For those with Hashimoto’s, optimizing thyroid hormones is one of the keys to feeling our best, while we work to remove the underlying triggers (such as nutrient deficiencies, stress and infections) that caused and/or are worsening the autoimmune component of the condition.
The right thyroid hormone medication can reduce thyroid antibodies and slow down the progressive thyroid destruction, as well as provide the energy needed to continue to work towards one’s health. Thyroid hormone medications can also reduce the size of thyroid goiters and nodules, as well as reduce the likelihood of thyroid cancer.
That said, thyroid hormone medications are very individualized! What works for your friend may not be your best option, leaving you with lingering symptoms such as fatigue, anxiety, brain fog, and excess weight. And just because your doctor may be most familiar and comfortable with prescribing one particular type of thyroid hormone medication, doesn’t mean you should settle for his/her preferred medication if that particular prescription just isn’t working for you.
As a pharmacist, I want to empower you to be your own best thyroid advocate. Taking the right thyroid hormone medication for you can be a game changer for how you feel and progress. But how do you know which medication might be best for you?
Read on to learn more about:
- A review of the available thyroid hormone options
- How to get the best results from your current medications
- How to improve your T4 to T3 conversion
- How to switch medications, if you need to
Medications to Balance Thyroid Hormones
Choosing the best medications starts with an understanding of our symptoms and labs.
While our symptoms can provide a clue that something is off, our labs can tell us if the reason we’re feeling unwell could be due to our medications. Labs will provide information on whether we are absorbing our medications, whether we are on a correct dose of medications, as well as whether our body has issues converting T4 to T3 (meaning a T4-only medication may not be optimal and/or we may need to address the conversion issues — more on that in this article).
All too often, conventional doctors simply test one’s TSH (thyroid stimulating hormone) and T4 levels (the amount of thyroid hormone circulating in your blood). However, TSH is a pituitary hormone, and doesn’t tell us what level of hormones we have available to use within the rest of the body.
For this reason, it’s important to have a full thyroid panel done, which will also help you and your practitioner determine the appropriate medication for you.
A full thyroid panel checks one’s TSH, free T4, free T3, and thyroid antibody levels.
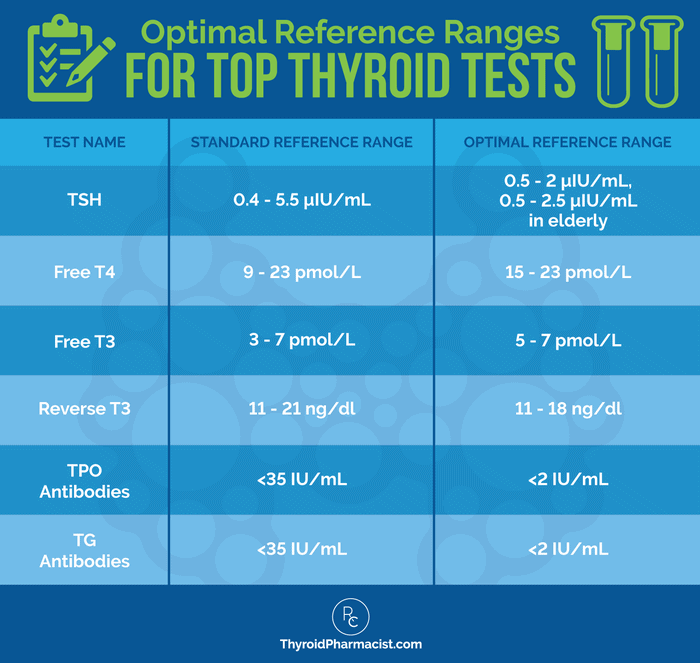
- TSH: The thyroid stimulating hormone, or TSH test, is used as a screening test for thyroid disease, as well as a test for monitoring the correct dose of medication needed for an individual. TSH is elevated in cases of hypothyroidism. While conventional practitioners may have lax reference ranges, functional medicine practitioners have further defined the optimal reference range in which most patients will feel their best.
- Recommended test: TSH
- Optimal reference range: between 0.5-2 μIU/mL
- Free T4 & Free T3: T4 (thyroxine) and T3 (triiodothyronine) are the two main thyroid hormones. Some clinicians may only test for T4, but both are important to test for and should be in the optimal ranges. If the T4 is optimal, but the T3 is out of the optimal range, you know that your body is not making enough T3 hormone from the T4. It is important to monitor your T4 and T3 levels when adjusting your thyroid medications.
- Reverse T3: The reverse T3 (rT3) test measures how much of the free active T3 is able to bind at thyroid receptors. RT3 is produced in stressful situations and binds to thyroid receptors, but turns them off instead of activating them. The rT3 test is sometimes used to identify cases of poor T4 to T3 conversion, as well as thyroid symptoms that are due to adrenal stress, instead of thyroid malfunction or autoimmunity.
- Recommended tests: Reverse T3 (rT3)
- Optimal rT3 reference range: 11-18 ng/dl
- Thyroid Antibodies (TPO, TG): The presence of thyroid antibodies indicates that the thyroid gland has been recognized as a foreign invader by the immune system and that the thyroid gland is under attack. Up to 95 percent of people with Hashimoto’s will present with elevated thyroid antibodies. However, they can be reduced as we work to address the root causes of the autoimmunity behind Hashimoto’s.
For a detailed discussion and guidance on understanding your thyroid labs, please visit my article Top 10 Thyroid Tests and How To Interpret Them.
Symptoms or Thyroid Hormone Medication Side Effects
I put symptoms and side effects for all thyroid medications in the same category. This is because side effects of most thyroid hormones are primarily due to overmedication or inadequate doses of medication. That said, some individuals can have additional reactions to the fillers in the various medications.
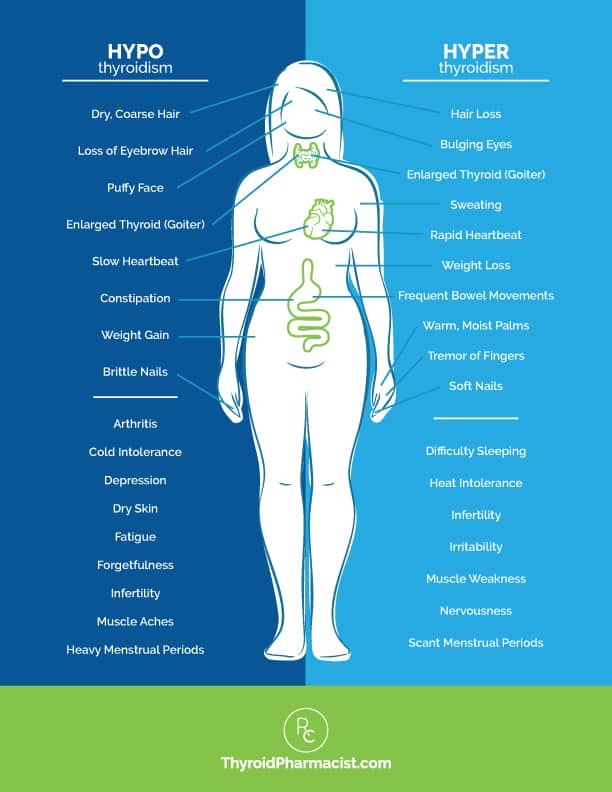
Overmedication can cause hyperthyroidism due to therapeutic overdose. (Symptoms may include rapid or irregular heartbeat, nervousness, irritability or mood swings, muscle weakness or tremors, diarrhea, menstrual irregularities, hair loss, weight loss, insomnia, chest pain, and excessive sweating.) The cardiovascular and central nervous system effects are particularly serious. It’s important when starting medications (and while your doctor is finding the right dose for you) that you report all symptoms and have your labs repeated every four to eight weeks, or more often, if you have any of the above symptoms.
When not enough hormone is provided, people may continue to experience symptoms of hypothyroidism such as heavy menses, hair loss, dry skin, loss of eyebrow hair, infertility, constipation, slowed digestion, joint pain, depression, brain fog, fatigue, weight gain, and even miscarriages.
See the image below for the consequences of hypothyroidism and hyperthyroidism.
Safety
Thyroid medications are generally well tolerated and safe for those with hypothyroidism. However, there are some precautions for certain populations.
First and foremost, thyroid hormones should only be used for those with hypothyroidism, not for people with normal thyroid function who are wanting to lose weight.
Additionally, those with adrenal insufficiency due to Addison’s disease, should not start thyroid hormones for hypothyroidism until their condition has been well controlled. People with Addison’s disease can have low levels of cortisol, and thyroid hormones can increase how quickly they are removed from the body, leading to a dangerous situation.
In older individuals and those with cardiac issues, thyroid hormones need to be started at a lower dose, and increased slowly, as well as monitored frequently.
All thyroid medications have precautions relating to many different underlying health conditions. You will want to review your particular health situation with your practitioner and have them review any potential concerns with you.
Additionally, most thyroid medications react with other medications and may require you to space them apart when taking them.
Thyroid medications are generally safe for most women during pregnancy and while breastfeeding (they are considered category A, which is the safest category). Taking them can help prevent miscarriage, infertility issues, and even developmental disabilities. (Note: Most women will need to increase their dosage in the first trimester. If you’re planning a pregnancy, you may also need to increase your dosage; you’ll want to have your labs rechecked and work with your doctor to determine what is best for you and your baby.)
Dosing Considerations
You’ll want to have your full thyroid panel measured before and during dose titration trials. While trying to get on the right dosage of medication, you will want to test your thyroid labs every four to six weeks. Once you’re symptom-free, and if you’re stabilized on your new thyroid medications, every three months to one year may then be appropriate for testing and monitoring your thyroid levels.
Generally, the rule of thumb I like to consider is that if your TSH is elevated, and you have thyroid symptoms, you may benefit from starting thyroid medications.
If you are already on thyroid medications, and have levels of TSH, T3 and/or T4 outside of the optimal ranges, you may benefit from further tweaking or optimizing how you take your medications, as well as considering a dose increase/decrease and/or medication change, depending on the circumstances.
Choosing Your Best Medication
Choosing your best medication also requires a little self-assessment.
- Do you have food sensitivities to gluten, lactose or other ingredients such as corn or grains (which are often found in thyroid meds)?
- Do you take medications for stomach acid issues (acid blockers don’t play well with many thyroid meds)? Do you have gastrointestinal or liver concerns?
