Histamine is such a fascinating chemical, and I feel like my knowledge and appreciation for histamine is ever-evolving! As a young pharmacy technician, I was excited to learn about antihistamines, and their effects on allergies.
Then in pharmacy school, I learned about how psychiatric medications have histamine-blocking properties as well. Additionally, I had the rare honor of doing a rotation at the Pfeiffer Treatment Center under Dr. William Walsh in my early twenties, where I learned about ortho molecular medicine and two seldom known biochemical imbalances: histapenia (not enough histamine) and histadelia (too much histamine), both of which can present as psychiatric issues. The protocols employed by the clinic focused on modulating histamine levels to produce health transformations.
As time went on, and I got into functional medicine, I began to have a few clients with histamine issues. I had a pretty straightforward (or so I thought) approach to addressing histamines, but I guess I was meant to learn more about it. 🙂
By chance, I met the late Yasmina of Healing Histamine and began to appreciate histamine intolerance a bit more. Since that time, I have had a recent personal connection with histamine issues – with my own little son, who had eczema, frequent night wakings, poor appetite, and other signs of histamine intolerance when he was a toddler.
They say that children are our greatest teachers, and I think that’s so true. Thanks to a few wonderful pediatric specialists – Dr. Sheila Kilbane, Deborah Allen, RPh, Dr. Erica Peirson, Dr. Pejman Katiraei, as well as Michael McEvoy (a functional diagnostic nutritionist with a brilliant training for clinicians) – I got to learn so much about addressing histamine issues. And then I found my old notes on modulating histamine from my clinical rotations, and was able to finally make sense of them! Thus, this article was due for an update, as it was initially published in 2019. 🙂
Many readers in my community report symptoms of histamine intolerance, which can be challenging to differentiate from other food sensitivities and imbalances in the digestive system. The good news is that many seemingly different symptoms will have the same root causes.
When we get to the root, whole-body healing can happen.
At the beginning of my healing journey with Hashimoto’s, I experienced many allergies and sensitivities. It truly felt like I was allergic to everything, including all of the trees and bushes in California, as well as my sweet dog!
Reacting to my environment and food, as well as having other symptoms of Hashimoto’s (like brain fog, hair loss, fatigue, and anxiety), was overwhelming, to say the least. It took me some time to sort everything out and get to my root causes. My hope is that this article provides you with helpful information, clarity, and next steps in your own journey of discovery.
In this article, you’ll discover:
- What histamine is, and what it means to have an intolerance
- What DAO is, and how it relates to histamine
- How histamine acts as a neurotransmitter
- Potential causes of histamine intolerance
- Testing strategies for histamine intolerance
- The histamine and thyroid connection
- Histamine intolerance treatments
What is Histamine?
Histamine is an important chemical in the immune system that is released by cells during hypersensitivity or inflammatory reactions. [1] In simple terms, when your body is exposed to a reactive compound, histamine increases and turns on inflammatory processes in order to protect the body from that compound. Histamine causes the contraction of smooth muscles and the dilation of blood vessels, which allow immune cells to travel to the site of the perceived attack. In normal amounts in the body, histamine helps with circulation, attention, and digestion, and is also considered a neurotransmitter.
Your body cells make histamine, as do certain bacteria and yeast in your digestive tract, and it is also found in some foods.
Histamine is associated with allergic or sensitivity reactions. In the springtime, when pollen comes out, many people experience watery eyes, a runny nose, and itchy skin. This is a histamine reaction. You’ve likely heard of antihistamine medications or supplements designed to dampen this type of reaction.
What is Histamine Intolerance?
Simply put, histamine intolerance occurs when there is an imbalance between the amount of histamine produced in the body, versus the body’s ability to break it down. This histamine overload results in symptoms. I personally believe that histamine overload is the more correct term, but “histamine intolerance” is the term currently used.
The body produces histamine on its own, but histamine can also be ingested or produced through the food we eat. Unlike a true allergy, histamine intolerance may not be an immediate reaction.
I used to think that this was due to not having enough DAO enzymes to balance the levels of histamine in the digestive system, but there’s actually more to the equation than that. Notably, excess histamine-producing microbes and a deficiency in vitamin B6, which is an important co-factor in breaking down histamine properly, are two causes that can be at the root of histamine build up, rather than a sensitivity to histamine-containing foods.
Symptoms of Histamine Intolerance
Symptoms of histamine intolerance are widespread and may be non-specific, making histamine intolerance difficult to diagnose. Often, histamine intolerance may be mistaken for (or overlap with) a food allergy, food sensitivity, mast cell disorder, and other diagnoses.
Individuals with histamine intolerance may experience some of the symptoms listed below, but not others. Bloating may be the most common symptom, along with fullness after a meal, diarrhea, abdominal pain, and constipation. These symptoms may be similar to symptoms of SIBO.
Common Histamine Intolerance Symptoms
- Stomach pain, cramping
- Nausea, vomiting
- Diarrhea, constipation
- Headaches and migraines
- Low blood pressure
- Heart arrhythmia
- Hives, itching, flushing
- Runny nose
- Swelling in the face, mouth or throat
- Asthma
- Fatigue
- Dysmenorrhea (menstrual cramping)
Histamine as a Neurotransmitter
The other day, I was helping someone who has a child with allergies, eczema, asthma, digestive distress, as well as behavioral issues. “What’s the connection?” she wondered. To that I said, “histamine”.
One thing about histamine that not many people know is that it functions as a neuromodulator, meaning that it regulates the release of neurotransmitters typically associated with mood, like serotonin, dopamine, and norepinephrine. It may increase dopamine, norepinephrine, and glutamate, while decreasing serotonin levels.
Histamine can also act as an excitatory neurotransmitter, which means it can affect the sleep-wake cycle and mood; it has also been linked to anger and aggression. [2]
While people typically associate histamine with allergies, histamine can also have an impact on the digestive tract as well as our brain.
There are several different histamine receptors, known as H1, H2, H3, and H4 receptors. H1 and H4 receptors are associated with seasonal allergies and symptoms like wheezing, asthma, itching, and bronchial restriction. H2 receptors are connected to a cell-mediated inflammatory response and the gut (hello acid reflux), while H3 receptors are connected to the central nervous system and neurotransmitters.
Increased histamine in the brain inhibits the release of serotonin, which can affect our mood and lead to depression, anxiety, disrupted sleep, chronic pain, dysregulated appetite, and even constipation. [3]
Research has found that in addition to lowering serotonin levels in the brain, high histamine levels make SSRIs less effective, which is important to note for those who have treatment-resistant depression, or anyone considering getting on an SSRI. [4]
High histamine levels may also decrease methylation activity, and undermethylation can contribute to a host of symptoms such as an inability to clear out toxins, estrogen dominance, brain fog, fatigue, and anxiety. You can learn more about methylation in my article on the MTHFR gene variation.
The Ortho Molecular Approach to Histamine Intolerance
When I was a pharmacy intern at the Pfeiffer Treatment Center, a center focused on balancing biochemical imbalances that can cause mental health and developmental issues though the use of vitamins, minerals, and nutrients, one of my assignments was to review the antihistamine properties of various psychotropic drugs and provide an in-service to the staff on this topic.
I was fascinated to learn how many psychotropic medications actually suppressed blood histamine levels. Knowing what a powerful neurotransmitter histamine can be, it makes so much sense that this is their mechanism of action.
The Pfeiffer Treatment Center has an approach on addressing mental health issues through the orthomolecular approach of testing blood histamine and using natural therapies to resolve histamine issues, and the related mental health symptoms.
The Pfeiffer Treatment Protocols focus on using B6, zinc and methionine or SAMe, to clear out excess histamines (I’m excited to share that the same modified approach also works for allergic and gut-related histamine issues I see in Hashimoto’s).
The Histamine and Thyroid Connection
Those with thyroid imbalances, including Hashimoto’s, may be more susceptible to histamine intolerance. This may be because histamine intolerance and Hashimoto’s thyroiditis can share the same root causes.
What’s more, in attempts to heal the thyroid, some may inadvertently increase high histamine foods in their diet. This alone is not enough to cause a “histamine intolerance”, but can be problematic in the presence of an H. pylori or Blastocystis hominis infection (two common Hashimoto’s triggers), or when a person has mold exposure or mold colonization. People may also discover that they are unknowingly consuming substances that block DAO. I will cover each of these topics below, in the treatment section.
There is also a connection between mast cells and the thyroid. Mast cells are a type of white blood cell found throughout the body that help mediate the inflammatory response in the body, including releasing histamine. Research has found that mast cells also have the ability to synthesize and store thyroid hormones like T3 and TSH, suggesting that mast cells can modulate thyroid function, and an increase of mast cells has been observed in cases of hypothyroidism. [5]
The complex and reciprocal relationship between inflammation, histamine, and the thyroid is still being explored, and I’m excited for future research that explores this connection even more.
Causes of Histamine Intolerance
Histamine intolerance is thought to be due largely to a deficiency in DAO, and this is what I used to think as well. I used to treat histamine intolerance primarily by recommending someone go on a low histamine diet and supplement with DAO enzymes. While this can still be part of the overall approach to histamine intolerance, it rarely gets to the root cause.
My histamine protocols have evolved over the years, and I’ve been fortunate to work with many experts and clients who have expanded my views and knowledge on histamine.
