In addition to thyroid symptoms, are you also experiencing joint pain, burning with urination, burning with bowel movements — and/or do you have a history of kidney stones? If so, you may want to look into oxalate sensitivity. Oxalates are found in certain “healthy” foods such as dark leafy vegetables and legumes, as well as some nuts and seeds.
Preliminary research has linked oxalate build-up to thyroid disease, and while I’ve personally not had a problem with oxalates (knock on wood 😉), other thyroid patients have reported oxalate issues, and oxalates turned out to be at the root of one of my client’s joint pain and urinary symptoms… (This was a person who was “doing everything right”, but still struggling!)
While oxalate build-up has been predominantly tied to kidney stone formation, a study of thyroid autopsies found that 79 percent of adults had oxalate crystals in their thyroid glands, with prevalence increasing with age. Interestingly, people with Hashimoto’s had a higher incidence of oxalate crystals, especially in the parts of their thyroid gland that were inflamed!
This led the scientists to conclude that oxalates may play a role in contributing to Hashimoto’s, potentially causing inflammation that may trigger the autoimmune response that, in turn, results in the destruction of the oxalate crystals and the surrounding thyroid tissue. In some cases, giant cell reactions were found around the crystals, suggesting an ongoing immune response.
Some believe that an oxalate-free diet is the only path to freedom from these symptoms, but I have found that in many cases, oxalates may need to be reduced in the short term, and that there are underlying issues that can be addressed to resolve oxalate sensitivity!
Thus, for those of us with thyroid disease, it is important to recognize the role of oxalates and how we can address them.
In this article, I’ll dive into:
- What are oxalates and how do they impact thyroid health?
- What are the symptoms of oxalate sensitivity?
- How to test for oxalate issues
- Treatment options for oxalate build-up
- Eating oxalates again – yay!
What Are Oxalates?
Oxalates are naturally occurring molecules that are found in certain foods, and are also a waste product made by our bodies and excreted through our kidneys.
Oxalates form salts in the body by combining with calcium, after we consume foods that have a high oxalate content. When our body can’t process the calcium-oxalate compounds, they crystallize and lodge in our organs, causing inflammation, which can turn into painful kidney stones and lead to other inflammatory symptoms of oxalate buildup in the body, such as joint pain, pain with urination/bowel movements, and even inflammation of the thyroid gland.
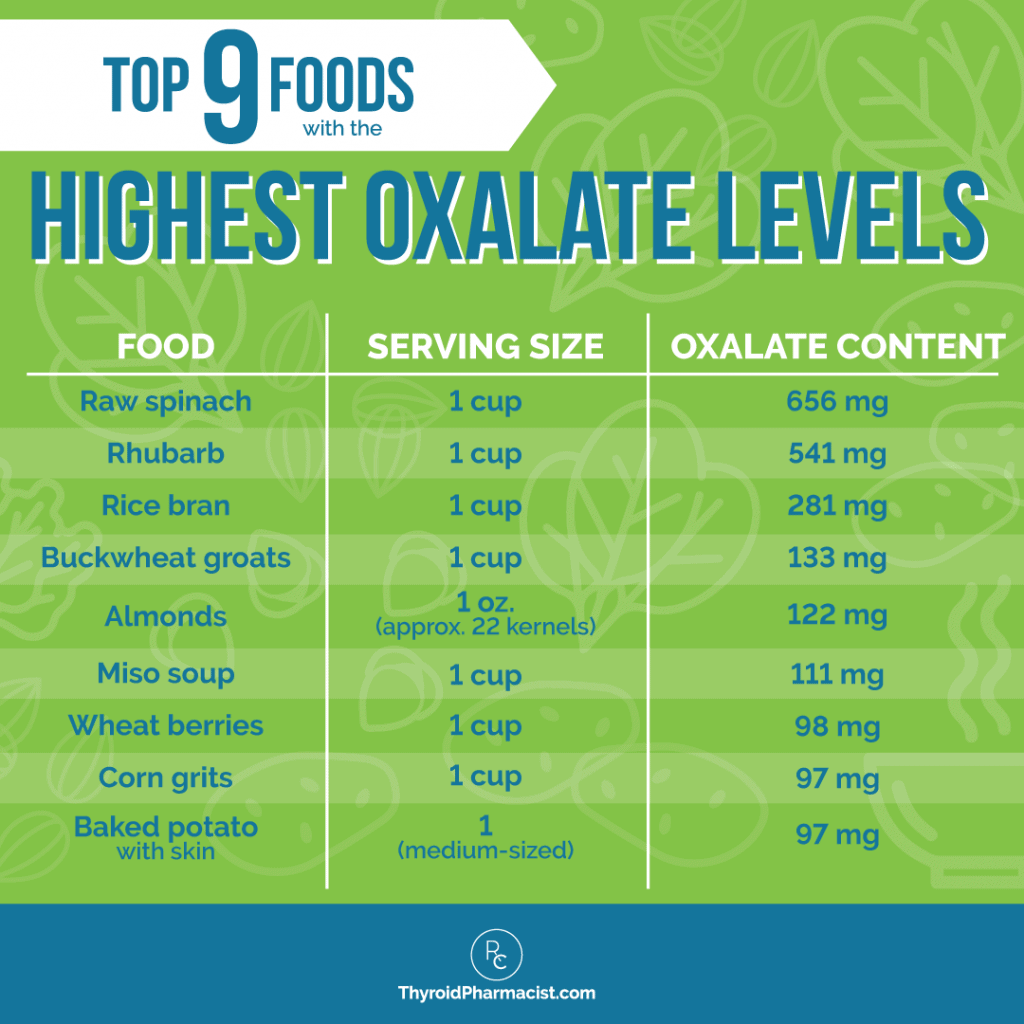
The top common foods with the highest oxalate content per serving include: rhubarb, rice bran, buckwheat, almonds, miso soup, wheat berries, corn, potatoes, navy beans, beets, cocoa powder, and raspberries.
Primary and Secondary Hyperoxaluria
Oxalates are usually excreted from the body via urine.