- Do you have a morning habit that prevents you from absorbing most thyroid medications? (Some medications need to be taken away from breakfast, other supplements and coffee. I’ve been personally guilty of the latter, courtesy of #mamalife, so no judgement here.) All of these can impact how well you consistently absorb your particular thyroid hormone medication, which will directly impact its effectiveness.
- Do you have low ferritin, a selenium or zinc deficiency, or gene variations in your deiodinase genes that may prevent you from properly converting T4 to T3?
Overview of Thyroid Hormone Medication Options
Medication options to balance thyroid hormones include:
- T4-only medications
- Generic levothyroxine tablets
- Synthroid tablets
- Levoxyl tablets
- Tirosint gel caps
- Tirosint liquid (Tirosint SOL)
- Compounded T4 medications
- T3-only medications
- Liothyronine
- Cytomel
- Compounded T3 medications
- T4/T3 combination medications
- WP Thyroid (Note: This medication has been unavailable since 2021, following a voluntary recall in 2020)
- Nature-Throid (Note: This medication has been unavailable since 2021, following a voluntary recall in 2020)
- Armour Thyroid
- Compounded T4/T3 medications
To better understand the differences in these available thyroid medications, we need to briefly talk about a few of the thyroid hormones we have in our body. The three hormones I’ll primarily talk about in this article are T3, T4, and TSH.
Triiodothyronine (T3) is our primary biologically active thyroid hormone. About 20 percent of our T3 hormone comes from thyroid secretion directly, while the remaining 80 percent is produced when Thyroxine (T4) is naturally converted to T3 within our bodies. While T4 is 300 percent less biologically active than T3, it is critical to our body’s ability to produce adequate and healthy levels of the needed T3.
It is the low levels of T3 and T4 that signal the release of thyroid stimulating hormone (TSH). When TSH remains too high, we know we have hypothyroidism, and that is the conventional measure that many doctors solely look at.
On the opposite end of the spectrum, continued high levels of circulating T3 and T4 stop the release of TSH. When TSH remains too low, we suspect a hyperthyroid problem.
In people with normal thyroid function, TSH levels still often fluctuate (such as in cases of pregnancy, illness, diabetes, other underlying conditions, chronic stress, or nutrient deficiencies).
Most conventional doctors will prescribe synthetic T4 medications, so many people are only familiar with T4-containing thyroid medications tablets such as levothyroxine (generic), Synthroid®, Levoxyl®.
However, there are additional, lesser known T4 formulations such as Tirosint® gel caps, Tirosint®-SOL liquid and compounded T4 capsules, that may lead to better outcomes for some individuals.
Additionally, there are T3-only medications such as liothyronine (generic), Cytomel®, and compounded T3, which offer the more active thyroid hormone, T3, to be taken directly.
Last but not least, there are combination T4/T3 medications which can be naturally derived from the thyroid glands of animals, often referred to as Natural Desiccated Thyroid (NDT) medications (examples being Armour® Thyroid, Nature-Throid®, and WP Thyroid®), as well as versions of T4 and T3 that are compounded by compounding pharmacists. Thyrolar, a manufactured synthetic version of T4/T3, was previously available in the United States. However, it has been on long term back-order since 2013.
Let’s look at how these medications are different and who might be best served by the different types. We’ll start with one of the most prescribed drugs in the United States, the generic T4 medication levothyroxine.
T4 Medications (Levothyroxine)
As there are various manufacturers and dosage forms of T4 medications, I’m going to focus on the guidelines that apply to all T4 medications first, and then I will go into differences between the various versions of levothyroxine.
Description: Levothyroxine is the generic name of a synthetic version of the thyroid hormone Thyroxine, referred to as T4.
In an extensive survey done in 2014 (and published in 2018), it was the second most prescribed drug in the United States. It is among the most widely prescribed medications in the world.
When a drug becomes “generic,” this means that the pharmaceutical formulation has lost its patent, and this allows many manufacturers to make it, instead of just one pharmaceutical manufacturer having exclusive rights to it.
Various pharmaceutical companies offer their own versions of levothyroxine tablets under specific brand names, including: Synthroid®, Levothroid®, Levoxyl®, Unithroid® and Thyro-Tabs® (in the United States), Eltroxin® (in Canada), Euthyrox® (in the EU), and Oroxine® or Eutroxsig® (in Australia).
Levothyroxine is also available as Tirosint® gel caps, Tirosint®-SOL liquid, as well as compounded T4 capsules.
Dose: T4-containing medications are usually started at a dose of 25-50 mcg per day. The medications are then adjusted to the target dose by 25 mcg per day, every four to six weeks, depending on the person’s thyroid function tests and symptoms.
The maximum recommended dose is 300 mcg/day. Most negative side effects have to do with incorrect dosage (this is true of all thyroid hormone meds, as I mentioned at the beginning of this article). It is important to start low and go slow for that reason. Your practitioner should work with you and adjust the starting dose to best fit your particular health profile.
Pros: As a well-established prescription medication that is off-patent, levothyroxine is a low cost option and is typically well tolerated by most patients. Most conventional doctors are most familiar with and will prescribe T4 medications, and many people will do well on them once they are on the correct dose.
Potential Cons: There is one main issue that applies to all types of T4-only medications (whether branded, generic, gel cap, or liquid), and this has to do with the fact that T4 is a prodrug, and needs to be converted to T3, the more active thyroid hormone in the body. This reaction doesn’t happen equally in every person, and thus some are not able to adequately convert T4 to T3 within their body. This can result in inadequate treatment and ongoing symptoms.
Some Patients Feel T4 Medications Often Result in Inadequate Treatment
While many people do very well on T4-containing medications once they are dosed appropriately and stabilized, a 2019 review of the research found that many people taking T4 medications simply aren’t happy with their results, and that more than a third of patients remain inadequately treated (based on labs and symptoms) despite levothyroxine therapy. In particular, 5-10 percent of people taking T4 replacement – even if they normalize their TSH level – are found to have impaired psychological well-being, anxiety, or depression.
As a pharmacist, I would ask the following questions in this situation.
- Is your TSH normal, but not optimal? Most people feel best with a TSH between 0.5-2 μIU/mL, so you may need a dose adjustment.
- Is your TSH inconsistent and/or fluctuating? If so, you may not be absorbing your medications due to fillers, GI issues, or interference from foods, medications, and supplements. (See below.)
- Are your levels of T3 and reverse T3 optimal? If not, you may want to look at conversion issues. In those taking T4, we can work on optimizing your conversion and/or consider a therapy that includes both T3 and T4.
- Do you have root causes (like adrenal issues!) that need to be addressed?
Unresolved Root Causes Can Keep Us Symptomatic
One reason we may not have a 100 percent response to levothyroxine is because levothyroxine does not address the underlying root causes of the condition, which can contribute to other remaining symptoms. I’ve written extensively about root causes in other articles, and the importance of not just taking medications but working on our overall health through lifestyle changes and root cause medicine, so to keep this article from being a whole ‘nother book, I’ll focus on the pharmacology related issues. 🙂
T4 to T3 Conversion Issues
An important reason why some individuals may not have a full therapeutic response to T4-only thyroid hormones (even when dosed and taken correctly), can be due to the person’s ability to convert T4 to T3, so let’s talk more about that. (This is not just specific to the generic version of levothyroxine, by the way. It applies to all T4 medications.)
This is because levothyroxine contains the less-active but longer-acting T4 hormone. The T4 molecule is considered a prohormone, as it is less physiologically active than T3 and needs to be converted to T3, the more active thyroid hormone, by our bodies. T3 is sometimes called our “go” hormone because it tells our body to boost metabolism, grow hair, and create more energy.
In 2014, Dr. Wilmar Wiersinga, a Dutch endocrinologist and top thyroid researcher, stated that: “Impaired psychological well-being, depression or anxiety are observed in 5-10 percent of hypothyroid patients receiving levothyroxine, despite normal TSH levels. Such complaints might hypothetically be related to increased free T4 and decreased free T3 serum concentrations, which result in the abnormally low free T4/free T3 ratios observed in 30 percent of patients on levothyroxine. Evidence is mounting that levothyroxine (T4) monotherapy cannot assure a euthyroid state in all tissues simultaneously, and that normal serum TSH levels in patients receiving levothyroxine reflect pituitary euthyroidism alone.” In other words, this study suggested that T4-only therapy might not be enough to address the symptoms of hypothyroid patients, especially those related to mental well-being.
Some people have challenges taking a T4 medication, as they aren’t able to properly convert T4 to T3. This improper conversion can result in lingering thyroid symptoms or even new ones. The conversion from T4 to T3 can be impeded by numerous factors, including nutrient deficiencies, stress, infections, and impaired liver and gut activity.
Furthermore, in recent years, pharmacogenomics (the study of how a person’s genes impacts their response to medications) has helped us determine which patients may best benefit from particular medication due to their unique genes. From a pharmacogenomic standpoint, polymorphisms (variations) in the DIO2 deiodinase gene, which codes for the deiodinase 2 enzyme (Thr92Ala), can also lead to inadequate conversion of T4 to T3.
The thyroid gland plays a minor role in the daily production of T3, with the bulk of it being produced by two deiodinase genes (D1 and D2) that convert T4 to T3 outside the thyroid tissue. Thus, variations in these genes can impact how well the body is able to produce T3. Studies have shown that hypothyroid patients maintained on levothyroxine, depend on D2 for more than 80 percent of all their T3 needs. Thus, they are at much greater risk to develop low serum T3 during caloric restriction when the body acts to limit caloric expenditure, and temporarily slows metabolic function.
In one study suggesting a genetic link to poor ability to convert T4 to T3, a polymorphism in the DIO2 gene was found to be linked to who will or won’t respond well to T4 therapy (due to how well their body converted T4 to T3). Findings, however, are still viewed as controversial, and more studies are required.
If you have challenges converting T4 to T3, you might want to consider a genetic test with Nutrition Genome.
