. [80]
Herbs
- Curcumin/Turmeric: Up to 65 percent of my readers with Hashimoto’s have reported a reduction in pain by taking turmeric (curcumin is the active compound found in turmeric), and the herb has been shown to exert significant anti-inflammatory, antioxidant, and neuroprotective effects on the peripheral nerves. [81] This is one of my go-to anti-inflammatory solutions.
- Boswellia: Boswellia extracts have a long history of use for connective tissue and joint support. Several studies have found that boswellia can be effective as an anti-inflammatory, anti-arthritis, and analgesic agent. One study found that the use of Boswellia carteri improved CTS pain and function in patients with CTS (although no change in tested electrodiagnostic parameters was found). [82]
- Chamomile: A 2015 pilot study found that chamomile helped improve function and symptoms in CTS. A follow-up 2017 study involving 86 patients with mild to moderate CTS using chamomile oil, found significant improvements in functionality, symptoms, and test measurements in the treated group. [83]
CBD
Studies involving cannabis (medical marijuana) and cannabinoids (containing THC, CBD, or both) have demonstrated they can offer effective pain relief in conditions of chronic neuropathic pain.
CBD (cannabidiol) can come in various forms (oils, edibles, tinctures, creams, and pills), and because it isn’t psychoactive like THC, it doesn’t provide the high that THC does. CBD typically will relax people, but will not affect their perception or physical reactions as much as THC. Just be careful with taking it orally! It can make you super drowsy.
The research specific to carpal tunnel is lacking, but in 2020 there was a study focused on CBD oils on peripheral neuropathy. The study found that the application of CBD oil on the skin achieved significant improvement in pain, as well as other negative sensations of peripheral neuropathy. [84]
Personally for me, CBD/THC are never my top recommendations because they can make people more fatigued and get the munchies, two things most of us with Hashimoto’s don’t need. 🙂
You can read about other holistic healing approaches to pain in this article on pain management in Hashimoto’s.
Systemic Enzymes
I have long used systemic enzymes such as Rootcology Systemic Enzymes or Wobenzym in my practice, as they can reduce thyroid antibodies, as well as reduce food sensitivities, inflammation, and pain. [85]
Enzymes have become a popular alternative to conventional pain medications for many inflammatory conditions such as arthritis. One study specific to carpal tunnel syndrome found that systemic enzyme therapy reduced the incidence and severity of median nerve pain. [86] Systemic enzymes work by breaking down inflammatory cytokines.
Final Words on Carpal Tunnel
While repetitive motions may exacerbate carpal tunnel, it is important to address the underlying causes of inflammation in order to fully heal from the condition.
The good news is that many of the interventions that have been shown to alleviate CTS symptoms and the condition’s progression also are thyroid-supportive. Several have been tied to reductions in TSH, thyroid antibodies, and improvements in Hashimoto’s symptoms.
The easiest way to address peripheral nerve issues such as CTS is to start with thyroid hormone optimization, eliminate dairy, take a P5P supplement, and see your favorite chiropractor. For many people, this will resolve the majority of carpal tunnel symptoms or even heal the problem completely (as it did with me).
You will find a good deal of support for all of these topics on my website. Check out the linked articles for greater details and more specific recommendations.
Addressing pain is a frequent topic, and so important to our well-being! We are on this journey together.
P.S. You can also download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free, by signing up for my weekly newsletter. You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow me on Facebook, Instagram, Pinterest, and TikTok!
References
[1] Wipperman J, Goerl K. Carpal tunnel syndrome: diagnosis and management. Am Fam Physician. 2016 Dec 15;94(12):993-999.; van Dijk MA, Reitsma JB, Fischer JC, et al. Indications for requesting laboratory tests for concurrent diseases in patients with carpal tunnel syndrome: a systematic review. Clin Chem. 2003 Sep;49(9):1437-44.