In my experience, I have learned that the following can be reversible causes of histamine intolerance:
- Gut imbalances (including dysbiosis, bacterial overgrowth of pathogenic gut microbes, including SIBO, H. pylori, Candida, and parasitic infections like Blastocystis hominis and Dientamoeba fragilis)
- Mold exposure
- P5P deficiency
- Zinc deficiency
- Methylation issues
- Estrogen dominance
In my evolved approach (that has come full circle thanks to finding my notes from the Pfeiffer Treatment Center a few years ago), I now recommend P5P and zinc to balance histamine levels as a starting point (as they are both needed to break down histamine), followed by methylation support (the Pfeiffer Treatment Center used B6 and zinc, plus methionine or SAMe; I use B2, methylfolate, and methionine), while doing some root cause investigation.
It’s funny, because I had learned about this approach as a student, but did not have much understanding of how or even why to use it. I had to have a lot more experience and much more context to make it applicable.
This approach makes a lot of sense, as P5P, the metabolically active form of vitamin B6, is low in those with histamine intolerance, and it’s necessary for the breakdown of histamine. [6]
Zinc helps to stabilize mast cells, making it an important nutrient for those with histamine issues. [7]
SAMe (S-adenosylmethionine or S-adenosyl-L-methionine) is your body’s main methyl donor. SAMe is a cofactor for the HNMT enzyme, which is necessary for the breakdown of histamine. [8] Methionine is the precursor to SAMe and it also has benefits on gut health, while people with bipolar disorder should not take SAMe except under the supervision of a health care provider, as SAMe may worsen symptoms of mania. [9]
I have been fascinated by how well this approach works, and also a little bit embarrassed that it took so long for me to make this connection, having learned this protocol back in 2005/2006 during pharmacy school rotations!
Simultaneously, I prefer to test, whenever possible, to determine a root cause of histamine intolerance.
Histamine and the Gut
There are certain gut microbes that can potentially produce histamine, including Blastocystis hominis, H. pylori, Dientamoeba fragilis, as well as certain dysbiotic bacteria. [10]
Other types of bacteria that can potentially produce histamine in the gut include: [11]
- Lactobacillus (especially in SIBO)
- Morganella
- Pseudomonas
- Pseudomonas aeruginosa
- Citrobacter freundii
- Klebsiella
- Klebsiella pneumoniae
- Proteus
- Proteus mirabilis
- Enterobacter
- Escherichia
- Fusobacterium
This is why if you’re experiencing symptoms of histamine intolerance, I would suggest doing a GI-MAP, which can help you identify whether you have H. pylori, histamine producing-protozoa, or high levels of histamine-causing bacteria in your gut. Additionally, a test for SIBO may be helpful.
Candida
When Candida grows in the gut, it releases histamine, while at the same time reducing the amount of DAO, which is needed to break down histamine. [12]Candida also releases mycotoxins, and the body can release histamine in response to these toxins (more on mold in the next section). [13]
Not surprisingly, many symptoms of histamine intolerance overlap with those of a Candida infection.
If you have Candida overgrowth, treating the Candida can often result in a relief of symptoms and lower histamine levels.
You can test for Candida through a stool test like the GI-MAP. I also recommend checking out my article to learn more about treating Candida.
Mold Exposure
Exposure to mold can cause mast cells to release histamine, in order to attack toxic mold organisms. [14] If the appearance of your symptoms line up with moving into a new home, or following water damage to your home, or perhaps you seem to feel better when you are on vacation, there’s a good chance mold may be connected to your symptoms.
I recommend testing to give you a better picture of mold toxicity. I like either the MycoTOX test or the Organic Acids Test.
Nutrient Deficiencies
The top nutrients I look at when addressing histamine intolerance are vitamin B6, specifically the P5P form, and zinc. P5P is the metabolically active form of vitamin B6, and has been found to be low in those with histamine intolerance. It’s a necessary cofactor for the breakdown of histamine. [15] Zinc is also needed for the breakdown of histamine, and also helps to stabilize mast cells. [16] I’ve found that ensuring someone has adequate levels of these two nutrients is an important part of treating histamine intolerance. I list my recommended brands and dosages in the Root Cause Approach section below.
Methylation
Undermethylation is often thought to be the result of the MTHFR gene variation, but there are conditions that can increase our methylation requirements as well, such as toxic exposure. Many toxins (including mold) and hormones (including estrogen) are removed via methylation.
Undermethylation can also lead to dysregulated neurotransmitter activity. Common symptoms of undermethylation include perfectionism, a history of high achievement, obsessive compulsive tendencies, and ritualistic behaviors. [17] (Also known as my entire childhood and my early twenties, or me before I started taking methylfolate supplements.)
This gene variation is actually fairly common, with at least 50 percent of Americans having some degree of methylation gene alterations. When it comes to histamine, this process of methylation is essential for clearing histamine from the body, and when someone has impaired methylation, histamine can build up and cause issues.
The Estrogen Connection
Estrogen down-regulates the DAO enzyme, which we know we need to clear histamines, and at the same time, it stimulates mast cells to release histamine. [18] Histamine stimulates the ovaries to make more estrogen, which can then lead to a vicious cycle where estrogen and histamine perpetuate one another. [19]
On the other hand, progesterone stabilizes mast cells and up-regulates DAO, meaning it can reduce histamine. This is why women with histamine intolerance may see changes in their histamine symptoms fluctuating with their menstrual cycle, and women in perimenopause often see histamine issues worsened or exacerbated as progesterone levels drop (a few weeks ago, I wrote about increasing progesterone naturally).
Understanding estrogen’s role in histamine, it makes sense that estrogen dominance could be a factor in exacerbating histamine intolerance symptoms. That said, some of the drivers of histamine intolerance (such as mold exposure and colonization), may also be drivers of estrogen dominance. All that to say, addressing estrogen dominance can help with histamine issues and vice versa (and treating the cause of both is always key).
What About Histamine Overload from Diet & Supplements?
Sometimes, people on a healing diet may inadvertently add high histamine foods into their diet. Avocado is a good example – it’s a great source of fiber and healthy fats, but it also happens to be high in histamine.
Avoiding high histamine foods may be helpful for reducing symptoms of histamine intolerance while the other root causes are addressed. As the gut heals and other triggers are removed, it is likely that these foods will be able to be introduced again at some point, with better tolerance.
One study showed that a low histamine diet can increase the body’s own production of DAO. [20]
Another study showed that either boiling plant foods or ensuring maximum freshness of foods, can lower one’s histamine reaction. [21] This is because as foods age and ferment, bacteria on the foods can release more histamine. This is one reason that you may not have a reaction to a fresh cooked meal, but you do experience a reaction to the leftovers a couple days later. This is why I recommend avoiding leftovers as part of your low-histamine diet.
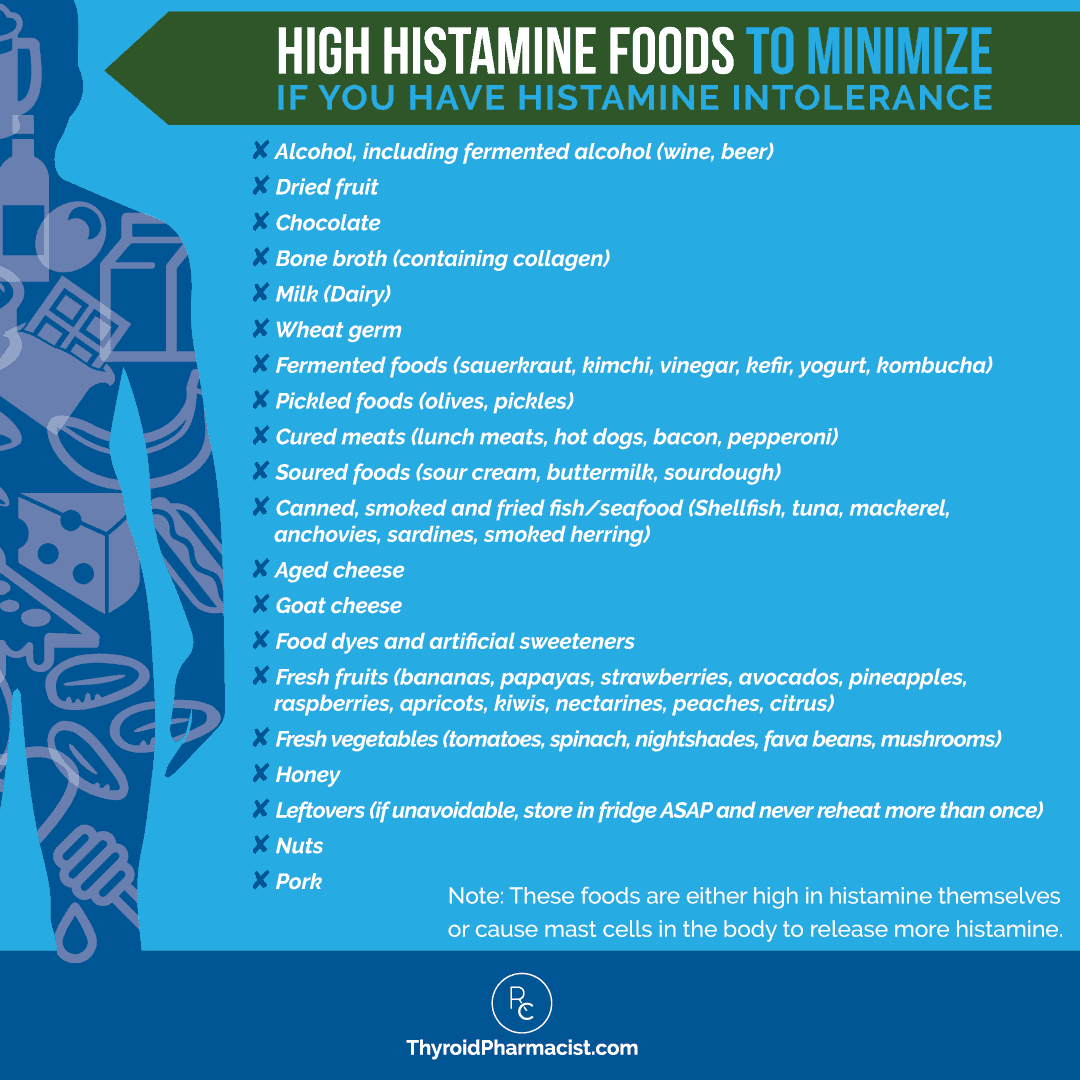
The following food lists can provide guidance for a starting point. Consider eliminating the high histamine foods for a period of 30 days, and then begin to slowly reintroduce foods. The process is the same as my elimination diet; however, the food lists are different.