Other potential factors impacting T4 to T3 conversion include:
- Aging
- Alcohol
- Chemotherapy
- Cigarettes
- Deiodinase gene variation
- Diabetes
- Fasting
- Growth hormone deficiency
- Heavy metals
- Iodine excess
- Kidney and liver disease
- Liver backlog
- Low ferritin
- Low progesterone
- Medications
- Nutrient depletions
- Obesity
- Pesticides
- Radiation
- Stress
- Soy
- Surgery
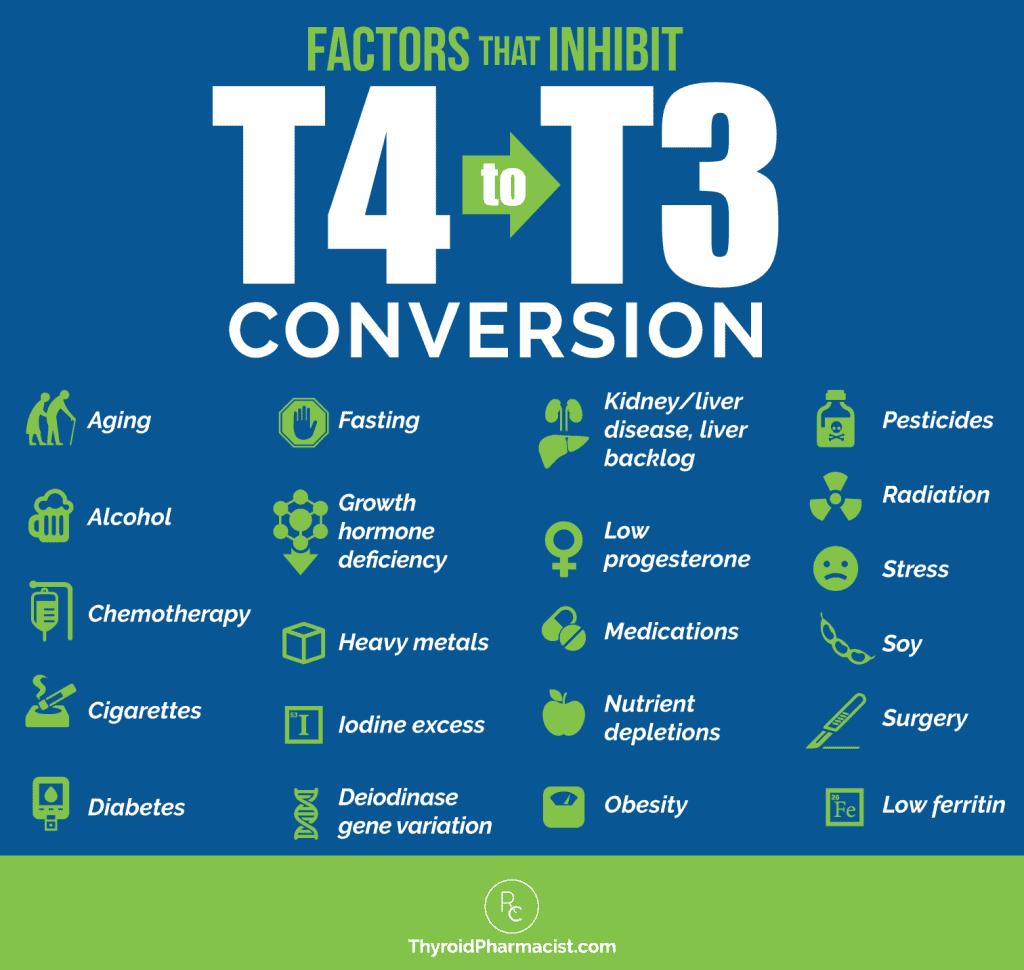
As you can see from the graphic, a lot of the reasons people have poor conversion are also common triggers for Hashimoto’s. I believe this is one reason many of my clients do not do well on T4-only medications.
How to Make Your T4 Medications Work for You
There are a few steps that you can take to ensure that you are getting the most out of your T4 thyroid medications so that they work optimally for you.
1. Ensure ferritin is optimized: As mentioned earlier, T3 is sometimes called our “go” hormone because it tells our body to boost metabolism, grow hair, and create more energy. Without proper levels of ferritin (the iron storage hormone), the conversion of T4 to T3 can be impeded.
2. Support your adrenals: Stress is another common cause of low T4 to T3 conversion. Under stressful situations, T4 gets converted to reverse T3 instead of T3. Reverse T3 is an inactive molecule related to T3, but without any physiological activity. (It essentially just takes up space!) In the case where a lot of reverse T3 is produced, adding a combination product that contains T3 will help ensure that the right hormone is getting to the right receptors.
3. Support your liver: Most T4 to T3 conversion takes place in the liver, and when the liver is impaired, usually due to an accumulation of toxins or lack of nutrient absorption, we are unable to complete the process. Oftentimes, focusing on a liver support protocol, which includes eliminating food sensitivities, removing environmental toxins, and adding in supportive nutrients, can improve T3 levels.
4. Consider supplementing with zinc and selenium, which support the conversion of T4 to T3. Thyroxine (T4) is produced by the thyroid gland in ample amounts, but is relatively biologically inactive. Therefore, triiodothyronine (T3), the biologically active thyroid hormone, must be produced by a hormone conversion process, converting T4 to T3. The antioxidant selenium is required during this conversion process, its role being to neutralize the toxic build-up of hydrogen peroxide (H2O2) which is produced as a by-product of the hormone conversion.
A depletion in zinc also prevents the conversion of the T4 hormone into the active T3 version. This could lead to symptoms like hair loss, fatigue, and weight gain, even while taking thyroid medications like Synthroid.
Check out the articles linked above to learn more about supplements to optimize selenium and zinc levels.
5. Consider taking probiotics. We know that everyone with Hashimoto’s (and autoimmune conditions in general) have some degree of intestinal permeability. Given that about 20 percent of the conversion of T4 to T3 takes place in the gut, improving gut health can help with the conversion process and improve T3 levels. For many, the problem lies in the imbalance of beneficial to opportunistic bacteria in the gut microbiome, and getting a quality probiotic on board can help improve gut health and increase T3 levels.
But what if you find yourself needing to tweak your T4 medication (multiple times!), or you continue to experience symptoms or poor lab results? You may want to consider adding a T3 medication or switching to a combination T4/T3 medication instead, to address the conversion issue.
This underlying conversion issue also points to why using only a person’s TSH level (the conventional measure typically used) to determine how well their medication is working for them, is not truly reflective of what is going on with their thyroid health. A full thyroid lab panel is needed. When lab results come back showing that free T3 is below or within the low end of the reference range, while free T4 is above the reference range or in the optimal upper part of the reference range, this suggests that the individual might be dealing with impaired conversion. It is so important to know.
Beyond optimizing conversion, some individuals may benefit from switching to T4/T3 medications. Of the readers I’ve surveyed, up to 60 percent have felt better taking a combination T4/T3 medication, while around 40 percent have felt better on a synthetic T4 medication. I used to routinely recommend T4/T3 medications for my clients, however, three of the four available brands have recently been recalled in the United States. We will discuss T4/T3 medications later in this article, including the options that are still available.
Last but not least, people may have suboptimal results to T4 medications due to inconsistent absorption. Let’s talk about this next.
Strict Adherence Required for Consistent Absorption and Effectiveness
Studies (and my own clinical observations) have found that many people don’t adhere to thyroid medication usage guidelines. They won’t take it on an empty stomach (an hour before breakfast), and they’ll take it with their morning coffee or their acid reflux medication, without the required wait time. All of this can impact their medication’s absorption and its effectiveness. If adherence is an issue for you, the best T4 medication might be the hypoallergenic T4 medication, Tirosint, which I’ll talk about in a moment.
I am always a bit dismayed to hear from people that they did not know about the impact on their medication’s effectiveness by not following these basic guidelines, but research has found that ingesting food with T4 medication (tablets) decreases its absorption from approximately 80 percent to 40 percent. Coffee impacts absorption, too. It’s all about the gastric pH level and how foods, drinks and medications (including acid reflux/acid blocking medications) reduce the acid levels within the gastrointestinal system. Without this acidity, tablets take longer to break down, and there are direct effects on absorption that occur.
Thyroid medications have a narrow therapeutic index, meaning that they are “goldilocks” hormones, and careful dose titration is needed to get things “just right.” Doses that are incorrect by just a tiny amount can result in symptoms from over-treatment or under-treatment. So the above issues (generics’ potency differences, fillers, drinking coffee when taking your medicine or popping meds for acid reflux) can all result in ineffective thyroid treatment.
In order to overcome the absorption issues, I recommend the following:
- Follow guidelines. Take your medication consistently at the same time each day with a glass of water, 30 minutes before having food, coffee and other medications or supplements. Avoid magnesium, calcium, and iron supplementation within four hours of taking thyroid medication. Taking your medication with lemon water may help with absorption.
- Consider Tirosint and Tirosint SOL — these formulations can be taken with food and even coffee! (More on Tirosint options further on in this article… keep reading!)
Adverse Reactions and Medication Ineffectiveness Due to Fillers
I have found that some of my clients experience sensitivities and adverse reactions to the many inactive ingredients or fillers found in their T4 medications. These are added as bulking agents used to stabilize the tablets, as coloring agents, as preservatives, or to aid in the manufacturing process in some way. Many have been shown to potentially cause adverse reactions, as well as affect the absorption rate and effectiveness of the very medication meant to help the thyroid.
Most generic levothyroxine products contain lactose (the generic manufactured by Mylan is, however, lactose-free) and not all are gluten-free (examples: Lannet does not contain gluten, per se, but the maker does not certify it as gluten-free; Mylan does certify their product as gluten-free).
Can small amounts of these types of fillers really be problematic? Yes! Many people with Hashimoto’s have sensitivities to these ingredients no matter how small the exposure. In my 2015 survey of 2,232 readers, 57 percent of respondents said they reacted to or avoided all dairy, and over 75 percent avoided gluten due to sensitivities and reactions. Other fillers that are commonly found in T4 medications may include confectioners’ sugar (contains corn starch, and corn is another food sensitivity for many people with Hashimoto’s), sucrose, talc, and dyes. Why would we want these inactive filler ingredients in our thyroid medication?
If you are following all of the “absorption rules” but still having fluctuations in your TSH and symptoms such as anxiety, you may be reacting to the fillers in your medications. Fillers can cause malabsorption of the medications as well as digestive symptoms. In my experience, reactions to fillers are more common in those with liver congestion, food sensitivities, celiac disease, H. pylori, SIBO, parasites, and other root causes.
- You can look up the latest and greatest on medication fillers at glutenfreedrugs.com (this info actually changes frequently, so it is worth checking) to ensure that your medications are gluten-free and free of fillers that may be reactive for you.
- Alternately, consider switching to Tirosint and Tirosint SOL — these formulations have minimal fillers.
Potency and Ingredient Inconsistency with Generic T4 (Unbranded) Versions
While generic availability is a positive thing because it reduces the cost of most medications, with medications that have a narrow therapeutic index, like thyroid hormones, generic versions open up the door for inconsistent thyroid hormone levels with every refill.