[2] Bland JD, Rudolfer SM. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom, 1991-2001. J Neurol Neurosurg Psychiatry. 2003;74(12):1674-1679. doi:10.1136/jnnp.74.12.1674
[3] Patel JN, McCabe SJ, Myers J. Characteristics of sleep disturbance in patients with carpal tunnel syndrome. Hand (N Y). 2012;7(1):55-58. doi:10.1007/s11552-011-9373-1
[4] Wipperman J, Goerl K. Carpal tunnel syndrome: diagnosis and management. Am Fam Physician. 2016 Dec 15;94(12):993-999.
[5] Muller M, Tsui D, Schnurr R, Biddulph-Deisroth L, Hard J, MacDermid JC. Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17(2):210-228. doi:10.1197/j.jht.2004.02.009
[6] Schmid AB, Fundaun J, Tampin B. Entrapment neuropathies: a contemporary approach to pathophysiology, clinical assessment, and management. Pain Rep. 2020;5(4):e829. Published 2020 Jul 22. doi:10.1097/PR9.0000000000000829
[7] Yoshii Y, Zhao C, Amadio PC. Recent Advances in Ultrasound Diagnosis of Carpal Tunnel Syndrome. Diagnostics (Basel). 2020;10(8):596. Published 2020 Aug 15. doi:10.3390/diagnostics10080596; 1. Sevy JO, Sina RE, Varacallo M. Carpal Tunnel Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448179/
[8] Wahab KW, Sanya EO, Adebayo PB, Babalola MO, Ibraheem HG. Carpal Tunnel Syndrome and Other Entrapment Neuropathies. Oman Med J. 2017;32(6):449-454. doi:10.5001/omj.2017.87
[9] Cranford CS, Ho JY, Kalainov DM, Hartigan BJ. Carpal tunnel syndrome. J Am Acad Orthop Surg. 2007;15(9):537-548. doi:10.5435/00124635-200709000-00004
[10] Aboonq MS. Pathophysiology of carpal tunnel syndrome. Neurosciences (Riyadh). 2015;20(1):4-9.
[11] Wahab KW, Sanya EO, Adebayo PB, Babalola MO, Ibraheem HG. Carpal Tunnel Syndrome and Other Entrapment Neuropathies. Oman Med J. 2017;32(6):449-454. doi:10.5001/omj.2017.87
[12] Wahab KW, Sanya EO, Adebayo PB, Babalola MO, Ibraheem HG. Carpal Tunnel Syndrome and Other Entrapment Neuropathies. Oman Med J. 2017;32(6):449-454. doi:10.5001/omj.2017.87
[13] Aboonq MS. Pathophysiology of carpal tunnel syndrome. Neurosciences (Riyadh). 2015;20(1):4-9.
[14] Ibid
[15] Moalem-Taylor G, Baharuddin B, Bennett B, et al. Immune dysregulation in patients with carpal tunnel syndrome. Sci Rep. 2017;7(1):8218. Published 2017 Aug 15. doi:10.1038/s41598-017-08123-6
[16] van Dijk MA, Reitsma JB, Fischer JC, Sanders GT. Indications for requesting laboratory tests for concurrent diseases in patients with carpal tunnel syndrome: a systematic review. Clin Chem. 2003;49(9):1437-1444. doi:10.1373/49.9.1437
[17] Schmid AB, Fundaun J, Tampin B. Entrapment neuropathies: a contemporary approach to pathophysiology, clinical assessment, and management. Pain Rep. 2020;5(4):e829. Published 2020 Jul 22. doi:10.1097/PR9.0000000000000829; Gupta N, Arora M, Sharma R, Arora KS. Peripheral and Central Nervous System Involvement in Recently Diagnosed Cases of Hypothyroidism: An Electrophysiological Study. Ann Med Health Sci Res. 2016;6(5):261-266. doi:10.4103/amhsr.amhsr_39_16