How to Do an Elimination Diet with High Histamine Foods
An elimination diet requires you to remove the most common food sensitivities from your diet, for a period of three weeks. It is imperative during this time that you do not “cheat” at all by eating even a small amount of any of the foods that have been removed. Doing so could cause a reaction and interfere with your results.
There are three important steps to the elimination diet:
- Decide which foods you are going to eliminate. If you are looking to identify and heal from histamine intolerance, you will need to avoid all foods that are high in histamine. See the food list below.
- Avoid the foods you are eliminating. This step is crucial! Again, even the smallest amount of a food that you are avoiding could cause a reaction, so it is important that you are vigilant and avoid all traces of the food for three weeks. Check food labels carefully, and be extra careful if you are eating out, as it’s difficult to know all of the ingredients used in restaurants. It may be best to avoid eating out during this elimination period, to avoid any cross-contamination that might skew your results. Additionally, you’ll want to avoid leftovers! Leftover food is high in histamines because the histamine content of cooked foods increases as it sits in the fridge. As much as possible, prepare your meals fresh.
- Reintroduce the challenged foods. If your symptoms have improved after 30 days, you can start adding the foods back in, one at a time. Paying attention to any reactions you may have to particular foods, will help you identify your personal food sensitivities.
High Histamine Foods to Minimize
These foods are either high in histamine themselves, or cause mast cells in the body to release more histamine:
- Alcohol, including fermented alcohol (wine, beer)
- Dried fruit
- Chocolate
- Bone broth (containing collagen)
- Milk (dairy)
- Wheat germ
- Fermented foods (sauerkraut, kimchi, vinegar, kefir, yogurt, kombucha)
- Pickled foods (olives, pickles)
- Cured meats (lunch meats, hot dogs, bacon, pepperoni)
- Soured foods (sour cream, buttermilk, sourdough)
- Canned, smoked and fried fish/seafood (shellfish, tuna, mackerel, anchovies, sardines, smoked herring)
- Aged cheese
- Goat cheese
- Food dyes and artificial sweeteners
- Fresh fruits (bananas, papayas, strawberries, avocados, pineapples, raspberries, apricots, kiwis, nectarines, peaches, citrus)
- Fresh vegetables (tomatoes, spinach, nightshades, fava beans, mushrooms)
- Honey
- Leftovers (best to avoid altogether, but make sure cooked foods are cooled rapidly and put right into the refrigerator; never reheat more than once)
- Nuts
- Pork
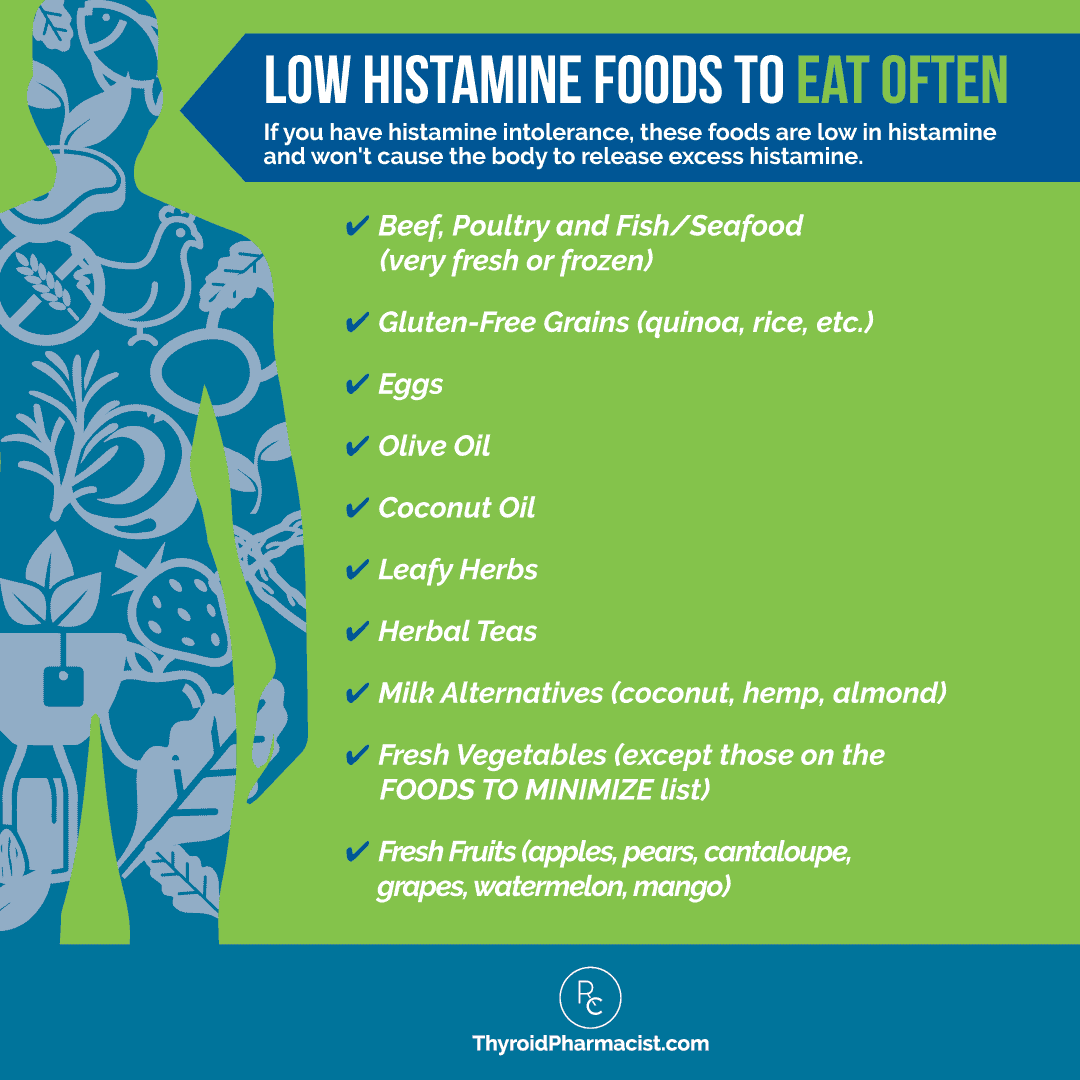
Low Histamine Foods to Eat Often
- Beef, poultry and fish/seafood (very fresh or frozen)
- Gluten-free grains (quinoa, rice, etc.)
- Eggs
- Olive oil
- Coconut oil
- Leafy herbs
- Herbal teas
- Milk alternatives (coconut, hemp, almond)
- Fresh vegetables (except those listed as AVOID)
- Fresh fruits (apples, pears, cantaloupe, grapes, watermelon, mango)
How to Make Bone Broth Low in Histamines
Bone broth is known for its healing properties, and I love to recommend it to my readers to support gut health. But for those with histamine issues, it can actually make them feel worse because of its high histamine content! This is due in large part to the long cooking time of bone broth (sometimes as long as 24 hours). To reduce the histamine content and still receive the nutrients that bone broth has to offer, you can cook the bone broth for a shorter amount of time – usually about two hours. You can simply reduce the cooking time on my bone broth recipe, use a pressure cooker, or use this Instant Pot recipe by my friend Dr. Kellyann Petrucci.
Avoid DAO Blockers and Histamine Producers
It’s also important to be aware of foods and medications that act as DAO “blockers”, and some may act as histamine producers.
Alcohol and tea (green and black tea) may block DAO from doing its job to break down histamine. Avoiding these in one’s diet may be a helpful part of improving tolerance to histamine.
Certain medications also release histamine or block DAO. These may include: muscle relaxants, narcotics, pain medications (NSAIDs), antihypertensives, antiarrhythmics, diuretics, drugs that speed up gut motility, antibiotics, antidepressants, and others. If you are suffering from symptoms of histamine intolerance, it may be helpful to review medications with your provider and pharmacist.
Lastly, many people take probiotics in an effort to improve gut health, but there are certain probiotics that can actually produce histamine, undermining our efforts to feel better. These strains include Lactobacillus casei, Lactobacillus bulgaricus, and Lactobacillus reuteri. [22]
Diagnosis and Testing
The three tests that I routinely recommend for those exhibiting potential histamine issues, that can help us pinpoint the root cause, include:
- GI-MAP – Since histamine issues often originate in the gut, the GI-MAP can provide insight into levels of microbes that may be producing excess histamine.