This is because the dosages and fillers may vary ever so slightly between each manufacturer. Different pharmacies may dispense different manufacturers, and even the same pharmacy may switch between manufacturers from month to month. For patients taking generic thyroid hormones, it’s important to note the name of the manufacturer as well as request that their refills be filled with that particular manufacturer’s version of levothyroxine. While most pharmacists and physicians actually recommend keeping on T4 hormones made by the same manufacturers (instead of switching between brands), this doesn’t always happen in the real world.
Generic prescriptions suffer from a potential potency and ingredient inconsistency issue as a result of having multiple manufacturers providing the drug to the same pharmacy. The U.S. Food and Drug Administration (FDA) requires the potency of all thyroid hormone medications to fall within a range of 95 to 105 percent, but different manufacturers can pick what potency within that range they will provide. Different makers also include different fillers.
This can result in issues when it comes to taking a generic, as you don’t know which manufacturer (what potency and what inactive ingredients) you might be getting with each refill. With one refill, you may get a pill at 95 percent potency, and the next time, due to it originating from a different manufacturer, you might get pills at 105 percent potency. This can affect the consistency of how much thyroid hormone you are getting (and absorbing), which can affect both your symptoms and your labs. Additionally, with one refill, you may be getting a filler that is reactive in your body and prevents proper absorption.
However, brand name prescriptions are manufactured by only the branded maker (like Synthroid), so you will always get the same potency and the same inactive ingredients with each refill of brand medication.
We know that even small differences in dose and absorption levels may lead to adverse reactions and even therapeutic failure. The American Association of Clinical Endocrinologists, the Endocrine Society, and the American Thyroid Association (ATA) recommend the consistent use of a single preparation of brand-name levothyroxine over generic preparations for this reason.
How to Overcome:
- One way to overcome this issue is to note the manufacturer of your levothyroxine and insist that your pharmacy only use this manufacturer for all of your refills. Then, verify that the correct manufacturer was indeed dispensed when you pick up your prescription. I generally recommend sticking to one pharmacy for all of your prescriptions, to ensure your drug interactions are properly monitored; and as long as your pharmacy is able to continue providing the same manufacturer of levothyroxine to you, you will want to continue getting your refills there.
- If needing to switch pharmacies, you will also need to inquire that the new pharmacy can order the levothyroxine made by the same manufacturer you have been using.
Branded Versions of Levothyroxine
There are various branded versions of levothyroxine tablets, and each one has slight differences in absorption and fillers. The main takeaway from this section is that if you feel well on one particular brand, you will want to stick with it. If you feel unwell on that brand, you may want to consider adjusting your dose or how you take the medicine, or consider switching to a different version of levothyroxine (which may be available in tablets, gel caps, or liquid formats).
Synthroid
Description: Synthroid is a branded version of levothyroxine and is the most commonly prescribed medication for hypothyroidism. In 2013, Synthroid was the number one prescribed drug overall in the United States.
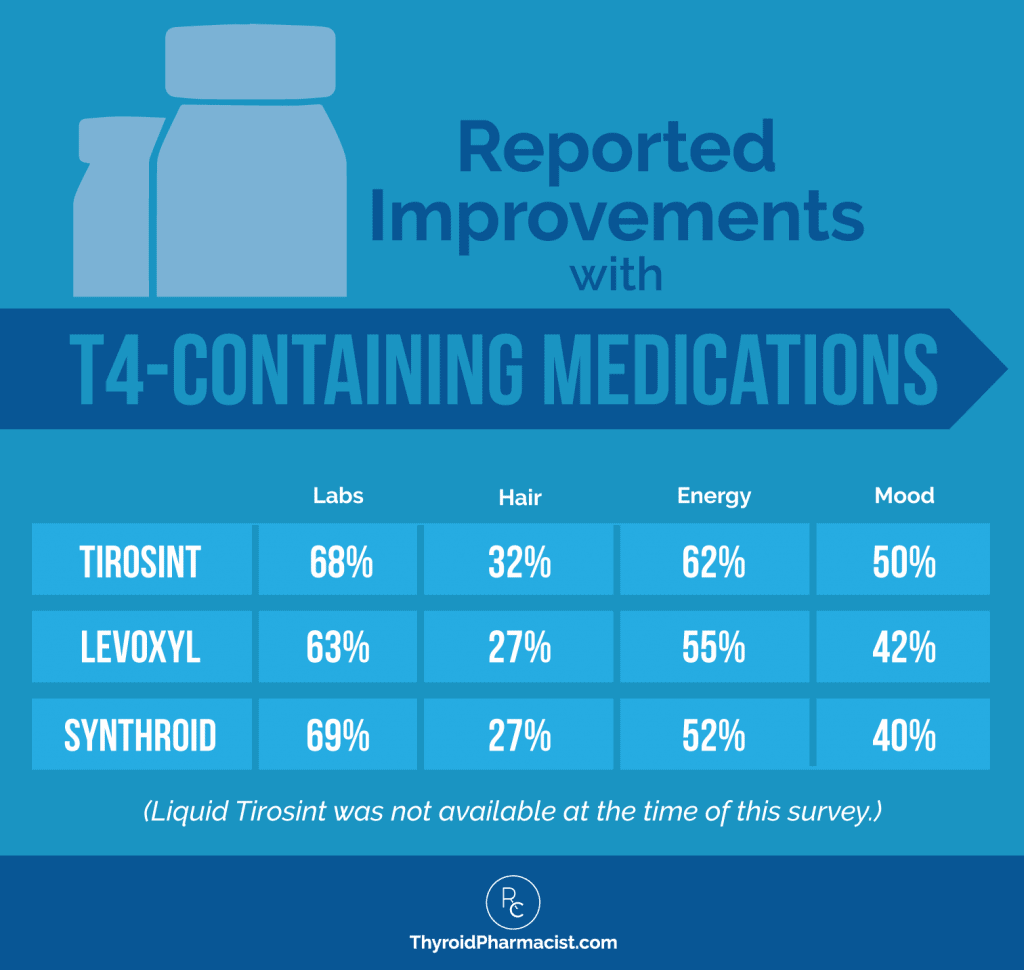
In my reader’s survey, some 43 percent of respondents said they felt better on Synthroid. Additionally, Synthroid results were the best (of other T4 medications) for improvements in labs, with 69 percent experiencing improvements in their labs when taking Synthroid. Another 52 percent saw improvements in energy, 27 percent saw improvements in hair loss, and 40 percent saw improvements in mood.
Differences between generic (levothyroxine) and Synthroid:
The earlier concerns relating to the issue with fillers, the need for adherence to usage guidelines, and the potential ineffectiveness due to poor T4/T3 conversion, apply to Synthroid as well. Conventional doctors will be very familiar with this top branded medication.
Pros:
- Branded drugs like Synthroid, unlike the generic levothyroxine, do not vary in potency or fillers, as they come from a single manufacturer.
- It appears to be gluten-free, according to the Gluten Free Drugs website.
Potential Cons:
- It is more expensive than the generic version.
- Synthroid’s fillers contain lactose, which may cause some people to experience absorption challenges (especially those with dairy sensitivities, lactose intolerance, or lactose allergies).
- Synthroid is not certified as gluten-free. I have heard from multiple patients with Hashimoto’s and/or celiac disease, who were adhering to a gluten-free diet, that they have had similar symptoms to gluten exposure when taking Synthroid. I actually put in a request to the maker of Synthroid (Abbvie) to resolve this issue back in 2016.
- Synthroid does contain other fillers (on top of lactose) which may trigger a negative response, including confectioners’ sugar (contains corn starch), magnesium stearate, talc, povidone, and color additives.
Levoxyl
Description: Levoxyl is another branded version of levothyroxine.
In my reader’s survey, 25 percent of respondents said they felt better on Levoxyl, with 63 percent experiencing improvements in their labs. Another 55 percent saw improvements in energy, 27 percent improvements in hair loss, and 42 percent improvements in mood.
Differences between generic (levothyroxine) and Levoxyl:
The earlier concerns relating to the issue with fillers, the need for adherence to usage guidelines, and the potential ineffectiveness due to poor T4/T3 conversion, apply to this branded drug as well. Conventional docs will be familiar with this branded medication.
Pros:
- Unlike the generic levothyroxine, branded drugs like Levoxyl do not vary in potency or fillers, as they come from a single manufacturer .
- Levoxyl is lactose-free.
- It is gluten-free (but not certified).
Potential Cons:
- It is more expensive than the generic version.
- Levoxyl contains five inactive ingredients, including an antacid (which we know can impact the medication’s absorption!). Any of these fillers can cause adverse reactions in people who are sensitive.
- It is not certified as being gluten-free.
Tirosint – Levothyroxine Gel Caps
Description: Tirosint is a newer thyroid medication that is a hypo-allergenic version of levothyroxine. I recently wrote an entire article focused on Tirosint. In my survey, 26 percent of respondents said they felt better taking Tirosint. Out of those that switched to Tirosint gel caps (this was the only form available in 2015; recently, the maker introduced a liquid version as well, which contains just three hypoallergenic ingredients: levothyroxine, glycerol, and water), 68 percent saw an improvement in their labs, 62 percent saw an improvement in energy levels, 32 percent an improvement in hair loss, and 50 percent saw an improvement in mood.
Because of how quickly and consistently Tirosint is absorbed, it has also been found to be a better option for people who have certain gastrointestinal challenges (including infections like H. pylori and SIBO, both common triggers for people with Hashimoto’s), who are taking antacids/acid blockers/PPIs, or who are otherwise experiencing low stomach acid.
Dose: Tirosint gel caps are available in 12 different dosage strengths, ranging from a 13 mcg dose to a 200 mcg dose. Because this medication is more readily absorbed than other forms of levothyroxine, some people may find that they require a smaller dosage of Tirosint to keep thyroid hormones within optimal range.
Pros:
- As a branded medication, there are no potency or filler variations.
- Tirosint contains no gluten, lactose, or reactive fillers.
- It has been shown to be consistently absorbed by people with co-occurring digestive and gastrointestinal conditions (including H. pylori infections, celiac disease, other gastric pH-related issues, and malabsorption issues such as IBS), with patients gaining significant symptom improvements.
- Tirosint minimizes negative absorption effects relating to a person taking medications such as PPIs for GERD/acid reflux, even with their thyroid medication.