[18] Karne SS, Bhalerao NS. Carpal Tunnel Syndrome in Hypothyroidism. J Clin Diagn Res. 2016;10(2):OC36-OC38. doi:10.7860/JCDR/2016/16464.7316
[19] Newington L, Harris EC, Walker-Bone K. Carpal tunnel syndrome and work. Best Pract Res Clin Rheumatol. 2015;29(3):440-453. doi:10.1016/j.berh.2015.04.026
[20] Roquelaure Y, Garlantézec R, Rousseau V, et al. Carpal tunnel syndrome and exposure to work-related biomechanical stressors and chemicals: Findings from the Constances cohort. PLoS One. 2020;15(6):e0235051. Published 2020 Jun 25. doi:10.1371/journal.pone.0235051; Karne SS, Bhalerao NS. Carpal Tunnel Syndrome in Hypothyroidism. J Clin Diagn Res. 2016;10(2):OC36-OC38. doi:10.7860/JCDR/2016/16464.7316
[21] Roquelaure Y, Garlantézec R, Rousseau V, et al. Carpal tunnel syndrome and exposure to work-related biomechanical stressors and chemicals: Findings from the Constances cohort. PLoS One. 2020;15(6):e0235051. Published 2020 Jun 25. doi:10.1371/journal.pone.0235051; Paiva HR, Paiva VDGN, Oliveira EF, Rocha MA. PROFILE OF PATIENTS WITH CARPAL TUNNEL SYNDROME TREATED AT A REFERRAL SERVICE. Acta Ortop Bras. 2020;28(3):117-120. doi:10.1590/1413-785220202803227138
[22] Schmid AB, Fundaun J, Tampin B. Entrapment neuropathies: a contemporary approach to pathophysiology, clinical assessment, and management. Pain Rep. 2020;5(4):e829. Published 2020 Jul 22. doi:10.1097/PR9.0000000000000829
[23] Hakim AJ, Cherkas L, El Zayat S, MacGregor AJ, Spector TD. The genetic contribution to carpal tunnel syndrome in women: a twin study. Arthritis Rheum. 2002;47(3):275-279. doi:10.1002/art.10395
[24] Chien HC, Kao Yang YH, Kwoh CK, Chalasani P, Wilson DL, Lo-Ciganic WH. Aromatase Inhibitors and Risk of Arthritis and Carpal Tunnel Syndrome among Taiwanese Women with Breast Cancer: A Nationwide Claims Data Analysis. J Clin Med. 2020;9(2):566. Published 2020 Feb 19. doi:10.3390/jcm9020566
[25] Chai T, Copeland R, Vangeison C, Lam L, Reeh C, Briggi D. Carpal Tunnel Syndrome. PM&R KnowledgeNow. July 5, 2023. Accessed December 1, 2024. https://now.aapmr.org/carpal-tunnel-syndrome/.; Al-Rousan T, Sparks JA, Pettinger M, et al. Menopausal hormone therapy and the incidence of carpal tunnel syndrome in postmenopausal women: Findings from the Women’s Health Initiative. PLoS One. 2018;13(12):e0207509. Published 2018 Dec 4. doi:10.1371/journal.pone.0207509
[26] Song CH, Gong HS, Bae KJ, Kim JH, Nam KP, Baek GH. Evaluation of female hormone-related symptoms in women undergoing carpal tunnel release. J Hand Surg Eur Vol. 2014;39(2):155-160. doi:10.1177/1753193413484873
[27] Toesca A, Pagnotta A, Zumbo A, Sadun R. Estrogen and progesterone receptors in carpal tunnel syndrome. Cell Biol Int. 2008;32(1):75-79. doi:10.1016/j.cellbi.2007.08.014
[28] Stolp-Smith KA, Pascoe MK, Ogburn PL Jr. Carpal tunnel syndrome in pregnancy: frequency, severity, and prognosis. Arch Phys Med Rehabil. 1998;79(10):1285-1287. doi:10.1016/s0003-9993(98)90276-3
[29] Genova A, Dix O, Saefan A, Thakur M, Hassan A. Carpal Tunnel Syndrome: A Review of Literature. Cureus. 2020;12(3):e7333. Published 2020 Mar 19. doi:10.7759/cureus.7333