- Organic Acids Test – This test can provide insight into methylation defects, including low B2 or low B6, mold colonization, inflammation levels in the body, root causes for that inflammation, and other markers that could indicate high histamine levels in the body.
- MycoTOX – Since exposure to mold can cause mast cells to release histamine, I also recommend this test that measures levels of various molds that have colonized the body.
Testing and diagnosis for histamine intolerance itself is emerging.
Currently, some functional and naturopathic doctors test for blood levels of DAO as an indicator of the body’s ability to break down histamine.
Urine histamine testing is also being developed and implemented as a new, and likely much easier, testing option. [23]
A whole blood histamine test can measure levels of both intracellular and extracellular blood histamine levels. Levels should be between 40 and 70 ng/mL, with levels over 70 indicating undermethylation, or poor breakdown of histamines. DHA Laboratory has a whole blood histamine test.
However, these tests may still not be widely available.
Genetic testing may also be helpful. Looking for SNPs (single nucleotide polymorphisms) in the genes that code for the DAO and HNMT enzymes, can often provide a piece of the puzzle.
Dr. Sheila Kilbane also likes to do a full iron panel, because excess histamine means your body probably isn’t absorbing iron as effectively as it should be.
Conventional Treatments – Antihistamines
The conventional approach to treating histamine intolerance, often looks toward medications such as antihistamines. If you have seasonal allergies, you might already be inclined to reach for antihistamines, because symptoms can be similar.
You’re likely familiar with over-the-counter options like Benadryl, Claritin, Zyrtec, and Pepcid. These medications can suppress histamine levels in the blood temporarily, typically for 1-4 weeks after use.
The upside to antihistamines might be some momentary relief. However, I don’t think using them is the best long-term solution.
Not only can some antihistamines decrease DAO production in the body in the long term, but they also don’t address the root cause.
Furthermore, many of them tend to have side effects like fatigue, dry mouth, and constipation, which are never fun. 😉
Benadryl, in particular, also has anticholinergic activity that can interfere with our memory, and long-term use has been linked to an increased risk of dementia, and it is a notorious drug on the Beers’ list of medications that should be avoided in the elderly, due to excess risks. [24]
Therefore, they’re not the most effective solution in the long run.
As a pharmacist, a big eye-opening perspective on histamine intolerance for me was the role of psychiatric medications with histamine activity in people who have histamine-induced “psychiatric issues.”
People are often aware that they receive antihistamine medications for their “allergies”, but may not be aware their reflux medications are also antihistamines (some work on histamine 2 receptors, H2 blockers); and most don’t know that their psychotropic medications have strong antihistamine properties.
Here’s a list of psychiatric medications with antihistamine properties that I helped to compile.
| Medication Classification | Medications |
| Selective Serotonin Reuptake Inhibitors | Prozac (fluoxetine), Paxil (paroxetine), Zoloft (sertraline), Luvox (fluvoxamine), Celexa (citalopram) |
| MAO Inhibitors | Parnate (tranylcypromine), Nardil (phenelzine) |
| Phenothiazines | Compazine (prochlorperazine), Etrafon (perphenazine), Mellaril (thioridazine), Prolixin (fluphenazine), Serentil (mesoridazine), Stelazine (trifluoperazine), Thorazine (chlorpromazine), Trilafon (perphenazine) |
| Anti-Psychotics | Haldol (haloperidol), Loxitane (loxapine), Moban (molindone), Navane (thiothixene), Orap (pimozide), Risperdal (risperidone), Zyprexa (olanzapine), Seroquel (quetiapine) |
| Benzodiazepines | Ativan (lorazepam), Librax (chlordiazepoxide), Librium (chlordiazepoxide), Limbitrol (chlordiazepoxide/amitriptyline), Serax (oxazepam), Tranxene (clorazepate), Valium (diazepam), Xanax (alprazolam) |
| Tricyclics | Ascendin (amoxapine), Elavil (amitriptyline), Etrafon (perphenazine), Limbitrol (amitriptyline, chlordiazepoxide), Norpramin (desipramine), Pamelor (nortriptyline), Sinequan (doxepin), Surmontil (trimipramine), Tofranil (imipramine), Triavil (amitriptyline/perphenazine), Vivactil (protriptyline) |
| Anti-Mania Agents | Depakote (divalproex sodium), Eskalith (lithium carbonate), Lithobid (lithium, Lamictal (lamotrigine), Neurontin (gabapentin), Tegretol (carbamazepine), Topamax (topiramate) |
| Anti-Anxiety Agents | Klonopin (clonazepam), Paxil (paroxetine), Xanax (alprazolam), Zoloft (sertraline) |
I am not suggesting that every person with psychiatric issues can come off their medications simply by addressing histamine levels, but I do think that it’s worth investigating further.
The Root Cause Approach
As you know, I love digging deeper and looking at the root cause of issues. I find this to be the most reliable way to promote healing and create long-term health changes.
My histamine protocols have really evolved over the years. As I mentioned already, I used to primarily focus on a low histamine diet and DAO enzymes. These can still be part of the overall approach, but I see them as symptom management strategies, rather than root cause medicine.
I do prefer to test, whenever testing is available, to find and treat the cause. As mentioned, I like the GI-MAP, Organic Acids, and MycoTOX tests.
Now, I focus on P5P and zinc to balance histamine levels, followed by methylation support (B2, methylfolate, and methionine). Additionally, sometimes I may recommend DAO enzymes as needed, with food.
- P5P (B6) – This is an important cofactor for breaking down histamines. A deficiency in vitamin B6 may result in histamine intolerance. The recommended dosage is 1 capsule per day at breakfast, of Rootcology P5P.
- Zinc – Zinc assists in the breakdown of histamine. I recommend 30 mg of Pure Encapsulations zinc picolinate. Please note that I don’t recommend taking more than 30 mg per day unless under the supervision of a doctor.
- Methyl donors – The Pfeiffer Treatment Center preferred methionine or SAMe as methyl donors. While both can be used on their own, I generally prefer to use methionine in combination products that also supply additional benefits. A couple that I like include:
- Liver and Gallbladder Support – This comprehensive supplement contains L-methionine, vitamin A, vitamin B6, vitamin B12, milk thistle, taurine, inositol, ox bile, artichoke, and beet. By supporting bile production, this combination of ingredients can also help clear out pathogenic microbes like H. pylori, Candida, and mold. It offers support during times of GI distress, and is especially helpful for those who need additional liver and gallbladder support. It is not for those with a history of Addison’s, electrolyte imbalance, diuretic use, or steroid medication use.
- HP Restore – In addition to methylmethionine, HP Restore contains vitamin C, zinc, mastic gum, and deglycyrrhizinated licorice root, to support a healthy gastric microbial balance and help maintain a healthy gastric lining, further supporting the clearing of histamine-producing microbes such as H. pylori. The recommended dosage is 2 capsules, twice a day, with meals.
Additional Things That May Help While Searching for the Root Cause
Histamine intolerance isn’t a new condition, but awareness has been rising, and treatment options are still evolving as more and more doctors and practitioners are becoming aware of it. Here I’d like to cover some additional perspectives and approaches to the treatment of high histamine levels that perhaps may help while searching for the root cause or if you can’t tolerate the supplements I mentioned above.
These are the steps that I used to recommend to address histamine intolerance, and are very helpful for many people in improving symptoms. They can also help reduce the amount of histamine in one’s bucket. 🙂
1. Remove gluten.
When treating the root cause of Hashimoto’s, a gluten-free trial is well warranted because of the connections between gluten-sensitivity and thyroid health. [25] When talking about Hashimoto’s and histamine intolerance, we can often see even more of a connection. In those with non-celiac gluten sensitivity, it is possible that gluten is reducing DAO production in the gut, and removing gluten may be a simple root cause solution. [26]
Once gluten is removed from the diet, the intestines can begin to heal and DAO production will increase, allowing histamine to be broken down and better eliminated. I have seen the removal of gluten to be the most effective strategy to relieve many of the symptoms associated with Hashiomoto’s, including histamine intolerance and similar food sensitivities, in my clients.
2. Address intestinal permeability (and check for SIBO).
Groundbreaking research done by Fasano and colleagues, found that all cases of autoimmunity have some degree of intestinal permeability (commonly referred to as “leaky gut,” though if you use that term with a conventionally-trained physician, he/she may look at you like you have three heads!), a genetic predisposition, and a triggering event. [27]
Zonulin is a protein that is released in excess when the gut becomes permeable. This can now be measured — although I don’t often test this clinically, as the cut-off range can be misleading in my opinion. Additionally, most people with Hashimoto’s who are not in remission, will have a leaky gut.
However, this test is often super relevant in research studies. A 2018 study showed elevated levels of zonulin and dysbiosis (bacterial imbalances in the gut) in people with histamine intolerance. [28]
So, healing intestinal permeability not only addresses histamine intolerance, but helps to heal the root cause of Hashimoto’s as well.
Another important root cause of intestinal permeability and digestive symptoms is SIBO, or small intestinal bacterial overgrowth. This generally means that bacteria from the large intestine have migrated up in the small intestine. The bacteria may ferment foods there, and that may cause gas, bloating, and indigestion. [29] SIBO is known to be a potent cause of leaky gut.