- It may be better absorbed, even when taken with a morning cup of coffee. Studies have shown that Tirosint is better absorbed with coffee compared to other forms of T4. In fact, new research has found that gel caps and liquid forms are unaffected when taken with coffee (unlike tablet formulations). For some people, it may be better absorbed than other forms of levothyroxine when taken with breakfast.
Potential Cons:
Just like with all T4 medications, the effectiveness of Tirosint may be impacted if a given individual is experiencing poor T4/T3 conversion. Here are some additional things to consider:
- As a newer and branded drug, it carries a higher cost, which means some insurance companies may penalize patients with a higher copay, while others may not pay for it at all (although the manufacturer offers a variety of programs to help with that — read more about that here).
- Conventional doctors may not be familiar with or have limited experience prescribing Tirosint, and may be reluctant to do so.
Tirosint-SOL – Levothyroxine Liquid
Description: Tirosint-SOL is a liquid form of Tirosint gel caps and only contains two inactive ingredients (glycerol and water). While the original Tirosint formula is considered to be hypoallergenic, having even fewer ingredients makes for a great T4-only option for those who may have difficulty swallowing pills or who may be allergic to the porcine in the gel caps.
Dose: Tirosint-SOL is packaged in monodose ampules in 12 different dosage strengths, including a 13 mcg/mL dose. It can be administered either directly into the mouth or diluted in a glass of water.
Pros: As a branded medication, there are no potency or filler variations.
- Tirosint-SOL contains the fewest fillers of all thyroid medications on the market.
- It has been shown to be consistently absorbed by people with co-occurring digestive and gastrointestinal conditions (including H. pylori infections, celiac disease, other gastric pH-related issues, and malabsorption issues such as IBS), with patients gaining significant symptom improvements.
- Tirosint-SOL minimizes negative absorption effects relating to a person taking medications such as PPIs for GERD/acid reflux, even with their thyroid medication.
- It may be better absorbed, even when taken with a morning cup of coffee. Studies have shown that Tirosint is better absorbed with coffee compared to other forms of T4. In fact, new research has found that gel caps and liquid forms are unaffected when taken with coffee (unlike tablet formulations). For some people, it may be better absorbed than other forms of levothyroxine when taken with breakfast.
Potential Cons: Just like with all T4 medications, the effectiveness of Tirosint-SOL may be impacted if a given individual is experiencing poor T4/T3 conversion. Here are some additional considerations:
- As a newer and branded drug, it carries a higher cost, which means some insurance companies may penalize patients with a higher copay, while others may not pay for it at all (although the manufacturer offers a variety of programs to help with that — read more about that here).
- Conventional doctors may not be familiar with or have limited experience prescribing Tirosint, and may be reluctant to do so.
T3 Medications
Having an impaired gut, stress, and/or any of other reasons shown in the earlier T4 to T3 conversion graphic, can make a T4-only medication ineffective. We can see signs of poor conversion happening when we look at a full thyroid lab panel, as mentioned earlier.
The reverse T3 (rT3) test measures how much of the active free T3 is able to bind at thyroid receptors. RT3 is produced in stressful situations and binds to thyroid receptors, but turns them off instead of activating them. (Stress is a common cause of low T4 to T3 conversion. Under stressful situations, T4 gets converted to reverse T3 instead of T3. Reverse T3 is an inactive molecule related to T3, but without any physiological activity.)
The rT3 test is sometimes used to identify cases of poor T4 to T3 conversion, as well as thyroid symptoms that are due to adrenal stress, instead of thyroid malfunction or autoimmunity. In cases where a lot of reverse T3 is produced, adding a thyroid medication that contains T3, ensures that the right hormone is getting to the right receptors.
In my practice, we have clients routinely plot their lab results on thyroid gradients, which provide great visuals to assess conversion and general thyroid health. We can easily see when it might be time to add in a T3 medication, or switch out a T4-only medication to some kind of combination therapy.
T3-only medications are typically used as an add-on to T4-only medications, to address this issue. T3 medications have a short half-life and can pack a punch, so they must be dosed by a practitioner who is familiar with them. I’ll talk briefly about the generic, liothyronine, as well as the more commonly prescribed branded option in the U.S., Cytomel.
Liothyronine
Description: Liothyronine is the generic of the synthetic version of the thyroid hormone triiodothyronine, referred to as T3. The branded version of T3 available in the U.S. is Cytomel.
Dose: Liothyronine and T3-only medications are usually started at 25 mcg by mouth daily, increasing by 12.5-25 mcg/day over the course of 1-2 weeks. Doctors may choose to increase this by a lower dose of 5 mcg every 1-2 weeks, for elderly individuals.
Most negative side effects have to do with incorrect dosage. T3 is absorbed very rapidly (it’s considered a “fast release” medication versus “sustained” or “slow” release). This may cause hyperthyroidism and even cardio symptoms such as palpitations in some patients. A good practitioner should work with you and adjust the starting dose to best fit your particular health profile (underlying health issues, age, etc.).
Pros: As a generic prescription, liothyronine is a low cost alternative.
Potential Cons: There are five potential areas of concern; the first one is applicable to the generic only, the other four for the branded version Cytomel as well.
- Potency and ingredient inconsistency due to it being a generic
- Adverse reactions and medication ineffectiveness due to fillers
- Strict adherence required for consistent absorption and effectiveness
- Lack of practitioner familiarity and expertise
- “Fast release” and rapid absorption can cause significant effects in some people
1. Adverse Reactions and Medication Ineffectiveness Due to Fillers
While Mylan’s branded generic offering is gluten-free and lactose-free, it does contain corn starch. Other makers of the generic, such as Paddock, are not certified gluten-free, although they don’t contain gluten in their ingredients list.
2. Lack of Practitioner Familiarity and Expertise
Probably the biggest potential con is that most conventional doctors may not be familiar or experienced with adding a T3 medication to a T4-only prescription (or switching to a T3-only medication). This inexperience may lead to a prescription resulting in incorrect dose ratios, or in patients not being effectively monitored for dose-related complications.
Some practitioners may even have an extreme aversion to prescribing T3 or combination therapies, given their knowledge of the inappropriate abuse of T3 medications in the 80s. Back then it was often – and inappropriately (and dangerously!) – prescribed as a weight loss medication (sometimes along with amphetamines!) by weight loss clinics. People were admitted to emergency rooms with serious cardio symptoms, some even in a coma. Some practitioners may have witnessed this, or had at least heard of it, so they’ve perhaps shied away from learning more. You can read more about this as well as other reasons practitioners may find it challenging to prescribe anything beyond T4 medications.
Having said that, it has now been shown in the (previously mentioned) research that a subset of hypothyroid patients just don’t do well on T4 medication alone, and that some people do better with T3/T4 combination therapy. Both the American Thyroid Association (ATA) and the European Thyroid Association (ETA) guidelines on thyroid hormone therapy do suggest that in certain such cases, a trial of T3 therapy including T4 can be considered.
In the 2014 ATA guidelines, it was pointed out that previously in a 2013 survey of specialist members of The American Thyroid Association, The Endocrine Society, and The American Association of Clinical Endocrinologists, only 3.6 percent of the 880 respondents would trial adding T3 to T4 given a hypothyroid patient with continuing symptoms, despite a TSH within the target range.
Fortunately, I think we’ve made some progress since 2013, and many more practitioners are opening up to the idea of using T3 medications.
In a more recent survey of clinicians, at least 58 percent said they would prescribe a trial of combination therapy for cases where T4-treated patients with normal serum TSH exhibited residual symptoms. Another found that up to 47 percent would add T3 therapy while reducing the T4 dose.
You may, however, need to find a doctor who is more familiar and willing. Here’s a link to a database of practitioners who would be more familiar with T3 and combination therapies.
3. “Fast Release” and Rapid Absorption Can Cause Significant Effects in Some People
When T3 is given in conventional tablet form, it’s absorbed and metabolized very rapidly, causing spikes in serum blood levels that may result in heart palpitations, sweating, tightness in the chest, and anxiety in some people. There is typically a peak of serum T3 about three hours after dosing, which is followed by a relatively fast decline. This is in contrast with the relative stability of T3 levels in individuals with healthy hormone levels. For this reason, manufacturers are looking at new delivery strategies such as liquid formulations and slow release tablets.
Researchers have been using laboratory rats to test a synthetic compound made up of zinc bound to three different T3 molecules, which is delivered in a capsule that is coated to prevent its breakdown in the stomach. The capsule is able to make its way to the small intestine where the zinc facilitates a slow release of the hormone.
Cytomel
Description: Cytomel is the branded version of the synthetic thyroid hormone T3, available in the U.S. In my survey, 52 percent of respondents said they felt better after taking Cytomel. The results relating to Cytomel also showed improvement in labs for 54 percent of respondents, improvements in energy for 73 percent, improvements in mood for 55 percent, and improvements in hair loss for 26 percent.
Pros:
- Unlike the generic, branded drugs like Cytomel do not vary in potency or fillers, as they come from a single manufacturer.
- Cytomel does not contain gluten (however, it is not certified gluten-free).
Potential Cons:
- Cytomel contains corn starch and lactose.
- Fast release and rapid absorption can cause significant effects in some people.
How to Overcome:
With T3 medications, I recommend starting with a low dose and slowly increasing it. Some individuals may also consider sustained release, compounded versions of T3.
Natural Desiccated Thyroid (T4/T3 Combination Therapy)
T4/T3 medications mimic the natural biological ratio of our hormones, with a ratio of 80 percent T4 to 20 percent of the more active T3 (4:1). In many cases, I recommend natural desiccated thyroid (NDT) medications (also referred to as desiccated thyroid extract or DTE). Natural desiccated thyroid medications are isolated from the thyroid glands of pigs and are bioidentical to what we would normally produce in our own bodies. Armour Thyroid, Nature-Throid, and WP Thyroid are three examples of natural desiccated thyroid medications.
Many patients who do not feel well on conventional T4 treatments, have reported feeling much better after switching to a T4/T3 option such as NDT.
If you are someone who is not able to tolerate NDT, or if you have an ethical or religious reason (since it is animal derived) why you’re not able to take the hormone, there are also compounded versions of T4 and T3 (I’ll talk about those in a moment; these are customized synthetic, not animal derived, medications that are tailored for a given individual).
Conventional doctors may not be supportive of NDT prescriptions due to their knowledge of past issues with quality control (relating to how dosage was determined, causing inconsistencies in hormone dose). Those issues are historical and dosing is now very consistent. You can read more about the history of NDT medications here.