A healthy range of oxalate excretion sits between 10-40 mg per day. Hyperoxaluria, or increased oxalate excretion, occurs when an individual excretes more than 40-45 mg of oxalates in a 24-hour window. It can contribute to the formation of kidney stones as well as other symptoms (more on that later in this article).
There are two different types of hyperoxaluria: primary hyperoxaluria and secondary hyperoxaluria.
Primary hyperoxaluria occurs when there is an inherited or genetic defect in the function of the enzymes that carry out oxalate metabolism. It is a rare genetic and metabolic disorder. (Within primary hyperoxaluria, there are three subtypes: types I, II, and III, each of which has a genetic defect in a different enzyme along the oxalate metabolism pathway.)
Secondary hyperoxaluria occurs due to non-genetic factors. Within secondary hyperoxaluria, there are two additional subtypes: dietary hyperoxaluria (caused by an increased consumption of oxalate-containing foods) and enteric hyperoxaluria (caused by changes in the intestinal microbiome).
Secondary hyperoxaluria is more common in those with Hashimoto’s, as this autoimmune condition is often associated with changes in the gut (intestinal) microbiome, and many people following thyroid-healing diets may consume a high amount of fruits/veggies that are high in oxalates.
How Do Oxalates Impact Thyroid Health?
Hyperoxaluria can indicate high levels of oxalates or oxalic (oxalate) buildup within the body.
As mentioned earlier, while oxalate buildup has been predominantly tied to kidney stone formation, a study of thyroid autopsies found that 79 percent of adults had oxalate crystals in their thyroid glands, with prevalence increasing with age. Interestingly, people with Hashimoto’s had a lower incidence of oxalate crystals, especially in the parts of their thyroid gland that were inflamed!
This led the scientists to conclude that oxalates may play a role in contributing to Hashimoto’s, potentially causing inflammation that may trigger the autoimmune response that, in turn, results in the destruction of the oxalate crystals and the surrounding thyroid tissue. In some cases, giant cell reactions were found around the crystals, suggesting an ongoing immune response.
A 2000 case report featured four people with a rare genetic disorder that resulted in oxalate build-up as well as the development of hypothyroidism. This report highlighted the role of oxalates in causing damage to the thyroid gland, and thus, hypothyroidism.
To complicate things further, a 2006 study reported that a person had developed excess oxalates due to hypothyroidism that was induced by amiodarone (one of the most thyroid toxic drugs)!
As such, it’s important to look into identifying any potential underlying oxalate issues.
What Are the Symptoms of Oxalate Sensitivity?
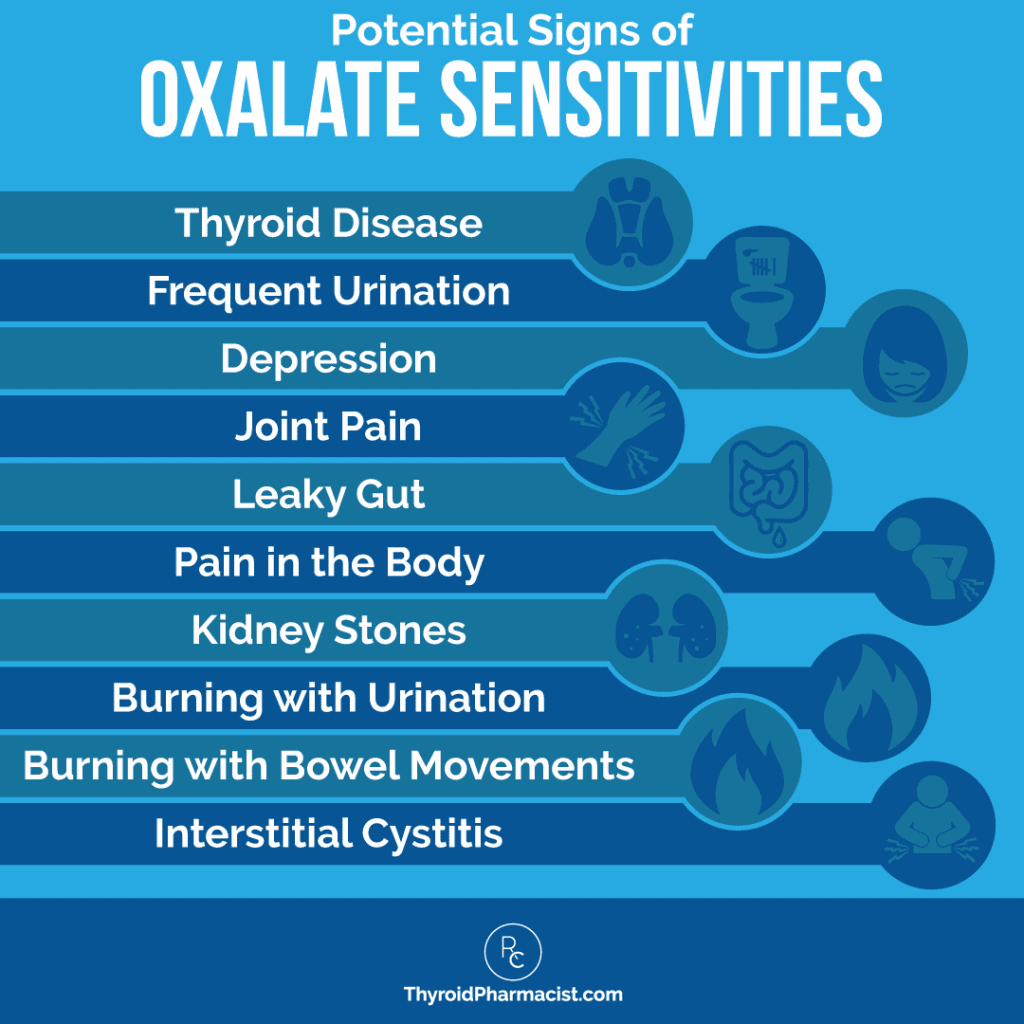
Oxalate buildup or sensitivity should be suspected if you have any of the following symptoms (in addition to a thyroid condition like Hashimoto’s or Graves’):
- Joint pain
- Pain in the body
- Burning with urination
- Interstitial cystitis
- Burning with bowel movements
- Leaky gut
- Depression
- Kidney stones
Root Causes of Oxalate Sensitivity
Oxalate sensitivity can be caused by various factors that result in the improper breakdown of oxalates in the body, such as a rare genetic disorder, any issues that affect the small intestine such as small intestinal bacterial overgrowth (SIBO) or small intestinal fungal overgrowth (SIFO), other kinds of gut dysbiosis (which can result from past antibiotic use), gastric surgery, Crohn’s disease, and short bowel syndrome.