Up to 50 percent of people with Hashimoto’s may have SIBO, possibly due to low thyroid hormone that slows down movement through the digestive system, among other factors. [30]
Hypothyroidism, slowed motility, and SIBO seem to fuel one another, and some practitioners who specialize in SIBO think that hypothyroidism is the trigger for SIBO… while others like yours truly, believe that SIBO triggers hypothyroidism though the autoimmune/leaky gut mechanism. Both scenarios are possible. 🙂
Since certain species of bacteria can be histamine producers, SIBO can exacerbate the amount of histamine in the gut and increase the need for DAO production. What’s more, since the gut may be leaky, this histamine has an easier time making it into the body, where it can cause a host of uncomfortable symptoms.
Addressing the microbial imbalances and restoring the integrity of the gut lining, may have a profound impact on one’s ability to tolerate histamine again. It may also increase DAO production.
Finally, “healing the gut” is a term that is widely thrown out into the blogosphere by natural health advocates, and one may think that all is required is eliminating a few foods, taking probiotics, and perhaps some bone broth. While these three things can be helpful, I want to be sure to stress that there are multiple causes of intestinal permeability (not just food sensitivities, dysbiosis, or a “bone broth” deficiency). Furthermore, certain probiotics and bone broth may make histamine issues worse in the short term!
In my experience, elimination diets can help the symptoms, but don’t usually heal most cases of leaky gut. With a few important exceptions (gluten, dairy, and potentially soy), food sensitivities are a symptom, not a cause, of leaky gut.
I’ve seen that people who have chemical sensitivities/multiple allergies, as well as histamine intolerance, often do really well with my liver protocol (or something similar) before diving into a gut support protocol like the one I outlined in Hashimoto’s Protocol, with modifications to avoid consuming high histamine foods (bone broth and fermented veggies, which are typically great for supporting the gut, are both high histamine foods).
3. Test for IgE allergies and avoid them.
IgE allergies are known as “true allergies” (though I always think this terminology is misleading). They can cause symptoms like wheezing, shortness of breath, and skin reactions. Symptoms are going to be more immediate (minutes) when compared to food sensitivities that are often delayed (hours to days). People with IgE food allergies often have an impaired capacity to break down histamine in the digestive system, so if someone is continually eating a food they are allergic to, it could be the cause of the increased histamine. [31]
The most common IgE food allergens are milk, egg, soy, wheat, peanuts, tree nuts, fish, and shellfish. Other non-food IgE allergens that we commonly see include dust, pollen, animal dander, and certain types of grasses. Environmental allergies will usually cause symptoms such as sneezing and stuffy nose, while food allergies typically present with symptoms such as coughing, shortness of breath, hives, and abdominal pain.
One form of treatment for allergies is an allergy shot. It works as an immunotherapy, wherein a tiny amount of the allergen is delivered through an injection over a period of time, in order to stimulate the immune system to build a tolerance to the allergen, so that it no longer reacts. While allergy shots can be effective for people with environmental allergies, they are less effective for food allergies and are not generally recommended.
An alternative form of allergy treatment, called sublingual immunotherapy (SLIT), involves giving a patient small doses of an allergen under the tongue, to boost tolerance to the substance, and reduce symptoms. This form of allergy therapy is generally considered safe and has several published studies showing its effectiveness for a wide range of allergies. [32] An added benefit is that the patient is able to administer maintenance doses of the prescribed allergen themselves, without returning to the allergist’s office for treatments.
4. Address DAO blockers.
As mentioned, alcohol and tea (green and black tea) may block DAO from doing its job to break down histamine. Certain medications may also release histamine or block DAO.
5. Avoid high histamine foods (temporarily).
As mentioned, temporarily reducing your intake of high histamine foods can be helpful in reducing symptoms, lowering your overall histamine levels and increasing production of DAO.
6. Consider supplementing with the DAO enzyme.
DAO, or diamine oxidase, is an enzyme produced by healthy gut cells that breaks down histamine in the small intestine. [33] HNMT, or Histamine N-Methyltransferase, is another enzyme that is responsible for breaking down histamine within the rest of the body. [34] The body’s preferred state is to have a nice balance between histamine levels and DAO enzymes, in the digestive tract.
A low histamine diet combined with DAO supplementation can improve one’s symptoms and quality of life. One study found that people with migraine headaches tend to have low DAO in their blood. [35] Another study found that, for those with migraine headaches, DAO supplementation has been shown to reduce the duration of their migraine attack by 1.4 hours. [36] DAO supplementation may be effective for other symptoms as well, and is often worth a trial. Be sure to work with a practitioner to help you find a DAO supplement that works best for your needs. Seeking Health’s Histamine Digest is one option.
7. Consider vitamin C.
Vitamin C – Vitamin C can help with symptoms of histamine intolerance, especially when combined with addressing root cause factors. I recommend experimenting with supplementing between 500 and 2000 mg per day, or as recommended by your provider. While high levels of vitamin C are not likely to be harmful, some people may have less bowel tolerance and experience diarrhea at higher doses.
8. Consider natural histamines like quercetin.
Quercetin is a natural pigment that can be found in many fruits and vegetables. It is high in antioxidants and plays an important role in combating free radicals, as well as reducing inflammation, allergy symptoms, and blood pressure. [37] Animal studies have found that quercetin may block enzymes involved in inflammation, and suppress inflammation-promoting chemicals, such as histamine. [38]
Quercetin-Rich Foods That Can Be Combined with High Histamine Foods
- Fresh fruits: apples, plums, cranberries and juice, black currants, capers
- Fresh vegetables: kale, onions – all varieties, red being the highest, spinach
- Fresh herbs: tarragon, watercress, chives, coriander, lovage, dill
- Cocoa powder (raw)
HistaEze by Designs for Health is a combination product that contains quercetin, along with vitamin C, electrolytes and nettles, to help with allergies or flares. The recommended dosage is 2 capsules twice per day between meals.
Please note that quercetin has some conflicting data on it with regard to thyroid health, with a recent study showing that it could interfere with thyroid function. [39] That said, I have not seen this reaction clinically.
9. Take food as a medicinal antihistamine.
While not technically a supplement, camel milk (if well tolerated) has some interesting properties to help with healing Hashimoto’s, food sensitivities, and histamine intolerance. There is evidence to suggest it’s beneficial for immune system balance, thyroid hormone balance, blood sugar balance, resolving food sensitivities, and reducing nutrient deficiencies. [40]
One of my clients shared: “Both of my daughters’ and my own histamine reactions have significantly improved. My 5-yr old was on daily antihistamines because she had stomach pain and itching after every meal. Two weeks drinking camel milk, and I was able to take her off them.”
If this food-as-medicine approach resonates with you, and it feels like a good fit, then Desert Farms Camel Milk is a great option!
Additional Histamine Perspectives
I would also love to share some perspectives/resources from colleagues, as over the years, I’ve learned so much from many other amazing practitioners about healing histamine intolerance.
Yasmina Ykelenstam
Healing Histamine is the website and life’s work of Yasmina Ykelenstam, an exceptional, passionate, and beautiful pioneer in histamine intolerance, and also a friend of mine who passed away due to breast cancer.
While I only had the pleasure of meeting Yasmina a few times, she had this vibrance about her that made people love her immediately after meeting her. She was fierce, fun, dedicated, and brilliant.
Her site has a host of information, resources, and recipes that fit in line with addressing the root causes of histamine intolerance. According to personal communication with Yasmina, she has also found the following supplements to be extremely helpful:
- NeuroProtek: This supplement was created by the National Institutes of Health, funded by Dr. Theoharides (mast cell researcher) at Tufts. It stabilizes mast cells and prevents them from releasing inflammation, while also acting as an antihistamine.
- Mangosteen: This fruit inhibits mast cell histamine release and prostaglandin synthesis, as well as helps with IgE allergies.
- Holy basil: This adaptogenic herb is excellent for stress relief, and is an effective antihistamine and mast cell stabilizer. I personally love the tea!
Yasmina’s website also contains a helpful high histamine food list, as well as information on getting a diagnosis. I know her work will continue helping people for many years to come.
Dr. Ben Lynch
Dr. Ben Lynch is a naturopathic doctor who specializes in genetic abnormalities, and who has a lot of experience personally and professionally with histamine. [41] I love how he views histamine load as a bucket and if we have too much in our bucket – genetics, gut problems, allergies, infections, acid reflux, high-histamine foods – eventually the bucket will overflow, and that’s when high histamine can become an issue and start causing symptoms for people.
We will always have histamine in our bodies, so high histamine and its associated symptoms can come and go, depending on what’s going on in your life.
The goal is not to eliminate histamine completely. In fact, we need histamine to focus, to stay awake, to have a robust immune response, and for proper digestion (histamine stimulates stomach acid and gut motility!).
Rather, we want to focus on keeping our histamine bucket at a reasonable level, so it can still do its job without overflowing and causing symptoms.
Dr. Ben Lynch also has really helpful enzymes to reduce histamine levels. One of my favorites is Histamine Digest, which is a DAO enzyme that can be taken with food. He also makes Histamine Block Plus, which contains the DAO enzyme plus various co-factors to help with breaking down histamine!
Dr. Becky Campbell
Dr. Becky Campbell is a well-known histamine intolerance expert. Having personally experienced histamine intolerance, she was able to overcome her symptoms and help her clients and readers do the same. She has a wonderful book, The 4-Phase Histamine Reset Plan: Getting to the Root of Migraines, Eczema, Vertigo, Allergies and More, that I recommend to anyone who needs guidance in healing histamine intolerance.