However, there have been recent recalls on NP Thyroid, Nature-Throid and WP-Thyroid, due to certain lots being found to be sub-potent. This means that the affected medications may have too little thyroid hormone in them. Therefore, it is important to check with manufacturers to stay informed of any recalls or potency issues. (Please contact their manufacturers and your local pharmacist directly if you have any questions or concerns.)
There are proponents of NDT medications that feel that this bioidentical version is the best option for most people (and that the trace amounts of other hormones found in this natural hormone therapy, such as T1 and T2, may in fact have undiscovered biological benefits).
There are also those that feel that for some patients, NDT medications may actually be perpetuating the autoimmune attack due to the fact that they contain thyroglobulin and TPO antibodies (since they are formulated from animal thyroids).
The bottom line is that different people will do best on different medications. A practitioner must monitor a medication’s effectiveness, checking labs and symptoms. If someone starts feeling worse on NDT medications or has an increase in thyroid antibodies, I’d then recommend they switch to a compounded T4/T3 medication (using synthetic hormones).
So let’s talk a bit about three of the NDT medications.
Armour Thyroid
Description: Armour Thyroid is a natural (bioidentical) version of combined T4 and T3 hormones. In my survey, 59 percent of respondents said they felt better using Armour Thyroid, and 73 percent had more energy.
Dose: General guidelines start at 30 mg and increase the dosage by 15 mg every 6 weeks. Your practitioner should work with you and adjust the starting dose to best fit your particular health profile (underlying health issues, age, etc.).
Most negative side effects have to do with incorrect dosage. T3 is absorbed very rapidly (it’s considered a “fast release” medication versus “sustained” or “slow” release). This may cause hyperthyroidism, and even cardio symptoms such as palpitations, in some patients. I have found that “fast release,” however, is better for people with Hashimoto’s given that they typically have gut issues that affect absorption.
Pros:
- No potency or filler variation
- Gluten-free but not certified
- “Fast release” and rapid absorption of T3
Potential Cons:
- Higher cost in most cases
- Adverse reactions and medication ineffectiveness due to fillers (contains several inactive ingredients including dextrose, calcium stearate, sodium starch glycolate, microcrystalline cellulose, and opadry white)
- Animal derived (if that is a problem for you)
- Strict adherence required for consistent absorption and effectiveness
- Practitioner may be unfamiliar with working with Armour
Nature-Throid
Description: Nature-Throid is a natural (bioidentical) version of combined T4 and T3 hormones. In my survey, 56 percent of respondents said they felt better using Nature-Throid.
Dose: General guidelines start at 30 mg and increase the dosage by 15 mg every 6 weeks. Your practitioner should work with you and adjust the starting dose to best fit your particular health profile (underlying health issues, age, etc.).
Most negative side effects have to do with incorrect dosage. T3 is absorbed very rapidly (it’s considered a “fast release” medication versus “sustained” or “slow” release). This may cause hyperthyroidism, and even cardio symptoms such as palpitations, in some patients.
Pros:
- No potency or filler variation
- Hypoallergenic
- “Fast release” and rapid absorption of T3
Potential Cons:
- Higher cost in most cases
- Animal derived (if that is a problem for you)
- Strict adherence required for consistent absorption and effectiveness
- Lack of practitioner familiarity and expertise
- Currently under recall — see my note below on switching meds!
WP Thyroid
Description: WP Thyroid is a natural (bioidentical) version of combined T4 and T3 hormones. In my survey, 32 percent of respondents said they felt better using WP Thyroid.
Dose: General guidelines start at 30 mg and increase the dosage by 15 mg every 6 weeks. Your practitioner should work with you and adjust the starting dose to best fit your particular health profile (underlying health issues, age, etc.).
Most negative side effects have to do with incorrect dosage. T3 is absorbed very rapidly (it’s considered a “fast release” medication versus “sustained” or “slow” release). This may cause hyperthyroidism, and even cardio symptoms such as palpitations, in some patients.
Pros:
- No potency or filler variation
- Hypoallergenic
- “Fast release” and rapid absorption of T3
Potential Cons:
- Higher cost in most cases
- Animal derived (if that is a problem for you)
- Strict adherence required for consistent absorption and effectiveness
- Lack of practitioner familiarity and expertise
- Currently under recall — see my note below on switching meds!
Compounded T4/T3
If NDT medications do not seem like a good fit for you, compounded T4/T3 products offer another alternative. These medications also offer the advantage of being made devoid of any fillers that people may not tolerate, such as lactose or gluten, which are present in some thyroid medications and can be problematic for thyroid patients. Furthermore, these medications do not increase autoimmunity.
However, compounded T4/T3 products need to be prepared by specially trained compounding pharmacists. These compounds are usually much more expensive and may need to be refrigerated to preserve activity.
Thyroid compounds are usually prepared in the same physiological ratio that is found in NDT products. However, physicians can elect to change the amount of T3 and T4, as compounding pharmacists must make the medications from scratch. This can be a huge advantage for patients who did not feel well on conventional treatments or natural desiccated thyroid treatments.
Most T4/T3 compounds, like NDT products, are immediate release versions, which means they’re formulated to release the active medication immediately after oral administration. However, compounding pharmacists can also make sustained release versions.
While there has been some concern expressed about the potential side effects of fast release thyroid medications (such as Cytomel), I have found that slow-release products don’t tend to work as well for my clients with Hashimoto’s.
Slow-release products may be more difficult to absorb, as many people with Hashimoto’s have gut issues (leaky gut). Methocel is the name of the slow-release formulation that compounding pharmacists will use.
For my clients, I usually recommend a fast release/immediate release T4/T3 formulation, which utilizes Avicel as the filler. I’ve seen quite a few times where people have gotten suspended release or slow release compounded thyroid hormones… and all of a sudden, their TSH went from 1 to 3 μIU/mL, to 8 or 10 μIU/mL, or even to 15-20 μIU/mL! As such, when people say, “I tried compounded medications and they didn’t work for me!”, the very first question I ask is: “Okay. Was it a slow-release form?”
In other words, we do not want slow-release if we have Hashimoto’s and any kind of gut issue.
Pros:
- Medications can be customized for your ideal ratio of T4/T3 and with filler ingredients that you are not sensitive to
- Can be made as fast or slow release versions
Cons:
- Not all doctors are familiar with prescribing T3/T4 meds
- A compounding pharmacist may not be available in your area
- You may need to pay out of pocket for them
Considerations:
Compounding pharmacies need to be high quality and meticulous due to the tiny amounts of drugs they work with; any errors can be magnified. I maintain a list of recommended compounding pharmacies for that reason. I look for compounding pharmacies that offer PCCA dilutions. PCCA is an association for pharmacists that helps them create more effective and more standardized compounds.
I recommend asking the following questions when considering a compounding pharmacist:
- What types of fillers are used?
- What is the source of the materials?
- Is the compound slow-release or immediate release?
Now that we’ve gone over the available thyroid hormone medications out there, let’s review the side effects and general precautions for thyroid hormone medications.
Switching Medications
While dose conversions from different medications are readily available, there may still be some discrepancies in the dose you receive and how you absorb the medications, so carefully monitor your symptoms and repeat your labs four to six weeks after switching, to make sure your body is adjusting properly.
While the conversion chart below is a great place to start, please note that NDT may be more bioactive, and thus physicians may elect to initiate with slightly lower doses when switching from levothyroxine to NDT. Furthermore, Tirosint may be better absorbed compared to other forms of levothyroxine. Thus, physicians may elect to initiate with slightly lower doses when switching from levothyroxine to Tirosint.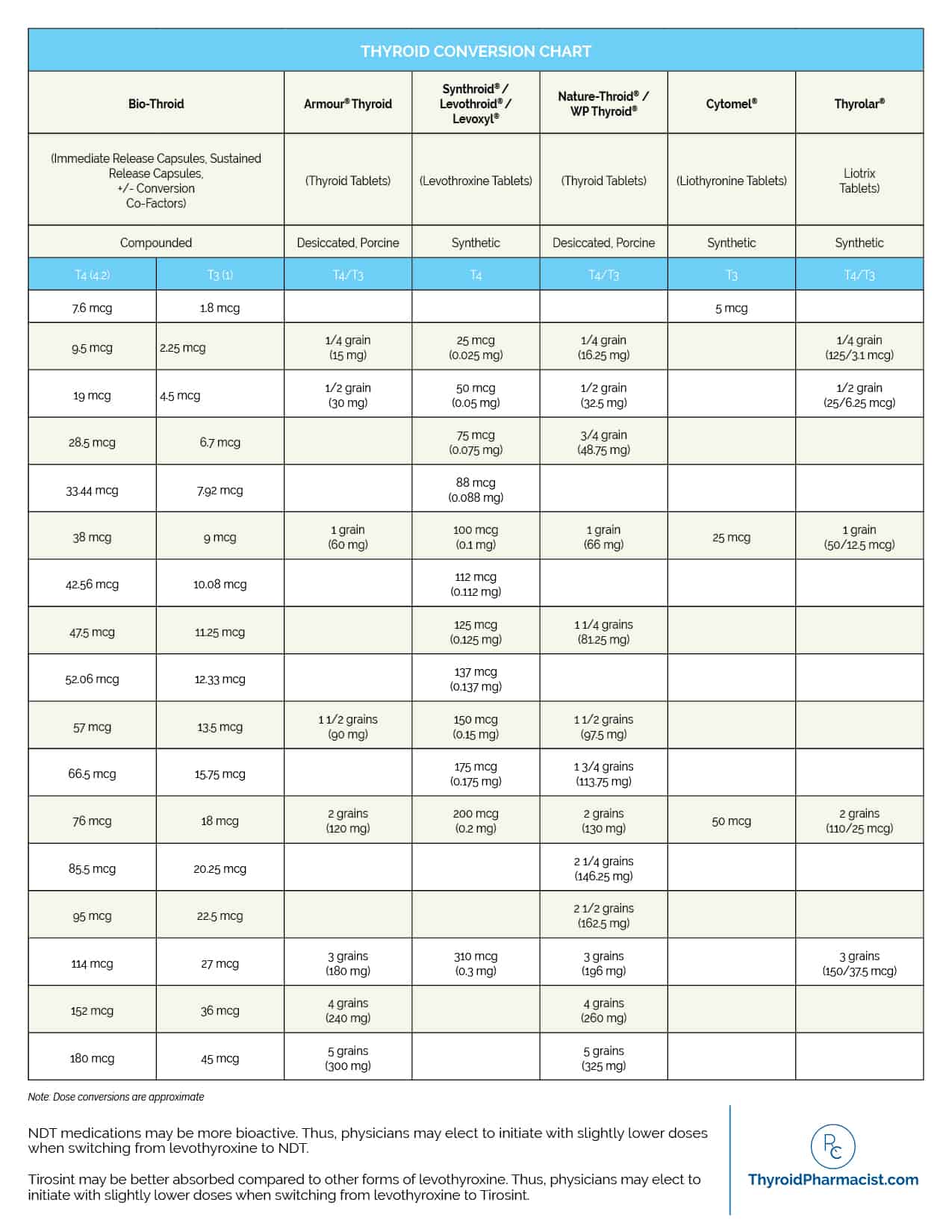
If you want more information on adjusting or switching your thyroid medication, I have written a short eBook called Optimizing Thyroid Medications, that you can download for free for a limited time. This eBook talks more about the types of thyroid medications and medication protocols out there, as well as medication titration, the issue with fillers, case studies to help show the benefits of different medications, and much more.