People with a low intake of calcium (such as those following a dairy-free diet, which is otherwise beneficial in Hashimoto’s) may also have exacerbated oxalate issues. This is because calcium in our foods can reduce our absorption of oxalates.
As mentioned previously, changes in the intestinal microbiome can lead to secondary hyperoxaluria. Gut microbiome imbalances can result in a deficiency in the probiotic bacteria Oxalobacter formigenes, which has an enzyme known as “oxalyl-CoA decarboxylase” that breaks down oxalate. As such, a deficiency in Oxalobacter formigenes has also been connected with oxalate sensitivity.
The use of two specific antibiotics, erythromycin and azithromycin (the popular “Z-pack”), is especially likely to cause a depletion of this bacteria. A 2011 study found that while 59 percent of people in the general population had a measurable level of Oxalobacter formigenes on stool tests, only 18 percent of past azithromycin users, and 26 percent of past erythromycin users, had this bacteria in their stools. In contrast, about 40 percent of Amoxicillin antibiotic users had the beneficial bacteria on stool tests.
Lastly, fungi (yeast and/or mold) overgrowth anywhere in the body, can be a root cause of oxalate buildup, as certain kinds of fungi, such as Candida or Aspergillus, produce oxalates in a process called biomineralization. When there is an overgrowth of yeast or fungus, the excess amounts of oxalates that are emitted can lead to oxalate buildup and contribute to the symptoms mentioned above. In my experience, eliminating these pathogenic growths can eliminate or reduce oxalate issues.
How to Test for Oxalate Issues
In some cases, oxalates can cause kidney stones. From a conventional medicine standpoint, if you are currently passing kidney stones, the stones can be tested by your doctor to see if they contain calcium oxalate. (If this test is positive, a low oxalate diet should be followed to help prevent the formation of more kidney stones — more on that further on in this article.)
However, when looking through the lens of functional and root cause medicine (and whether you are currently passing kidney stones or not), I recommend a urine metabolite test.
While some individuals recommend a trial of a low oxalate diet to determine if oxalates are indeed causing your symptoms, a low oxalate diet can — in some cases — cause “oxalate dumping” (where too many oxalates try to leave your body all at once). This can increase symptoms. Additionally, an elimination diet will not find the root cause of the oxalate issues.
Thus, if you suspect you may have an oxalate sensitivity, I recommend taking the Organic Acids Test (OAT) from Great Plains Labs, which can be ordered through your functional practitioner. Alternatively, you can also get the Organix Dysbiosis Marker Test Kit from Genova, which can be self-ordered. Not only do these tests help uncover oxalates issues, they can also provide further guidance on potential root causes of oxalate issues, such as yeast, mold and even some markers that may suggest SIBO (although the OAT doesn’t test for SIBO specifically).
The Conventional Approach to Correcting Oxalate Buildup
The conventional approach to correcting oxalate buildup includes a combination of medications or prescription vitamins, some dietary changes, as well as corrective procedures, depending on the amount of buildup present and the cause.
If there is some buildup but no kidney stones have formed yet, a prescription dose of vitamin B6 or potassium citrate is usually recommended. Thiazide diuretics are also recommended to help flush oxalates out of the kidneys. These prescription medications/vitamins can be especially helpful in the case of secondary hyperoxaluria.
For rare cases of type I primary hyperoxaluria, the FDA recently approved subcutaneous injections of a new drug, Oxlumo (lumasiran), as a potential treatment option. Oxlumo aims to target the genetic defects in primary hyperoxaluria that contribute to increased oxalate excretion and buildup.
The conventional approach also recommends dietary changes such as increasing water intake to flush out oxalates, as well as focusing on low oxalate foods.
If there is an excess amount of oxalates that have started to form kidney stones, there are two options. The first and least invasive option is to increase fluid intake to help the stones pass on their own. However, in some cases, a corrective procedure may be needed, so the second option consists of more invasive procedures, such as:
- Shockwave lithotripsy, in which shock waves are sent through water to break the stones apart in the affected area.
- Ureteroscopy, in which a ureteroscope is inserted through the urethra to the ureter, to either break the stones apart, or retrieve and remove them.
- Percutaneous nephrolithotomy, which is used as a last resort if the options above do not work. During this procedure, an incision is made in the back to access the kidneys directly and suction out the stones.
The Root Cause Approach to Correcting Oxalate Buildup
As mentioned earlier, while logic may suggest that we should limit all foods that contain oxalates, it’s actually not ideal or realistic to stop them all at once. This is because in theory, stopping our intake of all oxalates can lead to a period of “oxalate dumping” and cause unpleasant symptoms.
That said, functional medicine lab tests are not available to everyone, so I want to share more about trialing the Low Oxalate Diet.
Low Oxalate Diet
It may be helpful to start with taking an inventory of your actual oxalate intake. The average diet contains 250 mg of oxalates per day, and if you are eating a significant amount above that, this can lead to oxalate symptoms, simply because you are eating much more than you can break down. (That said, there can be more complicated, genetic reasons for poor breakdown, such as primary hyperoxaluria, and more simple ones, such as B6 deficiency or yeast overgrowth.)
In the case of my client, who was “doing everything right”, but continued to struggle with pain and urinary issues, we found that she had a yeast overgrowth in her body (through the OAT test). She had been eating a very high oxalate diet that included almond milk smoothies with spinach and chard, as well as a lot of beets. Additionally, she had poor sleep and poor dream recall, which are potential symptoms of B6 deficiency.