Dr. Erica Peirson
Dr. Erica Peirson works with children with conditions such as Down syndrome, ASD (autism spectrum disorders), ADD (attention deficit disorder), and other neurodevelopmental conditions. [42] She helps them by addressing the root cause of these conditions, which could be related to a number of things, including oxidative stress, methylation issues, mitochondrial function, endocrine function, neurotransmitters, digestive issues, heavy metal toxicity, or nutrient deficiencies. She also addresses genetic and epigenetic factors that can contribute to these imbalances.
She has found that excess histamine and impaired histamine metabolism can not only lead to symptoms like rashes, runny noses, and itchy, watery eyes, but also acts as an excitatory neurotransmitter. It plays a role in the sleep-wake cycle, and high levels of histamine can impair sleep. Histamine plays a large role in inflammation and the immune system, and can be a trigger for autoimmune disease. It has also been linked to behavior like anger and aggression in children.
The same methylation challenges that can inhibit the clearing of histamine from the body, have also been linked to malabsorption, autism, Down syndrome, and autoimmune disease. Dr. Peirson finds that children with these conditions are often at risk for histamine intolerance. With her functional medicine approach to children’s health, she digs for the root cause through testing, diet and lifestyle changes, and supplementation.
Michael McEvoy
Michael McEvoy, founder of Metabolic Healing, outlines four different histamine receptors, each with their own impacts on the body. H1 and H4 receptors are associated with seasonal allergies and symptoms like wheezing, asthma, itching, and bronchial restriction. H2 receptors are connected to a cell-mediated inflammatory response and the gut, while H3 receptors are connected to the central nervous system and neurotransmitters. To address histamine intolerance, no matter which receptor is being affected, Michael suggests addressing gut function and microbial balance, with specific nutrient recommendations for the H1 and H4 receptors associated with seasonal allergies and H3 receptors, respectively.
Dr. Sheila Kilbane
Dr. Sheila Kilbane, a pioneer in integrative pediatric health, uses a compounded antihistamine called Ketotifen, which can help bring histamine levels down in the gut specifically. [43] If she suspects histamine is playing a role in her patient’s condition, first she will give them an over the counter antihistamine (like Zyrtec or Benadryl) for a week so see if any symptoms improve. If there is an improvement, she will use the prescription medication Ketotifen to continue managing the patient’s symptoms. With the histamine symptoms under control, Dr. Kilbane will then run tests based on the patient’s background to help her find the root cause of the histamine excess. She is a wizard at helping children heal eczema, and I love her book: Healthy Kids, Happy Moms: 7 Steps to Heal and Prevent Common Childhood.
If you’re looking for a more supported way to address your gut health, my Gut Recovery Program is specifically designed to help people with histamine issues (and many other food intolerances) because it addresses the root causes that lead to histamine intolerance, such as infections, leaky gut, and deficiencies in nutrients that help reduce histamine build-up or break down histamines (e.g. vitamin B6 and certain probiotics).
One participant in the 2022 beta group stated: “Your suggestions have been the only things that seem to work for me. I healed my sulfur and histamine sensitivities. Thank you so much!!”
More specifically, the program will help with histamine intolerance in the following ways:
- Throughout the program, we follow the Gut Recovery Diet, which is an anti-inflammatory diet that eliminates all commonly reactive foods, including those high in histamines and those that can trigger histamine release or inhibit DAO. As a low-histamine diet, it may help those with histamine intolerance.
- In addition to the diet, we are also taking supplements that help heal the gut and may also be helpful with reducing or breaking down histamines in the body, including Spore Flora, S. Boulardii, P5P, and Liver and Gallbladder Support.
- We work on eradicating common infections such as Blastocystis hominis, yeast, and H. pylori, which are big histamine producers.
Enrollment for the program is currently closed, but you can learn more about it and be notified of the next release date here.
Next Steps
As with many healing journeys, the journey with histamine intolerance may be multifaceted, and requires patience and persistence. Taking a root cause approach can offer lasting results, so I’m glad you now have some tools to get started with.
For more information about addressing the root causes of Hashimoto’s, I encourage you to pick up a copy of Hashimoto’s: The Root Cause. My cookbook Hashimoto’s Food Pharmacology contains many histamine diet-friendly recipes that can help you on your journey to healing as well.
Now, I’d like to hear from you. Please share your experience with histamine intolerance and Hashimoto’s. What tools, strategies and root cause approaches have served you best?
I wish you all the best on your healing journey!
P.S. You can download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free by signing up for my newsletter. You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow us on Facebook, and Instagram, TikTok, and Pinterest!
References
[1] Maintz L, Novak N. Histamine and Histamine Intolerance. American Journal of Clinical Nutrition. 2007; 85(5): 1185-96. doi: 10.1093/ajcn/85.5.1185.
[2] Thakkar MM. Histamine in the regulation of wakefulness. Sleep Med Rev. 2011;15(1):65-74. doi:10.1016/j.smrv.2010.06.004; Naganuma F, Nakamura T, Yoshikawa T, et al. Histamine N-methyltransferase regulates aggression and the sleep-wake cycle. Sci Rep. 2017;7(1):15899. Published 2017 Nov 21. doi:10.1038/s41598-017-16019-8
[3] Hersey M, Samaranayake S, Berger SN, et al. Inflammation-Induced Histamine Impairs the Capacity of Escitalopram to Increase Hippocampal Extracellular Serotonin. J Neurosci. 2021;41(30):6564-6577. doi:10.1523/JNEUROSCI.2618-20.2021
[4] Hersey M, Samaranayake S, Berger SN, et al. Inflammation-Induced Histamine Impairs the Capacity of Escitalopram to Increase Hippocampal Extracellular Serotonin. J Neurosci. 2021;41(30):6564-6577. doi:10.1523/JNEUROSCI.2618-20.2021
[5] Landucci E, Laurino A, Cinci L, Gencarelli M, Raimondi L. Thyroid Hormone, Thyroid Hormone Metabolites and Mast Cells: A Less Explored Issue. Front Cell Neurosci. 2019;13:79. Published 2019 Mar 29. doi:10.3389/fncel.2019.00079
[6] Garcia M, González R. Efecto de la piridoxina sobre la liberación de histamina y la degranulación de los mastocitos de rata [Effect of pyridoxine on histamine liberation and degranulation of rat mast cells]. Allergol Immunopathol (Madr). 1979;7(6):427-432.
[7] Nishida K, Uchida R. Role of Zinc Signaling in the Regulation of Mast Cell-, Basophil-, and T Cell-Mediated Allergic Responses. J Immunol Res. 2018;2018:5749120. Published 2018 Nov 25. doi:10.1155/2018/5749120
[8] Branco ACCC, Yoshikawa FSY, Pietrobon AJ, Sato MN. Role of Histamine in Modulating the Immune Response and Inflammation. Mediators Inflamm. 2018;2018:9524075. Published 2018 Aug 27. doi:10.1155/2018/9524075
[9] S-Adenosyl-L-Methionine (SAMe): In Depth. National Center for Complementary and Integrative Health. January 2017. Accessed September 18, 2023. https://www.nccih.nih.gov/health/sadenosyllmethionine- same-in-depth.
[10] De Palma G, Shimbori C, Reed DE, et al. Histamine production by the gut microbiota induces visceral hyperalgesia through histamine 4 receptor signaling in mice. Sci Transl Med. 2022;14(655):eabj1895. doi:10.1126/scitranslmed.abj1895; Schink M, Konturek PC, Tietz E, Dieterich W, Pinzer TC, Wirtz S, Neurath MF, Zopf Y. Microbial patterns in patients with histamine intolerance. Journal of Physiology and Pharmacology. 2018; 69(4). doi: 10.26402/jpp.2018.4.09.
[11] Gas & Histamine Producers on GI-MAP. Accessed September 9, 2023. https://www.diagnosticsolutionslab.com/sites/default/files/Gas-and-Histamine-Producers-on-GI-MAP.pdf.
[12] Yamaguchi N, Sugita R, Miki A, et al. Gastrointestinal Candida colonisation promotes sensitisation against food antigens by affecting the mucosal barrier in mice. Gut. 2006;55(7):954-960. doi:10.1136/gut.2005.084954
[13] Iwata K. Toxins produced by Candida albicans. Contrib Microbiol Immunol. 1977;4:77-85.
[14] Kritas SK, Gallenga CE, D Ovidio C, et al. Impact of mold on mast cell-cytokine immune response. J Biol Regul Homeost Agents. 2018;32(4):763-768.
[15] Garcia M, González R. Efecto de la piridoxina sobre la liberación de histamina y la degranulación de los mastocitos de rata [Effect of pyridoxine on histamine liberation and degranulation of rat mast cells]. Allergol Immunopathol (Madr). 1979;7(6):427-432.
[16] Nishida K, Uchida R. Role of Zinc Signaling in the Regulation of Mast Cell-, Basophil-, and T Cell-Mediated Allergic Responses. J Immunol Res. 2018;2018:5749120. Published 2018 Nov 25. doi:10.1155/2018/5749120
[17] Common symptoms of undermethylation or histadelia. Mensah Medical. http://www.mensahmedical.com/common-symptoms-of-undermethylation. Published January 12, 2016. Accessed December 21, 2022.