In light of the recalls of several NDT thyroid medications over the past few years (NP Thyroid, Nature-Throid and WP-Thyroid), I’ve had a lot of questions about what replacement options people have. So, I wanted to take a moment to list some different options for when these medications aren’t available.
My top choices for replacement medications are:
- Armour: It is the most similar to other NDT options, but some people have issues with corn as a filler ingredient, and some have reported this medication actually raising their TPO antibody level. The theory is that it may contain some thyroglobulin due to the manufacturing process, but I am not 100 percent sure if this is the case. That said, many people do well with this medication, and I have previously taken it myself with great results.
- Compounded T4/T3: These are medications tailor made by compounding pharmacists. Ask for the immediate release version, as sustained release versions may not be absorbed properly by people with Hashimoto’s and gut issues like intestinal permeability (leaky gut).
- Tirosint and Tirosint SOL: These are T4-only options in highly absorbable formulations that can withstand food and coffee. Of all of the T4 medication options, these have the best absorbability and the fewest fillers. For those who have issues with converting T4 to T3, another version of T3 can be added, such as Cytomel, liothyronine or compounded T3.
- Synthroid or Levoxyl: These can also be combined with Cytomel or liothyronine for a T4/T3 combo medication.
- Generic levothyroxine: This can also be combined with Cytomel or liothyronine for a T4/T3 combo medication.
The Takeaway
I hope this article gave you a good overview of the various types of thyroid medications that are available to you. Just like there is no diet that is perfect for everyone, there is no “one size fits all” when it comes to thyroid hormones. In many cases, it will take some trial and error to find the right medication and dosage that reduce your symptoms and help you feel your best. I do recommend working with a practitioner who is open to exploring the different options out there, so that you are not limited in your choices and can find the right fit for your situation.
Beyond thyroid hormone replacement therapy, there are also lifestyle changes I recommend to ensure that you feel your best and are not just addressing the hormone imbalances that result from Hashimoto’s, but the underlying root causes.
Did you find this article helpful? Let me know your experience with thyroid medications in the comments, or join me over on Facebook or Instagram!
You can also download a free Thyroid Diet Guide, 10 Thyroid friendly recipes, and the Nutrient Depletions and Digestion chapter by signing up for my weekly newsletter. You will also receive occasional updates about new research, resources, giveaways and helpful information.
Don’t forget to download my free eBook on optimizing your thyroid medications as well!
References
- Fuentes AV, Pineda MD, Venkata KCN. Comprehension of Top 200 Prescribed Drugs in the US as a Resource for Pharmacy Teaching, Training and Practice. Pharmacy (Basel). 2018;6(2):43.
- Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We’ve Been and Where We’re Going. Adv Ther. 2019;36(Suppl 2):47‐58.
- Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We’ve Been and Where We’re Going. Adv Ther. 2019;36(Suppl 2):47‐58.
- Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We’ve Been and Where We’re Going. Adv Ther. 2019;36(Suppl 2):47‐58.
- Taylor PN, Eligar V, Muller I, Scholz A, Dayan C, Okosieme O. Combination Thyroid Hormone Replacement; Knowns and Unknowns. Front Endocrinol (Lausanne). 2019;10:706.
- Dayan C, Panicker V. Management of hypothyroidism with combination thyroxine (T4) and triiodothyronine (T3) hormone replacement in clinical practice: a review of suggested guidance. Thyroid Res. 2018;11:1.
- Fallahi P, Ferrari SM, Ruffilli I, et al. Advancements in the treatment of hypothyroidism with L-T4 liquid formulation or soft gel capsule: an update. Expert Opin Drug Deliv. 2017 May;14(5):647-655.
- Vita R, Saraceno G, Trimarchi F, et al. A novel formulation of l-thyroxine (l-T4) reduces the problem of l-T4 malabsorption by coffee observed with traditional tablet formulations. Endocrine. 2013;43(1):154–160.
- Cappelli C, Pirola I, Gandossi E, et al. Oral liquid levothyroxine treatment at breakfast: a mistake? Eur J Endocrinol. 2013 Nov 22;170(1):95-9.
- Vita R, Saraceno G, Trimarchi F, et al. A novel formulation of l-thyroxine (l-T4) reduces the problem of l-T4 malabsorption by coffee observed with traditional tablet formulations. Endocrine. 2013;43:154–160.
- Cappelli C, Pirola I, Daffini L, et al. A double-blind placebo-controlled trial of liquid thyroxine ingested at breakfast: results of the TICO study. Thyroid. 2016;26:197–202. 10.1089/thy.2015.0422.
- Pirola I, Gandossi E, Brancato D, et al. TSH evaluation in hypothyroid patients assuming liquid levothyroxine at breakfast or 30 min before breakfast. J Endocrinol Invest. 2018;41:1301–6. 10.1007/s40618-018-0867-3.
- Benvenga S, Ducharme MP. Comparison of the intestinal absorption of levothyroxine (LT4): Tablet vs. soft gel capsule formulation. Endocr. Rev. 2011;32:3–625.
- Vita R, Saraceno G, Trimarchi F,, et al. A novel formulation of l-thyroxine (l-T4) reduces the problem of l-T4 malabsorption by coffee observed with traditional tablet formulations. Endocrine. 2013;43:154–160.
- Saraceno G, Vita R, Trimarchi F, et al. Two novel formulations of l-T4 (oral solution and soft gel capsule) are refractory to the coffee-induced intestinal malabsorption of tablet l-T4. Eur. Thyroid J. 2013;2:P132–P145.
- Virili C, Giovanella L, Fallahi P, et al. Levothyroxine therapy: changes of TSH Levels by switching patients from tablet to liquid formulation. A systematic Review and meta-analysis. Front Endocrinol (Lausanne). 2018;9:10.
- Jonklaas J, Bianco AC, Bauer AJ, et al. Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid. 2014;24(12):1670‐1751.
- Dayan C, Panicker V. Management of hypothyroidism with combination thyroxine (T4) and triiodothyronine (T3) hormone replacement in clinical practice: a review of suggested guidance. Thyroid Res. 2018;11:1.
- Burch HB, Burman KD, Cooper DS, et al. A 2013 survey of clinical practice patterns in the management of primary hypothyroidism. The Journal of Clinical Endocrinology & Metabolism. 2014;99(6):P2077–2085.
- Jonklaas J, Tefera E, Shara N. Short-Term time trends in prescribing therapy for hypothyroidism: results of a survey of American Thyroid Association Members. Front Endocrinol (Lausanne). 2019;10:31.
- McAninch EA, Bianco AC. The swinging pendulum in Treatment for hypothyroidism: from (and toward?) combination therapy. Front Endocrinol (Lausanne). 2019;10:446.
- Idrees T, Price JD, Piccariello T, et al. Sustained release T3 therapy: animal models and translational Applications. Front Endocrinol (Lausanne). 2019;10:544.
- Rush University Medical Center. Potential therapy for treatment-resistant hypothyroidism proves effective in lab study: Novel coordination of thyroid hormone with zinc promotes slow release of active hormone to supplement standard therapy. ScienceDaily. www.sciencedaily.com/releases/2018/10/181012135315.htm. Accessed May 29, 2020.
- BiancoLab. http://deiodinase.org/2013/05/06/nutrient-availability-and-thyroid-hormone-activation-2/. Accessed October 12, 2020.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Thank you for this article! Very helpful… I’m wondering if it’s OK to drink coffee wait an hour and then take medication?… That’s what I’ve been doing. But not sure if that’s effective
Sam – thank you so much, I’m so glad you found it helpful! Thyroid medication should be taken on an empty stomach, one to two hours before eating, taking other medications, supplements or coffee to ensure appropriate absorption. Here is an article you might find helpful:
CONTROVERSY COFFEE AND YOUR THYROID
https://thyroidpharmacist.com/articles/controversy-coffee-bad-thyroid-myths-truths/
Tried to find what meds were recalled but could not find a source. Also I do not have any symptoms to say I need this thyroid med except a blood test with TSH off the wall.
Marcia – thank you for following! <3 Unfortunately, I do not have more information than what is available to the public on the recent recalls. Please see this link for additional information: https://getrealthyroid.com/
If you have subclinical hypothyroidism, it’s a gray area for treatment. For me, this is the way I think about it: if you don’t have any symptoms and you are trying to reverse Hashimoto’s the natural way, you can give yourself three months or so to get into remission. But, if you continue to worsen, and if it doesn’t get better, then I would start considering medications. Medications can help reduce many patients’ symptoms. They may also help reduce thyroid antibodies. In people who have really high antibodies or who have a lot of symptoms and antibodies, it may be a good idea to get on medications right away. There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication you are looking for, you may consider asking your local pharmacist for doctors in your area who prescribe the medication you are looking to try. I’m a big fan of using everything we can to get ourselves better, and medications are not always life-long. Some people are able to get off of them if they figure out their triggers and root causes. Here are a couple articles you might find interesting:
PATIENTS WITH SUBCLINICAL HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/patients-subclinical-hypothyroidism-deserve-care-treatment/
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Great article – but now what do you do if you can’t find it? I’ve tried all my local pharmacies started calling other provinces and nobody can get a hold of this. The only thing I’ve seen is some hoarder companies that are selling them for literally $6 a dose! And who knows if that’s legit or not.
If you have any information on where I can purchase tarot send Sol in Canada as of July 8th 2025 I would love to hear it!