[30] Ibid
[31] Yeap Loh P, Liang Yeoh W, Nakashima H, Muraki S. Impact of keyboard typing on the morphological changes of the median nerve. J Occup Health. 2017;59(5):408-417. doi:10.1539/joh.17-0058-OA
[32] Pourmemari MH, Viikari-Juntura E, Shiri R. Smoking and carpal tunnel syndrome: a meta-analysis. Muscle Nerve. 2014;49(3):345-350. doi:10.1002/mus.23922
[33] Dragan S, Șerban MC, Damian G, Buleu F, Valcovici M, Christodorescu R. Dietary Patterns and Interventions to Alleviate Chronic Pain. Nutrients. 2020;12(9):2510. Published 2020 Aug 19. doi:10.3390/nu12092510
[34] Piticchio T, Frasca F, Malandrino P, et al. Effect of gluten-free diet on autoimmune thyroiditis progression in patients with no symptoms or histology of celiac disease: a meta-analysis. Front Endocrinol (Lausanne). 2023;14:1200372. Published 2023 Jul 24. doi:10.3389/fendo.2023.1200372; Osowiecka K, Myszkowska-Ryciak J. The Influence of Nutritional Intervention in the Treatment of Hashimoto’s Thyroiditis-A Systematic Review. Nutrients. 2023;15(4):1041. Published 2023 Feb 20. doi:10.3390/nu15041041
[35] Markomanolaki ZS, Tigani X, Siamatras T, et al. Stress Management in Women with Hashimoto’s thyroiditis: A Randomized Controlled Trial. J Mol Biochem. 2019;8(1):3-12.
[36] Fernández-de-Las-Peñas C, Díaz-Rodríguez L, Salom-Moreno J, et al. Activation in the hypothalamic-pituitary-adrenocortical axis and sympathetic nervous system in women with carpal tunnel syndrome. Pain Med. 2014;15(8):1373-1378. doi:10.1111/pme.12453
[37] Sevy JO, Sina RE, Varacallo M. Carpal Tunnel Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing; October 29, 2023.; Stevens JC, Beard CM, O’Fallon WM, Kurland LT. Conditions associated with carpal tunnel syndrome. Mayo Clin Proc. 1992;67(6):541-548. doi:10.1016/s0025-6196(12)60461-3
[38] Callaghan BC, Gao L, Li Y, et al. Diabetes and obesity are the main metabolic drivers of peripheral neuropathy. Ann Clin Transl Neurol. 2018;5(4):397-405. Published 2018 Feb 14. doi:10.1002/acn3.531
[39] Nathan PA, Keniston RC, Lockwood RS, Meadows KD. Tobacco, caffeine, alcohol, and carpal tunnel syndrome in American industry. A cross-sectional study of 1464 workers. J Occup Environ Med. 1996;38(3):290-298. doi:10.1097/00043764-199603000-00015
[40] Roquelaure Y, Garlantézec R, Rousseau V, et al. Carpal tunnel syndrome and exposure to work-related biomechanical stressors and chemicals: Findings from the Constances cohort. PLoS One. 2020;15(6):e0235051. Published 2020 Jun 25. doi:10.1371/journal.pone.0235051; Huang WH, Hu CC, Yen TH, Hsu CW, Weng CH. Blood lead level: an overlooked risk of carpal tunnel syndrome in hemodialysis patients. Ren Fail. 2019;41(1):786-793. doi:10.1080/0886022X.2019.1657894
[41] Anglen J, Stayner L, Gruninger S. 0414 Cumulative mercury exposure and peripheral nerve function in a sample of U.S. dental professionals. Occupational and Environmental Medicine. 2014;71:A116.