Addressing her yeast overgrowth, adding B6, and modifying her diet resolved her pain and urinary issues, as well as helped her sleep better.
In order to modify one’s diet, it’s helpful to be aware of common foods with the highest levels of oxalates, as well as foods with lower oxalate levels.
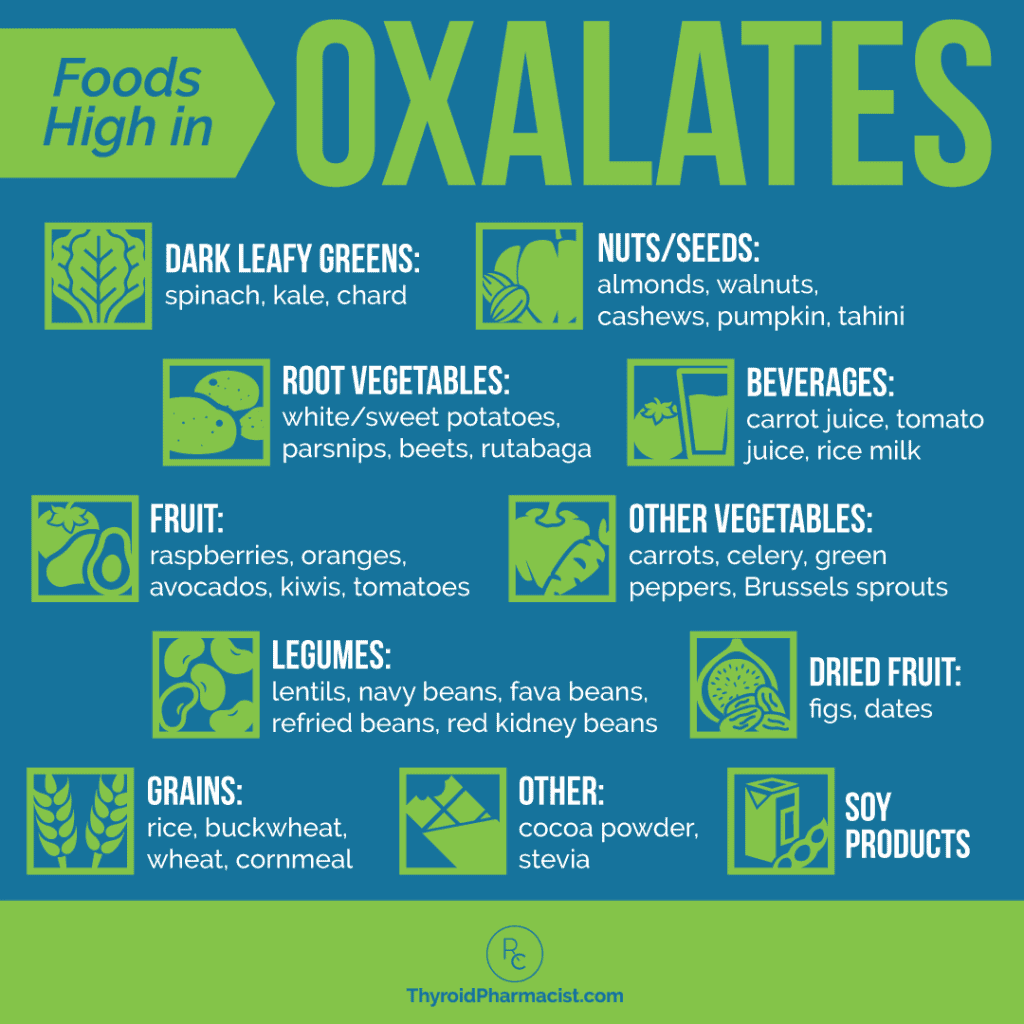
The foods with the highest oxalate content per serving (around 50 mg/serving or higher) include:
- Dark leafy greens: spinach, kale, chard
- Root vegetables: white/sweet potatoes, parsnips, beets, rutabaga
- Other vegetables: carrots, celery, green peppers, Brussel sprouts
- Fruit: oranges, avocados, kiwi, tomatoes, raspberries
- Dried fruit: figs, dates
- Nuts/seeds: almonds, walnuts, cashews, pumpkin, tahini
- Grains: brown rice, buckwheat, wheat
- Beverages: carrot juice, tomato juice, rice milk
- Soy products
- Legumes: navy beans, fava beans, lentils, refried beans, red kidney beans
- Other: cocoa powder, stevia
The other foods that are commonly eaten on a Paleo diet, and that have an oxalate content above 50 mg per serving, include: baked potatoes, beets, cocoa powder, and okra. Raspberries come in close, at 48 mg per serving!
There are also some foods that have an ultra high oxalate content. However, we use them sparingly (like black pepper). These foods are usually not as much of a concern unless you are using more than 1 tsp at a time (that’s a lot of pepper!).
Foods with moderate levels of oxalates (i.e. ranging between those found in high and low oxalate foods) include:
- Fruits: apples, apricots, berries (except raspberries), peaches, grapefruit, plums
- Grains: white rice
- Nuts/seeds: sunflower seeds, pecans
Foods with low oxalate levels (less than 50 mg/serving) include:
- Meats
- Dairy: all dairy products (although dairy is not recommended for those with Hashimoto’s)
- Fruits: melons, mangoes, grapes, coconut
- Vegetables: broccoli, cauliflower, cabbage, lettuce, mushrooms, onions, red peppers, cucumbers
- Condiments: mustard, vinegar, mayonnaise
- Sweeteners: honey, maple syrup
- Beverages: herbal teas, apple juice, water, cider
As mentioned above, a standard diet takes in about 250 mg of oxalates per day. However, some people may choose to eat a low oxalate diet to prevent oxalate buildup. Consuming under 100 mg is recommended, but under 50 mg is ideal, unless your doctor suggests otherwise (more on that further on in this article!).
To discover the amount of oxalates in specific foods, check out this helpful and thorough list by Jill Harris and Fred Coe: Oxalate Content by Food Type (it includes 170+ different foods!).