[18] Fogel WA. Diamine oxidase (DAO) and female sex hormones. Agents Actions. 1986;18(1-2):44-45. doi:10.1007/BF01987978; Zaitsu M, Narita S, Lambert KC, et al. Estradiol activates mast cells via a non-genomic estrogen receptor-alpha and calcium influx. Mol Immunol. 2007;44(8):1977-1985. doi:10.1016/j.molimm.2006.09.030
[19] Bódis J, Tinneberg HR, Schwarz H, Papenfuss F, Török A, Hanf V. The effect of histamine on progesterone and estradiol secretion of human granulosa cells in serum-free culture. Gynecol Endocrinol. 1993;7(4):235-239. doi:10.3109/09513599309152507
[20] Lackner S, Malcher V, Enko D, Mangge H, Holasek SJ, Schnedl WJ. Histamine-reduced diet and increase of serum diamin oxidase correlating to diet compliance in histamine intolerance. European Journal of Clinical Nutrition. 2019; 73(1): 102-104. doi: 10.1038/s41430-018-0260-5.
[21] Sanchez-Perez S, Comas-Baste O, Rabell-Gonzalez J, Veciana-nogues MT. Biogenic Amines in Plant-Origin Foods: Are They Frequently Underestimated in Low-Histamine Diets. Foods. 2018; 7(12). doi: 10.3390/foods7120205.
[22] Hrubisko M, Danis R, Huorka M, Wawruch M. Histamine Intolerance-The More We Know the Less We Know. A Review. Nutrients. 2021;13(7):2228. Published 2021 Jun 29. doi:10.3390/nu13072228; Hemarajata P, Gao C, Pflughoeft KJ, et al. Lactobacillus reuteri-specific immunoregulatory gene rsiR modulates histamine production and immunomodulation by Lactobacillus reuteri. J Bacteriol. 2013;195(24):5567-5576. doi:10.1128/JB.00261-13
[23] Comas-Baste O, Latorre-Moratalla ML, Bernacchia R, Veciana-Nogues MT, Vidal-Carou MC. New approach for the diagnosis of histamine intolerance based on the determination of histamine and methylhistamine in urine. Journal of Pharmaceutical and Biomedical Analysis. 2017; 145: 379-385. doi: 10.1016/j.jpba.2017.06.029.
[24] Wong HCG. Long-term use of diphenhydramine. CMAJ. 2015;187(14):1078. doi:10.1503/cmaj.1150066; 1. Potentially harmful drugs in the elderly: Beers list . Pharmacy Quality. March 2019. Accessed September 18, 2023. https://www.pharmacyquality.com/wp-content/uploads /2019/05/Beers-List-350301.pdf.
[25] Krysiak R, Szkróbka W, Okopień B. The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp Clin Endocrinol Diabetes. 2019;127(7):417-422. doi:10.1055/a-0653-7108
[26] Schnedl WJ, Lackner S, Enko D, Schenk M, Mangge H, Holasek SJ. Non-celiac gluten sensitivity: people without celiac disease avoiding gluten – is it due to histamine intolerance. Inflammation Research. 2018; 67(4): 279-284. doi: 10.1007/s00011-017-1117-4.
[27] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
[28] Schink M, Konturek PC, Tietz E, Dieterich W, Pinzer TC, Wirtz S, Neurath MF, Zopf Y. Microbial patterns in patients with histamine intolerance. Journal of Physiology and Pharmacology. 2018; 69(4). doi: 10.26402/jpp.2018.4.09.
[29] Camilleri M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut. 2019;68(8):1516-1526. doi:10.1136/gutjnl-2019-318427
[30] Patil AD. Link between hypothyroidism and small intestinal bacterial overgrowth. Indian J Endocrinol Metab. 2014;18(3):307-309. doi:10.4103/2230-8210.131155
[31] Shulpekova YO, Nechaev VM, Popova IR, et al. Food Intolerance: The Role of Histamine. Nutrients. 2021;13(9):3207. Published 2021 Sep 15. doi:10.3390/nu13093207
[32] Radulovic S, Wilson D, Calderon M, Durham S. Systematic reviews of sublingual immunotherapy (SLIT). Allergy. 2011;66(6):740-752. doi:10.1111/j.1398-9995.2011.02583.x
[33] Schnedl WJ, Lackner S, Enko D, Schenk M, Holasek SJ, Mangge H. Evaluation of symptoms and symptom combinations in histamine intolerance. Intest Res. 2019;17(3):427-433. doi:10.5217/ir.2018.00152
[34] Hrubisko M, Danis R, Huorka M, Wawruch M. Histamine Intolerance-The More We Know the Less We Know. A Review. Nutrients. 2021;13(7):2228. Published 2021 Jun 29. doi:10.3390/nu13072228
[35] Izquierdo-Cassas J, Comas-Baste O, Latorre-Moratalla ML, Lorente-Gascon M, Duelo A, Vidal-Carou MC, Soler-Singla L. Low serum diamine oxidase (DAO) activity levels in patients with migraine. Journal of Physiology and Biochemistry. 2018; 74(1): 93-99. doi: 10.1007/s13105-017-0571-3.
[36] Izquierdo-Cassas J, Comas-Baste O, Latorre-Moratalla ML, Lorente-Gascon M, Duelo A, Soler-Singla L, Vidal-Carou MC. Diamine oxidase (DAO) supplement reduces headache in episodic migraine patients with DAO deficiency: A randomized double blind trial. Clinical Nutrition. 2019; 38(1): 152-158. doi: 10.1016/j.clnu.2018.01.013.
[37] Salehi B, Machin L, Monzote L, et al. Therapeutic Potential of Quercetin: New Insights and Perspectives for Human Health. ACS Omega. 2020;5(20):11849-11872. Published 2020 May 14. doi:10.1021/acsomega.0c01818
[38] Li Y, Yao J, Han C, et al. Quercetin, Inflammation and Immunity. Nutrients. 2016;8(3):167. Published 2016 Mar 15. doi:10.3390/nu8030167
[39] Giuliani C, Bucci I, Di Santo S, et al. The flavonoid quercetin inhibits thyroid-restricted genes expression and thyroid function. Food Chem Toxicol. 2014;66:23-29. doi:10.1016/j.fct.2014.01.016
[40] Swelum AA, El-Saadony MT, Abdo M, et al. Nutritional, antimicrobial and medicinal properties of Camel’s milk: A review. Saudi J Biol Sci. 2021;28(5):3126-3136. doi:10.1016/j.sjbs.2021.02.057
[41] Lynch B. DGP: Histamine intolerance: How it may be affecting you [episode 14]. Seeking Health. https://education.seekinghealth.com/dgp-episode-14-histamine-intolerance/. Accessed December 21, 2022.
[42] Histamine intolerance. Peirson Center for Children. https://www.peirsoncenter.com/histamine- intolerance.html. Accessed December 21, 2022.
[43] Fugo J. 189: How to deal with histamine issues in Kids with Dr. Sheila Kilbane. Skinterrupt. https://www.skinterrupt.com/histamine-issues-kids/. Published April 8, 2021. Accessed December 21, 2022.


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
If you EVER come across a DAO product that does NOT have rice starch in it please tell us! DAO helped reduce the tremendous swelling in my abdomen but the rice starch found in every last DAO product on earth triggers my Hashimoto’s so that my thyroid crashes, so I can’t take it. All grains do that for me, and lots more food intolerances. Thanks for bringing up the other two supplements to try, I hope they will help as much as the DAO supplement did.
Aleksu – thank you so much for following my research! I’m glad you found it helpful. <3 I hope you will keep me posted on your progress.
Dr. Wentz,
Your contributions are exceptionally clear and thorough. Thank you for making difficult concepts easy to understand and for offering so many ideas for changing and healing. You are a wonderful resource for many struggling people and I commend you for putting your thoughtful comments online.
Dr. Vroni – thank you so very much for following my research! <3
hi
if ascorbic acid is high in histamine – according to your article
and vitamin c helps with histamine intolerance
which vitamin c product is best for us?
thank you
Rose – thank you so much for sharing this with me. I believe that most nutrients should come from the diet. This is why I always list food sources in the book and on the blog, for most of the nutrients, vitamins, minerals. and probiotics that are depleted in Hashimoto’s. However, some may require or prefer supplements. I recommend getting tested for deficiencies to determine your need for a supplement as instructed in the book and blog. Here is an article you might find helpful:
https://thyroidpharmacist.com/articles/thyroid-function-and-nutrient-extraction/
Another info packed article, thank you Izabella! I recently came to the conclusion that I’ve been dealing with a histamine intolerance, probably my whole life. Symptoms have tended to wax an wane but as I got older oestrogen is a big problem for me. B6 has been the most helpful for me so far and I intend to try some of the supplementation you suggest. I’ve had positive results after just 2 weeks of B6, cutting out alcohol altogether and eliminating bananas, spinach and other high histamine foods. The foods lists of what to avoid is tricky though as there seems to be lots of conflict depending on the source. I find it differs quite a bit from person to person on how they react anyway, and like you say some reactions take longer to show up so difficult to know exactly what caused it.
Mel – thank you so much! I appreciate you sharing your journey with me and I’m happy to hear you are seeing positive results! <3 Please keep me posted on you progress.
Hello,
I’m interested in a product to help the adrenals. It contains fermented Cordyceps sinensis. as well as Eleuthero, Rhodiola and some other ingredients. Should we avoid this due to the fermented Cordyceps? Would this ingredient make it a high histamine product? The product is Adrenaven.
Thank you for your information.
Janet – thank you for reaching out. <3 Please understand, I am not able to advise on whether this supplement would be appropriate for you and your specific health needs without a comprehensive health assessment. I recommend that you discuss this with your personal doctor. <3
Wanted to see if you see patient over phone live in Florida?