[42] Dragan S, Șerban MC, Damian G, Buleu F, Valcovici M, Christodorescu R. Dietary Patterns and Interventions to Alleviate Chronic Pain. Nutrients. 2020;12(9):2510. Published 2020 Aug 19. doi:10.3390/nu12092510
[43] Gupta N, Arora M, Sharma R, Arora KS. Peripheral and Central Nervous System Involvement in Recently Diagnosed Cases of Hypothyroidism: An Electrophysiological Study. Ann Med Health Sci Res. 2016;6(5):261-266. doi:10.4103/amhsr.amhsr_39_16
[44] Ibid
[45] Duyff RF, Van den Bosch J, Laman DM, van Loon BJ, Linssen WH. Neuromuscular findings in thyroid dysfunction: a prospective clinical and electrodiagnostic study. J Neurol Neurosurg Psychiatry. 2000;68(6):750-755. doi:10.1136/jnnp.68.6.750
[46] Oktayoglu P, Nas K, Kilinç F, Tasdemir N, Bozkurt M, Yildiz I. Assessment of the Presence of Carpal Tunnel Syndrome in Patients with Diabetes Mellitus, Hypothyroidism and Acromegaly. J Clin Diagn Res. 2015;9(6):OC14-OC18. doi:10.7860/JCDR/2015/13149.6101
[47] Vashishtha M, Varghese B, Mosley F, Kadakia A, de Jager W. Screening for thyroid dysfunction and diabetes in patients with carpal tunnel syndrome. Surgeon. 2016;14(3):147-149. doi:10.1016/j.surge.2014.11.003
[48] PURNELL DC, DALY DD, LIPSCOMB PR. Carpal-tunnel syndrome associated with myxedema. Arch Intern Med. 1961;108:751-756. doi:10.1001/archinte.1961.03620110091012; Karne SS, Bhalerao NS. Carpal Tunnel Syndrome in Hypothyroidism. J Clin Diagn Res. 2016;10(2):OC36-OC38. doi:10.7860/JCDR/2016/16464.7316
[49] Karne SS, Bhalerao NS. Carpal Tunnel Syndrome in Hypothyroidism. J Clin Diagn Res. 2016;10(2):OC36-OC38. doi:10.7860/JCDR/2016/16464.7316; Gupta N, Arora M, Sharma R, Arora KS. Peripheral and Central Nervous System Involvement in Recently Diagnosed Cases of Hypothyroidism: An Electrophysiological Study. Ann Med Health Sci Res. 2016;6(5):261-266. doi:10.4103/amhsr.amhsr_39_16
[50] Holováčová D, Kužma M, Killinger Z, Payer J. Cross-sectional area of the median nerve is increased in primary autoimmune hypothyroidism and decreases upon treatment with thyroxine. Eur J Endocrinol. 2016;175(4):265-271. doi:10.1530/EJE-16-0397
[51] Zaid FE, Eljazwi E, Eldrasi N. Effect of L-Thyroxine Therapy on Musculoskeletal Symptoms of Hypothyroidism. Rheumatology (Sunnyvale).2015; 5 (172). doi:10.4172/2161-1149.100017
[52] Karne SS, Bhalerao NS. Carpal Tunnel Syndrome in Hypothyroidism. J Clin Diagn Res. 2016;10(2):OC36-OC38. doi:10.7860/JCDR/2016/16464.7316
[53] Kececi H, Degirmenci Y. Hormone replacement therapy in hypothyroidism and nerve conduction study. Neurophysiol Clin. 2006;36(2):79-83. doi:10.1016/j.neucli.2006.04.001
[54] Scalise V, Brindisino F, Pellicciari L, Minnucci S, Bonetti F. Carpal Tunnel Syndrome: A National Survey to Monitor Knowledge and Operating Methods. Int J Environ Res Public Health. 2021;18(4):1995. Published 2021 Feb 18. doi:10.3390/ijerph18041995
[55] Atcheson SG, Ward JR, Lowe W. Concurrent medical disease in work-related carpal tunnel syndrome. Arch Intern Med. 1998;158(14):1506-1512. doi:10.1001/archinte.158.14.1506
[56] Ibid
[57] Ellis JM. Treatment of carpal tunnel syndrome with vitamin B6. South Med J. 1987;80(7):882-884. doi:10.1097/00007611-198707000-00018
[58] Ryan-Harshman M, Aldoori W. Carpal tunnel syndrome and vitamin B6. Can Fam Physician. 2007;53(7):1161-1162.
[59] Valente R, Gibson H. Chiropractic manipulation in carpal tunnel syndrome. J Manipulative Physiol Ther. 1994;17(4):246-249.