In general, a helpful recommendation may be to start by eating moderate oxalate foods for one week (reduce your intake to less than 100 mg of oxalates per day). Let the body adjust, and then go to low oxalate foods (less than 50 mg of oxalates per day). When a higher oxalate food is consumed, it should be rotated, to avoid over-concentration of oxalates and sensitivities to that food.
Once a person feels better, it’s easy to slowly let high oxalate foods creep back in. These foods should always be rotated. If symptoms return, it’s important to reduce oxalate intake immediately, to avoid possible stone formation.
Additional ways to support healing with oxalate sensitivities include:
- Drinking plenty of fluids, mainly water, as this will help prevent kidney stones. Water will help dilute the substances found in urine, and therefore help prevent stones.
- Adding a few slices of lemon to your water will not only flavor it, but will also help stop the formation of stones. This is because lemons contain citrate, which prevents oxalate buildup by binding to calcium.
- Reducing your intake of processed foods. Processed foods have high amounts of sodium, and when we consume too much sodium, the kidneys begin to excrete excess calcium from the urine; the calcium then combines with oxalates and stones form.
- Avoiding excess protein. Excess protein can contribute to kidney stone formation by creating more uric acid in the body and lowering the levels of citrate in the blood (which, as mentioned above, can help bind calcium and prevent oxalate buildup). Check out my article on safe proteins for Hashimoto’s, to calculate your ideal daily protein intake.
Nutrients and Supplements
Probiotics and Enzymes
As mentioned previously, a deficiency in Oxalobacter formigenes can contribute to oxalate sensitivity. It is thus no surprise that a 1999 study by Sidhu and colleagues, demonstrated that supplementing with Oxalobacter formigenes, which acts as both a probiotic and enzyme, can help break down oxalates.
While Oxalobacter formigenes has the most studies behind it with respect to breaking down oxalates, lactic acid probiotics, Bifidobacterium lactis, Enterococcus faecali, and Eubacterium lentum also contain oxalyl-CoA decarboxylase and may help with breaking down oxalates.
Oxabact and Oxazyme are probiotic treatments that have both been clinically tested to significantly reduce oxalates by directly providing the probiotic O. formigenes (Oxabact) and by providing the enzyme that breaks down oxalates (Oxazyme). These enzymes are currently undergoing testing for efficacy and are available through clinical trials. They are currently in the third phase of testing and are one step closer to becoming available to the general public through pharmacies specializing in “orphan drugs” (as explained below).
Please note that while the probiotic and enzyme are technically supplements, they are currently classified as “orphan drugs” by the FDA, meaning that they are indicated for rare conditions and not widely available. Your doctor will have to work with a pharmacy that specializes in orphan drugs. Additionally, these may not be covered by insurance.
That said, in researching this article, I was pleased to see that the probiotics and supplements I most commonly recommend can help with oxalate issues as well!
The following probiotics are widely available:
- Bifidobacterium lactis can be found in Ther-Biotic Complete and ProB 50, two of my favorite high dose probiotics.
- Enterococcus faecali is found in Dr. Ohhira’s brand of probiotics (please note, this brand does use fermented soy in the development of the probiotics, but most people with soy reactions should be able to tolerate it).
- MegaSporeBiotic and S. boulardii, my other two favorites, do not contain oxalyl-CoA decarboxylase-containing strains but may still be helpful in restoring gut health.
Conjugated Bile Acids
In addition to probiotics, conjugated bile acids (CBA) can also help to clear out oxalates, by preventing their reabsorption in the body.
A megadose of 9 grams per day of natural conjugated bile acids, was used in people with short bowel syndrome (SBS), who are known to hyper-reabsorb oxalates due to the structural bowel changes present with the disorder. Within three months of CBA use, their oxalate levels measured normal.
People without SBS are not necessarily reabsorbing oxalates at a higher rate than normal, but will likely benefit from reduced reabsorption. A smaller dose of conjugated bile acids, which are found in supplements such as ox bile, as well as any ingredients that support bile flow such as taurine, may help reduce the overall oxalate load in the body when used in conjunction with other interventions. You may benefit from Rootcology Liver & Gallbladder Support, which contains 75 mg of ox bile and 100 mg of taurine per 3 capsules. Additionally, some clinicians like to recommend TUDCA, a specific form of bile acids that is derived from taurine, to target oxalates.
Calcium
Calcium can block the absorption of oxalates, and people with a low dietary intake of calcium are more likely to be oxalate sensitive. (Please note that while dairy is rich in calcium, and although oxalates are not present in dairy, it is best to avoid dairy with Hashimoto’s).
In theory, taking calcium supplements with meals may help with binding up oxalates in the gut and preventing their absorption and concentration in the rest of the body, including the kidneys, where they turn into oxalate crystals.
According to a 2006 research article, “The preferred calcium supplement for people at risk of stone formation is calcium citrate because it helps to increase urinary citrate excretion. A dose of 200–400 mg is recommended if dietary calcium cannot be increased.”
B6
B6 deficiency has also been associated with oxalate issues. Symptoms of B6 deficiency can include poor dream recall, changes in mood, and low energy (as is the case with many B vitamin deficiencies).
In some cases, such as the case with my client described above, correcting a B6 deficiency (along with targeting the other root causes of oxalate issues) can help with symptoms of oxalate buildup.
In a 1999 study conducted by Curhan and colleagues, taking a B6 supplement with a dose greater than 40 mg per day resulted in the lowest risk of kidney stones (which are caused by oxalate crystals).
P5P (pyridoxal 5’phosphate), a form of B6, may be safer than the pyridoxine form. For this reason, I like the P5P from Pure Encapsulations as a starting point. A daily dose of 50 mg – 250 mg can be helpful for processing oxalates. I don’t recommend doses above 300 mg per day, as higher doses can be neurotoxic.
A Note on the Vitamin C Controversy
Some sources say to restrict vitamin C with oxalate sensitivity. However, a 1999 study did not find that vitamin C intake was related to kidney stone formation, a known consequence of oxalate sensitivity.