Yessy – thank you for reaching out. <3 I do provide a limited number of consultations, however, my consultative schedule is all full at the moment. I have a 12 week online program called Hashimoto’s Self-Management Program, that covers all of the strategies that I go through with my one-on-one clients, in a self-paced format, so that participants have access to all of the things I’ve learned about Hashimoto’s without having to schedule costly consults with me or another practitioner. Here is the link to the program:
Hashimoto’s Self-Management Program
https://thyroidpharmacist.com/enroll-in-hashimotos-program/
Excellent article. However I am confused about something. Under high histamine foods to avoid you list spinach and chocolate. Under quercetin rich foods to enjoy often you list spinach and cacoa. This seems like a contradiction. Could you please clarify it.
Anne – thank you so much for your support and feedback! <3 I am sorry that is confusing. If you have histamine intolerance, your body is reacting to the bacteria harbored on or within the food that reacts with our histamine receptors (mast cells). This is why if you are histamine intolerant, you may react to foods higher in even good bacteria, such as fermented foods and drinks and cured meats. Leaky gut is often a root cause of histamine intolerance, so my recommendation is to first try the healing diets featured in the book, which will help repair your gut. The intestinal repair might also restore your ability to produce enough DAO needed to eliminate histamines properly. <3 Here are some resources you might find helpful:
Elimination Diet
https://thyroidpharmacist.com/articles/elimination-diet-for-hashimotos
AUTOIMMUNE PALEO DIET
https://thyroidpharmacist.com/articles/autoimmune-paleo-diet
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Hashimoto’s Food Pharmacology
https://www.amazon.com/Hashimotos-Food-Pharmacology-Nutrition-Protocols/dp/0062571591?tag=thyroipharma-20
Thank you for another great article. It answers lots of questions related to my itching skin and “floating” allergies. I followed your Hashimoto Protocol, following all your articles. In addition to gluten, dairy, I avoid broth, grains, probiotic & some other foods that suppose to be ok for Hashimoto. Your Saccharomyces Boulardii and Systemic Enzyme made a big difference at the beginning of my journey. The allergies and itching increased again the last six month and nodules got visibly larger. Whenever rain, weeds, mold outside, even without eating any food, itching is back. Like Mel, I think the histamine intolorence was the cause of problems all my life. I see how nodules get larger with the allergy flairs. Don’t even want to bring it up with the doctor—here they have only one solution—just cut it. Do you think addressing the histamine issue might reduce the nodules? Anything on that subject would be very helpful. Grateful for your generosity.
Nina – thank you so much for reaching out and sharing your journey. <3 I understand how hare this can be. Nodules and goiters are often the result of toxicity and/or the autoimmune process. So, doing interventions to reduce the autoimmune attack on the thyroid, and toxicity, can be helpful to reduce them. Here is an article you may find helpful.
THYROID NODULES
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-nodules/
You may want to check out my books as well:
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Thank you for a great piece of well researched article. I have been following you for the last 2 years and there are so many things that have helped me get rid of various symptoms & live a better life.
There are two symptoms that I haven’t found a cure to,
1) acne – can histamine intolerance lead to acne? How can one deal with it?
2) a feeling of something being stuck in the throat / Mucus. This sensation has not left me for the past 8 years & I am struggling to find the root cause. On certain days ( once in six months ) it feels drained out & those are also the days I feel light overall. Could this also be a symptom of histamine intolerance?
Ple guide me to find a cure/path to clear these two symptoms. I am also tired of my acne, tried everything under the sun to get rid it. Please help!
Pooja – thank you so much for sharing and for your support! <3 Our skin is a window to our internal health. It is the body's largest elimination organ, and also a canvas where toxicities, nutrient deficiencies, food sensitivities and hormonal imbalances can show up. Women with Hashimoto's and autoimmune conditions are more likely to have dry, dull skin, rashes, hives, pre-menstrual acne and facial swelling, especially if their thyroid levels are not optimized and they are not absorbing vitamins and nutrients correctly.
THE THYROID AND SKIN
https://thyroidpharmacist.com/articles/the-thyroid-and-skin
THYROID NODULES
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-nodules/
Dr. Izabella – Thanks for all you do! I was diagnosed with hashimotos about a month ago. A doctor recommended your Hashimotos Protocol book. I’m a little over a week into the Liver Support Protocol. I lost 10 pounds of water weight in 3 days due to inflammation and congestion. The inflammation was causing peripheral neuropathy mostly in my arms and hands. This inflammation sounds like histamine. I feel like the inflammation was caused by food sensitivity. My question is: Is high levels of inflammation a symptom of histamine intolerance?
John – thank you so much for sharing. I’m so glad you are doing well on the liver support protocol. Please feel free to email my team at info@thyroidpharmacist.com if you have any questions or concern about the protocols and they will be happy to help you. <3
Did you overcome tour allergy to your pet? I am facing that now and it’s so sad since she keeps me fighting the good fight.
You mentioned Camel milk and I would like to try this. However you didn’t mention how long you had to consume this and how much you had to drink or consume? Is this something you take short term or is this something that needs to be taken long term? Any advice would be helpful. Thanks
Jeni – thank you for reaching out! <3 Everyone will react differently so it is hard to say. Here is an article with more information: BENEFITS OF CAMEL MILK IN HASHIMOTO'S HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/benefits-camel-milk-hashimotos-hypothyroidism/ ❤️
Thanks for your many helpful well researched and well written articles. They have made a huge difference in my well being. Especially The article on histamine intolerance. This was something I really struggled with. So many articles point to the healing power of bone broth, kombucha, yogurt. So I really overdid it! DAO worked miracles and I finally learned that I must be super careful with fish, to freeze leftovers immediately and avoid yogurt, kombucha and bone broth and especially smoked fish. Thanks to your kind sharing of your learning and story I am so much better! You have made all the difference.
Sandy – you are very welcome! <3 I'm so happy to hear you have found my research helpful! I hope you will keep me posted on your progress. <3
Hi! Can taking thyroid meds cause high histamine levels to rise and creating prickly skin reactions with hives? Upset stomach?
Thanks!
Actually specifically t3 meds only
Hi Ivy, I am also having histamine reactions to all thyroid medication especially T3
I have tried most brands in the UK and react to all of them. Have you found anything that helps you ?
Ivy – thank you for reaching out. ❤️ Allergic reactions and sensitivities to thyroid hormones are rare. Usually, it’s the fillers, and inactive ingredients in the thyroid hormone preparations as well as the dose that can lead to an adverse, sensitivity or allergic reaction. However, some people do experiences hypersensitivity reactions. These reactions usually present as itching/hives, palpitations, difficulty breathing, skin eruptions, fever and liver dysfunction. I’ve also found that liver support and addressing gut infections can reduce adverse reactions to medications, fillers and supplements. Here are some resources you might find helpful:
IMPORTANCE OF GUT HEALTH
https://thyroidpharmacist.com/articles/importance-gut-health/
OPTIMIZING MEDS
https://thyroidpharmacist.com/checkout/?product_id=4702
I have to say, I’ve been feeling terrible lately and my iron levels tanked, my white blood cells increased and my TSH is almost 7 out of no where. I’ve been trying to figure out what is going on past taking an iron supplement which was suggested to me. Everything together was showing me a bigger picture. Your research here has really been a light bulb moment and has given me a foundation to work off of. I have been in long term contact with a known allergy (true allergy) and I really think that it’s all related.
Thank you for the work you put into this!
Tamara, thank you so much for sharing! I’m so happy to hear my research is helping! I do hope you will keep me posted on your progress.
great post! super educating and helpful on this unique topic. Could you elaborate on the blood test mentioned? I’ve quoted it here “A whole blood histamine test can measure levels of both intracellular and extracellular blood histamine levels. Levels should be between 40 and 70 ng/mL, with levels over 70 indicating undermethylation, or poor breakdown of histamines. ”
I’ve had a lot of testing done. One being plasma histamine with the acceptable range stating equal to or below 1.8 ng/mL. I was wondering if the plasma histamine test is the same as the intracellular and extracellular blood histamine test? I do see the acceptable range is largely different though.
Hi Liz, The plasma histamine test measures histamine in the blood plasma, while the whole blood histamine test looks at both intracellular and extracellular histamine levels. This is why the reference ranges differ. Elevated whole blood histamine levels (over 70 ng/mL) can indicate undermethylation, or difficulty breaking down histamine. It’s important to discuss these results with your provider to understand their implications for your health. Hope that help.
Hey, I’ve been pursuing the issue of histamine intolerance diligently because it matches up so well with my symptoms and I tested high. But I was so deflated when I learned about the 2023 study that was done! A group of people who thought they were suffering from histamine intolerance couldn’t tell the difference in their symptoms when given a placebo or a large dose of histamines. What if I’m just imagining correlations in my own symptoms? I know you’re a super careful researcher, Dr. Wentz, so you must know about this study. How do you square up that study, which seemed to find that histamine intolerance isn’t a thing, with the rest of the info and evidence? I’m lost about what to think.
Hi Lia, Thank you for your thoughtful question! I completely understand how that study can feel deflating. Research on histamine intolerance is still emerging, and while some studies show mixed results, many patients with high histamine levels do notice symptom patterns that improve with targeted dietary and lifestyle strategies. It’s important to remember that each person’s experience is unique, labs, genetics, gut health, and other underlying factors can all influence histamine responses. I encourage you to work with a knowledgeable practitioner to explore triggers, support gut health, and address nutrient deficiencies, rather than relying solely on a single study. Your experience is valid, and sometimes clinical observations and patient-reported outcomes provide insight beyond what a single study can capture.