[60] Chen P, Wang C, Ren YN, Ye ZJ, Jiang C, Wu ZB. Alterations in the gut microbiota and metabolite profiles in the context of neuropathic pain. Mol Brain. 2021;14(1):50. Published 2021 Mar 9. doi:10.1186/s13041-021-00765-y
[61] Paez-Hurtado AM, Calderon-Ospina CA, Nava-Mesa MO. Mechanisms of action of vitamin B1 (thiamine), B6 (pyridoxine), and B12 (cobalamin) in pain: a narrative review. Nutr Neurosci. 2023;26(3):235-253. doi:10.1080/1028415X.2022.2034242
[62] Julian T, Syeed R, Glascow N, et al. B12 as a treatment for peripheral neuropathic pain: a systematic review. Nutrients. 2020 Jul 25;12(8):2221.; Kalita J, Chandra S, Bhoi SK, et al. Clinical, nerve conduction and nerve biopsy study in vitamin B12 deficiency neurological syndrome with a short-term follow-up. Nutr Neurosci. 2014 Jul;17(4):156-63.
[63] Di Geronimo G, Caccese AF, Caruso L, Soldati A, Passaretti U. Treatment of carpal tunnel syndrome with alpha-lipoic acid. Eur Rev Med Pharmacol Sci. 2009;13(2):133-139.
[64] Pajardi G, Bortot P, Ponti V, Novelli C. Clinical usefulness of oral supplementation with alpha-lipoic Acid, curcumin phytosome, and B-group vitamins in patients with carpal tunnel syndrome undergoing surgical treatment. Evid Based Complement Alternat Med. 2014;2014:891310. doi:10.1155/2014/891310
[65] Abdul-Razzak KK, Kofahi RM. Carpel tunnel syndrome: A link with vitamin D and calcium. Biomed Rep. 2020;13(3):15.
[66] Alam U, Petropoulos IN, Ponirakis G, et al. Vitamin D deficiency is associated with painful diabetic neuropathy. Diabetes Metab Res Rev. 2021;37(1):e3361. doi:10.1002/dmrr.3361
[67] Shin HJ, Na HS, Do SH. Magnesium and Pain. Nutrients. 2020;12(8):2184. Published 2020 Jul 23. doi:10.3390/nu12082184 .
[68] Maroon JC, Bost JW. Omega-3 fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain. Surg Neurol. 2006;65(4):326-331. doi:10.1016/j.surneu.2005.10.023
[69] LeBlanc JG, Milani C, de Giori GS, Sesma F, van Sinderen D, Ventura M. Bacteria as vitamin suppliers to their host: a gut microbiota perspective. Curr Opin Biotechnol. 2013;24(2):160-168. doi:10.1016/j.copbio.2012.08.005
[70] Maddali Bongi S, Signorini M, Bassetti M, Del Rosso A, Orlandi M, De Scisciolo G. A manual therapy intervention improves symptoms in patients with carpal tunnel syndrome: a pilot study. Rheumatol Int. 2013;33(5):1233-1241. doi:10.1007/s00296-012-2507-0
[71] Carlson H, Colbert A, Frydl J, Arnall E, Elliot M, Carlson N. Current options for nonsurgical management of carpal tunnel syndrome. Int J Clin Rheumtol. 2010;5(1):129-142. doi:10.2217/IJR.09.63
[72] Bahrami-Taghanaki H, Azizi H, Hasanabadi H, et al. Acupuncture for Carpal Tunnel Syndrome: A Randomized Controlled Trial Studying Changes in Clinical Symptoms and Electrodiagnostic Tests. Altern Ther Health Med. 2020;26(2):10-16.
[73] Hadianfard M, Bazrafshan E, Momeninejad H, Jahani N. Efficacies of Acupuncture and Anti-inflammatory Treatment for Carpal Tunnel Syndrome. J Acupunct Meridian Stud. 2015;8(5):229-235. doi:10.1016/j.jams.2014.11.005
[74] Rowin J. Integrative neuromuscular medicine: neuropathy and neuropathic pain: consider the alternatives. Muscle Nerve. 2019 Aug;60(2):124-136.
[75] Muller M, Tsui D, Schnurr R, et al. Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004 Apr-Jun;17(2):210-28.