If you are having any of the common oxalate symptoms, you may benefit from a three week trial of a low oxalate diet as described above, along with supplementing with calcium and B6 vitamins, probiotics, and conjugated bile acids.
Addressing Gut Dysbiosis
As mentioned earlier, gut dysbiosis, especially yeast overgrowth, as well as SIBO and mold toxicity, can contribute to oxalate excess. One of the steps to correcting oxalate buildup is addressing this dysbiosis.
First things first, I recommend screening for yeast through the Great Plains Organic Acids Test. If this test does not find any yeast, mold, or bacterial abnormalities, I would then recommend testing for SIBO specifically, as SIBO is present in 50 percent of people with hypothyroidism, and addressing any dysbiosis is a necessary part of one’s plan to overcome oxalate sensitivity.
I also recommend the GI-MAP stool test, which allows you to fully map and determine what microorganisms and/or pathogens are in your gut. This is a direct approach to determine whether there is a yeast/mold overgrowth or other gut dysbiosis present.
In the case that there is, removing triggering foods (such as high carbohydrates foods, to address Candida) and taking probiotics such as S. Boulardii by Rootcology, may promote a healthy gut.* For more information, I encourage you to read my comprehensive articles on addressing Candida and mold toxicity.
The Takeaway
Oxalates are substances that are found to be particularly high in some foods. In excess amounts, oxalates can build up, leading to inflammation and the progression of autoimmune conditions, such as Hashimoto’s.
Symptoms of oxalate buildup or sensitivity can range from joint pain to depression or kidney stones. Because the symptoms can be vague and overlap with other conditions, testing for oxalate buildup and/or sensitivity is important.
If there is buildup, there are steps you can take to reduce it and improve your health! These steps can include addressing your gut health, reducing oxalate-rich foods in your diet, increasing your water intake, and supplementing with B6, calcium, conjugated bile acids, and/or probiotics.
Most of my clients see a big reduction in their pain and other symptoms, once they start implementing these changes.
I hope that this information helps you improve your health and Hashimoto’s!
Has oxalate sensitivity been an “aha” moment in your journey?
P.S. You can also download a free Thyroid Diet Guide, 10 Thyroid friendly recipes, and the Nutrient Depletions and Digestion chapter. You will also receive occasional updates about new research, resources, giveaways and helpful information.
For future updates, make sure to follow us on Facebook and Instagram!
References
- Reid J, Choi C, Oldroyd N. Calcium Oxalate Crystals in the Thyroid: Their Identification, Prevalence, Origin, and Possible Significance. American Journal of Clinical Pathology. 1987;87(4):443-454. doi:10.1093/ajcp/87.4.443.
- Bhasin B, Ürekli HM, Atta MG. Primary and secondary hyperoxaluria: Understanding the enigma. World J Nephrol. 2015;4(2):235-244. doi:10.5527/wjn.v4.i2.235
- Shekarriz B, Stoller M. Hyperoxaluria: Practice Essentials, Oxalate Production and Function, Pathophysiology and Etiology. Medscape website. https://emedicine.medscape.com/article/444683-overview#a13. Accessed February 8, 2021.
- Frishberg Y, Feinstein S, Rinat C, Drukker A. Hypothyroidism in primary hyperoxaluria type 1. The Journal of Pediatrics. 2000;136(2):255-257. doi:10.1016/s0022-3476(00)70112-0.
- Tintillier M, Pochet J, Cosyns J, Delgrange E, Donckier J. Late-onset primary hyperoxaluria triggered by hypothyroidism and presenting as rapidly progressive renal failure – description of a new mutation. Clinical Nephrology. 2004;62(08):155-157. doi:10.5414/cnp62155.
- Castellaro A, Tonda A, Cejas H et al. Oxalate induces breast cancer. BMC Cancer. 2015;15(1). doi:10.1186/s12885-015-1747-2.
- Shaw W. OXALATES CONTROL IS A MAJOR NEW FACTOR IN AUTISM THERAPY. The Great Plains Laboratory, Inc. 2015. https://www.greatplainslaboratory.com/articles-1/2015/11/13/oxalates-control-is-a-major-new-factor-in-autism-therapy. Accessed September 7, 2017.
- Hoppe B. Diagnostic and therapeutic approaches in patients with secondary hyperoxaluria. Frontiers in Bioscience. 2003;8(5):e437-443. doi:10.2741/1135.
- Brooks, M. FDA Clears First Drug to Treat Ultra-Rare Metabolic Disorder. Medscape website. https://www.medscape.com/viewarticle/941520. Accessed February 8, 2020.
- Cleveland Clinic. Kidney Stones: Oxalate-Controlled Diet | Cleveland Clinic. Cleveland Clinic. 2015. https://my.clevelandclinic.org/health/articles/kidney-stones-oxalate-controlled-diet. Accessed September 7, 2017.
- Pendick D. 5 steps for preventing kidney stones – Harvard Health Blog. Harvard Health Blog. 2013.vhttps://www.health.harvard.edu/articles/5-steps-for-preventing-kidney-stones-201310046721. Accessed September 7, 2017.
- Hoppe B, von Unruh G, Laube N, Hesse A, Sidhu H. Oxalate degrading bacteria: new treatment option for patients with primary and secondary hyperoxaluria?. Urological Research. 2005;33(5):372-375. doi:10.1007/s00240-005-0497-z.
- Kelly J, Curhan G, Cave D, Anderson T, Kaufman D. Factors Related to Colonization with Oxalobacter formigenesin U.S. Adults. Journal of Endourology. 2011;25(4):673-679. doi:10.1089/end.2010.0462.
- Sidhu H, Schmidt M, Cornelius J. Direct correlation between hyperoxaluria/oxalate stone disease and the absence of the gastrointestinal tract-dwelling bacterium Oxalobacter formigenes: possible prevention by gut recolonization or enzyme replacement therapy. J Am Soc Nephrol. 1999;10(Suppl 14): S334-40.
- Plotner B. Options With Oxalate Intolerances – Nourishing Plot. Nourishing Plot. 2015. http://www.nourishingplot.com/2015/03/07/options-with-oxylate-intolerances/. Accessed September 7, 2017.
- Okombo J, Liebman M. Probiotic-induced reduction of gastrointestinal oxalate absorption in healthy subjects. Urological Research. 2010;38(3):169-178. doi:10.1007/s00240-010-0262-9.
- Emmett M, Guirl M, Santa Ana C, et al. Conjugated bile acid replacement therapy reduces urinary oxalate excretion in short bowel syndrome. Am J Kidney Dis. 2003;41(1):230-237. doi:10.1053/ajkd.2003.50012.
- Finkielstein V. Strategies for preventing calcium oxalate stones. Canadian Medical Association Journal. 2006;174(10):1407-1409. doi:10.1503/cmaj.051517.
- Curhan G, Willett W, Speizer F, Stampfer M. Intake of vitamins B6 and C and the risk of kidney stones in women. J Am Soc Nephrol. 1999;10(4):840-5.
- Health Resources and Services Administration. Orphan Drug Designations And Approvals List.; 2016. https://www.hrsa.gov/opa/programrequirements/orphandrugexclusion/orphandruglist072016.pdf. Accessed September 7, 2017.
- Yakowicz W. How a College Professor Built a $42 Million Pharmacy for Rare Disease Drugs. Inccom. 2016. Available at: http://www.inc.com/will-yakowicz/inc-5000-2016-pantherx-specialty-pharmacy.html. Accessed September 7, 2017.
- Tuason MM, Arocena JM. Calcium oxalate biomineralization by Piloderma fallax in response to various levels of calcium and phosphorus. Appl Environ Microbiol. 2009;75(22):7079-7085. doi:10.1128/AEM.00325-09
- Kelly JP, Curhan GC, Cave DR, Anderson TE, Kaufman DW. Factors related to colonization with Oxalobacter formigenes in U.S. adults. J Endourol. 2011;25(4):673-679. doi:10.1089/end.2010.0462
- Sidhu H, Schmidt ME, Cornelius JG, Thamilselvan S, Khan SR, Hesse A, Peck AB. Direct correlation between hyperoxaluria/oxalate stone disease and the absence of the gastrointestinal tract-dwelling bacterium Oxalobacter formigenes: possible prevention by gut recolonization or enzyme replacement therapy. J Am Soc Nephrol. 1999 Nov;10 Suppl 14:S334-40. PMID: 10541258.
- Okombo, J., Liebman, M. Probiotic-induced reduction of gastrointestinal oxalate absorption in healthy subjects. Urol Res. 2010;38:169–178. https://doi.org/10.1007/s00240-010-0262-9
- Finkielstein VA, Goldfarb DS. Strategies for preventing calcium oxalate stones. CMAJ. 2006;174(10):1407-1409. doi:10.1503/cmaj.051517
- Brown M, Ameer M, Beier K. Vitamin B6 Deficiency. StatPearls. Florida: Treasure Island; 2020. https://www.ncbi.nlm.nih.gov/books/NBK470579/. Accessed February 8, 2021.
Note: Originally published in September 2016, this article has been revised and updated for accuracy and thoroughness.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Finally, someone other than Sally K. Norton addressing the oxalate issue. I always took excellent care of myself since my twenties. (I am now 70.) Would never be without a garden which supplied swish chard, beets, spinach etc..doing research, I always read the more veggies you eat the better for your health. I was very disciplined in my eating habits, yet always had pain in my body. My legs, joints, arms etc..and always pain in my kidneys. I went to many doctor who were baffled by my symptoms. I suffered for years. I thought well maybe I need to start juicing to cleanse my body. I was slowly becoming even sicker. I could not work, and could barely walk due to the pain in my legs. Unfortunately, at that time there was no information on oxalates. I then developed hashimoto thyroid disease and became very chemically sensitive. I desperately needed thyroid medication and yet the medication made me very sick. It had become a nightmare of a vicious cycle. Finally after a lifetime of being sick, I came across nutritionist Sally K. Norton who had almost the same story as mine! when I read how she too suffered for many, many years..I cried. I finally knew what was wrong with me! All of the greens, smoothie, beans etc that I thought were helping me..were actually killing me. I immediately changed my diet and could start feeling the difference in a matter of days. Regrettably, I discovered this information at the age of 69. Better late than never. I am not 100%. It takes many years for the oxalates to leave the tissues in the body. However, the improvement is amazing.
Thank you Dr. Izabella for bringing this information to your patience and readers. I pray it will prevent others from going through the same suffering that I had to endure.
Sincerely,
Theresa
Theresa – thank you so very much for sharing your journey with me! ❤️ I’m so glad you have found a practitioner to work with and are feeling better! It’s never to late! Please keep me posted on your continued progress.
I had frequent trouble with kidney stones and have Hashimotos. My Urologist wanted me to stop eating foods with oxalates and to take Potassium citrate to make my itinerary more alkaline. He said my acidic urine was causing the stones, not to mention causes inflammation in the body. I asked how to do this with foods instead of medicine and he told me 1/4 cup lemon juice a day, but still refrain from oxalates in food. I started the daily organic fresh squeezed lemon juice, still eat foods with oxalates because I am so limited in what foods I can eat, and have not had a kidney stone since!
Patti – thank you so much for sharing what has worked for you! 💕
I discovered my oxalate sensitivity because I felt achy, broke out with eczema, and felt terrible after eating sweet potatoes. Sweet potatoes are very high in Oxalates and should be on the root vegetable list.
Alison – thank you so very much for sharing this with me! 💕 I would love to hear how your thyroid healing journey is going.
Hello. Thank you for talking about Oxalates, as most people have never heard of them. Unfortunately, there is quite a bit of erroneous information in this article, especially the information about food. Please join the Trying Low Oxalates Facebook group which is science based. They have a lab that tests food for oxalate levels and they provide a spreadsheet with the results of all the food testing. There is extensive information on Oxalates provided in their units.