[76] Jeffrey SL, Belcher HJ. Use of Arnica to relieve pain after carpal-tunnel release surgery. Altern Ther Health Med. 2002;8(2):66-68.; Widrig R, Suter A, Saller R, Melzer J. Choosing between NSAID and arnica for topical treatment of hand osteoarthritis in a randomised, double-blind study. Rheumatol Int. 2007;27(6):585-591. doi:10.1007/s00296-007-0304-y
[77] Fusakul Y, Aranyavalai T, Saensri P, Thiengwittayaporn S. Low-level laser therapy with a wrist splint to treat carpal tunnel syndrome: a double-blinded randomized controlled trial. Lasers Med Sci. 2014;29(3):1279-1287. doi:10.1007/s10103-014-1527-2
[78] Li ZJ, Wang Y, Zhang HF, Ma XL, Tian P, Huang Y. Effectiveness of low-level laser on carpal tunnel syndrome: A meta-analysis of previously reported randomized trials. Medicine (Baltimore). 2016;95(31):e4424. doi:10.1097/MD.0000000000004424
[79] Güven SC, Özçakar L, Kaymak B, Kara M, Akıncı A. Short-term effectiveness of platelet-rich plasma in carpal tunnel syndrome: A controlled study. J Tissue Eng Regen Med. 2019;13(5):709-714. doi:10.1002/term.2815
[80] Catapano M, Catapano J, Borschel G, Alavinia SM, Robinson LR, Mittal N. Effectiveness of Platelet-Rich Plasma Injections for Nonsurgical Management of Carpal Tunnel Syndrome: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Arch Phys Med Rehabil. 2020;101(5):897-906. doi:10.1016/j.apmr.2019.10.193
[81] Epstein J, Sanderson IR, Macdonald TT. Curcumin as a therapeutic agent: the evidence from in vitro, animal and human studies. Br J Nutr. 2010;103(11):1545-1557. doi:10.1017/S0007114509993667; Pajardi G, Bortot P, Ponti V, Novelli C. Clinical usefulness of oral supplementation with alpha-lipoic Acid, curcumin phytosome, and B-group vitamins in patients with carpal tunnel syndrome undergoing surgical treatment. Evid Based Complement Alternat Med. 2014;2014:891310. doi:10.1155/2014/891310
[82] Karimi M, Rohani S, Akbari MG, Kargozar E, et al. The Efficacy of Boswellia carterii Oleogel in Pain Relief and Functional Improvement Among Patients with Carpal Tunnel Syndrome: A Triple-Blind Randomized, Controlled Trial. Shiraz E-Medical Journal. In Press. January 2021. 10.5812/semj.107952. ResearchGate. Accessed December 3, 2024.
[83] Hashempur MH, Lari ZN, Ghoreishi PS, et al. A pilot randomized double-blind placebo-controlled trial on topical chamomile (Matricaria chamomilla L.) oil for severe carpal tunnel syndrome. Complement Ther Clin Pract. 2015;21(4):223-228. doi:10.1016/j.ctcp.2015.08.001; Hashempur MH, Ghasemi MS, Daneshfard B, et al. Efficacy of topical chamomile oil for mild and moderate carpal tunnel syndrome: A randomized double-blind placebo-controlled clinical trial. Complement Ther Clin Pract. 2017;26:61-67. doi:10.1016/j.ctcp.2016.11.010
[84] Xu DH, Cullen BD, Tang M, Fang Y. The Effectiveness of Topical Cannabidiol Oil in Symptomatic Relief of Peripheral Neuropathy of the Lower Extremities. Curr Pharm Biotechnol. 2020;21(5):390-402. doi:10.2174/1389201020666191202111534
[85] Nordio M, Basciani S. Efficacy of a food supplement in patients with hashimoto thyroiditis. J Biol Regul Homeost Agents. 2015;29(1):93-102.
[86] Žídková V, Nakládalová M, Štěpánek L. Effects of Exercise and Enzyme Therapy in Early Occupational Carpal Tunnel Syndrome: A Preliminary Study. Biomed Res Int. 2019;2019:8720493. Published 2019 Jan 23. doi:10.1155/2019/8720493

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Leave a Reply