Hilary – thank you so much for sharing this information with me! ❤️
Dr. Wentz,
Although I appreciate how detailed you are in gathering information for people with thyroid conditions, this is way too complicated and SO much information in one article. All the research that I do seems to just cause more stress, which I believe to be the real culprit when it comes to autoimmune disorders. Can it all be simplified somehow? All the testing and avoiding certain foods and exercise and. and. and…. it’s a full time job to keep up with it all, and I don’t have that kind of time. I can’t even find a doctor who meets my needs.
If I could just find a much simpler way to get my thyroid healthy, that would be great!
Thank you,
Alli
Alli – thank you so much sharing your journey. I understand how overwhelming and hard this is. ❤️ I have found that diet is very much an individual intervention. What works for one person, may not work for another, as each individual may be different in their triggers and needs. I generally recommends a full Root Cause Autoimmune Protocol (AIP) Diet for 30-90 days, which goes a long way to remove trigger foods, reduce inflammation, heal the gut, and even reduce thyroid antibodies! I recommend eliminating gluten, grains, dairy, and soy indefinitely, but we can have a rich, full diet with foods that we aren’t sensitive to. The end goal is for everyone to come up with their own personalized Root Cause Paleo Diet (modified for your personal sensitivities) that you can enjoy for life! A food and symptom journal can be very helpful for determining what foods you are sensitive to. If you have any questions please feel free to email my team at info@thyroidpharmacist.com and they will be happy to help. Here are some resources I hope you find helpful as well.
AUTOIMMUNE PALEO DIET
https://thyroidpharmacist.com/articles/autoimmune-paleo-diet
LOW FODMAP DIET FOR SIBO, IBS, AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/low-fodmap-diet-sibo-ibs-hashimotos/
ELIMINATION DIET
https://thyroidpharmacist.com/articles/elimination-diet-for-hashimotos
Hi Dr.Wentz, i have had a history of kidney stones formation and then i also got diagnosed with Hashimotos. I didnt know that they could be related. I have recently also developed knee joint pains especially when climbing up stairs. I have also read the Hashimotos protocol and i am ona gluten free diet. I feel that i have more energy now and my hair is getting its shine back. But i also consume nuts especially cashews and almonds and also kidneg beans and lentils. Looks like these cause oxalates. I also got my kidney stone tested and it was calcium oxalate. I have dad kidney stones 4 times and have hospitalized 3 out of the 4 times. Seems like i keep forming stones. So is there a chance that i have Hashimotos due to oxalate sensitivity. And if i go on a oxalate reduction diet i may be able to get rid of kidney stones, joitm pain and Hashimotos?
I will also get the oxalates test done. Its tough to get tests done in Australia without a doctors prescription..but ill try.
Sumit – thank you so much for sharing you journey. ❤️ I’m so sorry you are struggling with all of this. I’ve personally not had a problem with oxalates, however others have reported oxalate issues, and oxalates turned out to be at the root of one of my client’s joint pain and urinary symptoms. So if you are doing everything right, still struggling and have symptoms of oxalate sensitivity then this is something to look into. Hope this helps!
Loys of lemon water help keep the stones at bat and when having kidney pain from it the lemon water will be tour your friend
Stella, thank you fo rsharing what has worked for you.
I thought that cooked spinach had less oxalates than raw spinach. Your chart in this article shows the opposite.
I have Hashimoto’s and a few years back I was making green smoothies every morning for breakfast…. with lots of spinach. My hair started falling out a lot!!! That’s when I found out that high oxalates can cause some people with Hashimotos to lose hair.
Patti – thank you so much for sharing your journey. ❤️ I appreciate you sharing this with me! My team and I have looked into this and found that some studies do show that boiling may reduce oxalate content (https://pubmed.ncbi.nlm.nih.gov/15826055/), but other cooking methods, such as steaming and baking do not. The Harvard study that our chart source is based off of likely measured the oxalate content using baking/steaming methods, as these are more common ways of cooking spinach. Additionally, density changes when spinach is cooked and may account for the higher amounts in 1 cup raw vs 1 cup cooked (steamed or baked) spinach.
Dr. Wentz ,
Thanks for talking about oxalates. I have UC, thyroid antibodies, bad candida, oxalate issues, mold toxicity, gut dysbiosis, acid reflux, probable sibo, kidney and liver issues, osteopenia, and more! I’ve seen so many functional medicine doctors and spent so much money. What does one do with alllll of these issues and contradictions to each other?? I wanted to try ldn but probably shouldn’t now because of candida and mold. I’m so underweight because I’m sensitive to everything now and no one can help me with everything. Western and functional medicine has failed to be able to help me.
Kristin – thank you so much for sharing your journey. ❤️ I’m so sorry you are struggling with all of this. I understand how hard it can be to find the right practitioner. I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
In your third paragraph is says, “people with Hashimoto’s had a lower incidence of oxalate crystals, especially in the parts of their thyroid gland that were inflamed!”. Did you actually mean “higher incidence”? Just checking to make sure I’m understanding correctly.
Hello – thank you so much for bringing this to my attention. You are correct and I am so sorry for the error.
there are so many low oxalate cookbooks. Can you recommend one? Also how do you feel about the fact that goitergens are included in a light diet?
Beth, thank you for following. Sorry, I don’t have a specific Oxalate cookbook to recommend. Following the guidelines in the graphics and the article can help. As for goitrogens, there is a myth that foods known as goitrogens, such as cruciferous vegetables, are not good for those with Hashimoto’s. Iodine deficiency is not widespread in people with Hashimoto’s, so eating cruciferous vegetables (unless you are sensitive to them) is perfectly healthy for people with Hashimoto’s and should not impact thyroid function. In the case that a person does have hypothyroidism due to iodine deficiency, he/she can still enjoy crucifers as long as they are cooked or fermented. Cooking/fermenting will break down the iodine blocking content. Here is an article that I hope is helpful:
https://thyroidpharmacist.com/articles/what-are-goitrogens-and-do-they-matter-with-hashimotos/
In Italy there is also a food supplement (actually a plant) called Spaccapietra which means stonebreaker in English.
Renate, thank you so much for sharing.