Thank you and big hello from west coast of Canada
T – thank you for reaching out, I’m sorry to hear about the difficulty you’re experiencing in finding the product you’re seeking. Unfortunately, I don’t have information on where to purchase in Canada. It’s important to exercise caution when considering purchasing from unfamiliar sources, especially if prices seem unusually high, as this could indicate potential issues with product authenticity or quality. If you’re looking for specific health products or supplements, I recommend consulting with a healthcare professional who can provide guidance tailored to your individual needs and help you find reputable sources. They may also be able to suggest alternative products that are more readily available and suitable for your health requirements.
Hello Dr. Wentz,
I have been reading your advice for 7 years now. It was recommended to me when I first got diagnosed and it was very helpful to have someone so knowledgeable explain things in such detail.
When I learned my Nature Throid was recalled I was eager to see what you had to say and what recommendation you had for new medication. That being said, my pharmacist told me the recall was due to increased potency “up to 15% higher”. This was consistent with my symptoms as well.
I understand each batch could have their own issues but wanted to flag this and see if you had any additional information. Since then I have been trying to get into a new endocrinologist and have been reducing my dosage with the remaining medication (which was the recommendation until I could be seen).
My previous endocrinologist was not very supportive when my labs were “normal” but my symptoms remained, and recommended additional medications rather than working to tweak my current dosage.
One change that I found to make a measurable impact was taking my thyroid medication before bed, possibly because the slower acting made it more available when I needed it during the day. Again any information you have on this is always appreciated.
Many thanks!
Stephanie
Stephanie, thank you for reaching out and sharing your journey with me. ❤️ I understand how hard it is to find the right practitioner! I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
Thanks for this article. It is just what I needed, as I am always trying to get past the chemist staff; ie not the pharmacist, in that don’t muck around with my script, as well when I go to hospital about the regime for taking my medication.
Margaret, – you are very welcome! <3 I hope it's helpful and please keep me posted on your progress. <3
Thanks for the article. I switched from Naturethroid due to its potency/reliability issues to a lesser dose of Tirosint SOL (one step down). My TSH went from almost 7 to .1 in less than 6 weeks. My doctor then lowered my dosage from 150mcg to 125mcg and I’m still experiencing what seems to be hyperthyroid symptoms (sweating, hot/cold, blurry vision off and on, insomnia). I’m almost certain I need to lower the dosage again and will consult with my doctor. Have you heard of similar experiences with Tirosint SOL? It seems very strong compared to other thyroid medications.
Anne – thank you for reaching out. I’m so sorry you are struggling with all of this. <3 You may want to consider having your medication compounded. There are ompounding pharmacies that can provide more of a customized dose. Here is an article you might find helpful:
IS YOUR T4 MEDICATION WORKING
https://thyroidpharmacist.com/articles/is-your-t4-medication-working/
Hello Dr Wentz – I am wondering if you have any information regarding the potency of Tirosint SOL. I was switched to it after having been under dosed while on Naturethroid. Following the FDA’s recall, I was started on 150mcg of Tirosint SOL, which was one step lower than the Naturethroid equivalent. Within four weeks, my TSH went from 7 down to .1. I began experiencing hyperthyroid symptoms. I have since been stepped down twice and will now try 100mcg. Tirosint SOL seems to be far better absorbed and more potent than other thyroid medications. Have you come across this in any of your research?
Anne, thank you so much for sharing. <3 Here is an article you might find helpful: https://thyroidpharmacist.com/articles/is-your-t4-medication-working/
I have been diagnosed with Hashimoto disease. I also have Lupus, which has been in remission. Mostly, but was told this what had caused thyroid to malfunction.. my tsh was 16 several months ago, t3 t4 ok. I am currently taking iodine supplements and tsh is down to 9 was told it would take several months to correct. Do not want to take medication. Want to know what your feelings are on this treatment
Joan – thank you for reaching out. <3 I'm sorry you are struggling with all of this. Most autoimmune conditions, such as Lupus and Hashimoto's have common root causes, and a lot of times the things that are recommended for one will help with other. Hashimoto’s is an autoimmune condition that results in the immune system damaging the thyroid, which leads to a lack of thyroid hormone production. Most cases of hypothyroidism in the United States and other countries that add iodine to their salt supply are caused by Hashimoto’s. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target. We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my books focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are some articles you might find helpful:
IMPORTANCE OF GUT HEALTH
https://thyroidpharmacist.com/articles/importance-gut-health/
IODINE AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/iodine-hashimotos/
FOOD SENSITIVITIES AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/food-sensitivities-and-hashimotos
Hi! I have been struggling trying to find the right medicine and am sort of scared to keep doing so. I started on nature thyroid in June and the first month was great but I got the recalled version and felt horrible until I realized what happened I tried armour which I gained allt of weight on and now my doctor prescribed me compounded t3/t4 I just am anxious to try it because I have gained a weird amount of weight in a short period of time from one of the NDT. Is that something that can happen? My doctor has been not helpful in the slightest in regards to bad symptoms and told me to just stop taking medicine but I feel bad when I stop taking anything. Is it common to gain weight on the compounded medicine?
Katherine – thank you so much for sharing. <3 Thyroid hormone medications are very individualized! What works for one person not be your best option, leaving you with lingering symptoms such as fatigue, anxiety, brain fog, and excess weight. And just because your doctor may be most familiar and comfortable with prescribing one particular type of thyroid hormone medication, doesn’t mean you should settle for their preferred medication if that particular prescription just isn’t working for you. There are quite a few options for thyroid medications.Have you read these articles? ❤️
HISTORY OF NATURAL DESICCATED THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/the-history-of-natural-desiccated-thyroid-medications/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
Hello Dr. Wentz,
Please help me understand considerations when changing from a compounded T3 to Cytomel given compounded T3 is longer acting and Cytomel fast acting.
I take Tirosint 63mcg/day-no problem, with Compounded T3 20mcg/day (10mcg AM, 10mcg PM)
The Compounded T3 was changed to Cytomel 20mcg total/day (10mcg/AM, 10mcg/PM).
WOW! I felt the effect of what you wrote about: jitters, some anxiety, hand tremor.
The Cytomel was then decreased to 10mcg total/day and now 5mcg total/day which I am evaluating now.
Is Cytomel really that potent compared to Compounded T3 to the point a decrease from 20mcg/day to 5-10mcg/day is typical?
Thank you,
Rachel
Rachel – thank you so much for reaching out and sharing. <3 Everyone will react differently! In my experience, what works for one person may not work for another. I recommend discussing your experience and symptoms with your practitioner so they can evaluate and make changes to your dosage as needed. Here is an article with more information on Tirosint that I hope you find helpful as well:
IS YOUR T4 MEDICATION WORKING FOR YOU? (Tirosint)
https://thyroidpharmacist.com/articles/is-your-t4-medication-working/
Hello! Thank you for all your detailed info! My question is I switched bc of the recall from 81.25 on Nature throid which I was feeling great on to 90 mgs of Armour. 6 weeks in I felt totally hyper. Major weight loss, heart racing, random low fevers, exercise intolerance, feeling awful. Instead of going back to old recalled Med, I cut the nature throid in half for 4 weeks and seems to have had a crash. Like a major drug withdrawal. So I worked my way back up to 81.25, still feel off and crummy and heart palps remain , labs look good though. What do you recommend moving forward? Do you think it was just that that the Armour dosing was too high? Think it would be safe to try Armour at 60 mgs? This is so hard. It’s wreaked havoc on my health and life.
Thanks in advance
Karen – thank you so much for sharing. <3 I'm so sorry you are struggling with this. I understand how frustrating and hard it is. It is never advisable to alter your medication dosages, without the advice of your practitioner. T4 thyroid hormone medications have a half-life of about 1 week. This means that when a person stops taking them, the amount of the hormone activity in their body, from the medication, will decrease by about 1/2 each week. For T3 medications, this half-life is only about 1 day. Generally, within three weeks (or a few days for T3), most of the hormone will be out of the body. This could result in increased symptoms, an increase in the autoimmune attack on the thyroid, and extra stress on your body and the thyroid. There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication which you are looking for, ask your local pharmacist for doctors in your area who prescribe the medicationyou are looking to try. Have you read these articles? ❤️
MEDICATIONS FOR HASHIMOTO'S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
IS YOUR T4 MEDICATION WORKING FOR YOU? (Tirosint)
https://thyroidpharmacist.com/articles/is-your-t4-medication-working/
Hi Dr. Wentz,
I was on Naturethroid with no issues for 6 years before it was reformulated and I have been trying to find something that works and it’s been challenging. NP Thyroid worked great until their reformulation. Synthetic t4/t3 gave me leg cramps (maybe restless leg syndrome), Armour gave me reflux and slightly labored breathing. Tirosint and Synthroid did the leg cramp thing too. I think those medications would be great if I could figure out the leg cramp thing. Could that be an over/undermedication thing? My doctor is stumped by that and I am out of options. Any suggestions? Labs look ok on all but not optimal.
Lynn – thank you for reaching out and sharing your journey. <3 In my experience, what works for one person may not work for another. You may want to try a compounding pharmacist to see if titrating your dosage would help. Also, from my experinece, joint pain, leg cramps, menstrual cramps, and thyroid disorders are always a reason to suspect magnesium deficiency. Here is an article you might find intersting:
NEW STUDIES ON MAGNESIUM AND THYROID HEALTH
https://thyroidpharmacist.com/articles/new-studies-on-magnesium-and-thyroid-health/
Thank you for an excellent article! I’ll share it with my doctor.
Have a good day!
Paula – you are very welcome! I hope you will keep me posted on your progress! <3
What can you use for reflux other than the script medication by doctors that won’t effect ones hashimoto. Thanks
Lyn – thank you for reaching out. ❤️ Acid Reflux is a very common symptom that occurs in people with Hashimoto’s. Studies have shown that most people with Hashimoto’s either have very low stomach acid or produce no stomach acid at all. The person who does not have enough stomach acid will have the same symptoms as a person with an overabundance of stomach acid. Here are some articles I hope you find helpful:
GOT ACID REFLUX?
https://thyroidpharmacist.com/articles/got-acid-reflux
HASHIMOTOS AND LOW STOMACH ACID
https://thyroidpharmacist.com/articles/hashimotos-and-low-stomach-acid
GOING DAIRY FREE TO REVERSE HASHIMOTOS
https://thyroidpharmacist.com/articles/going-dairy-free-to-reverse-hashimotos
I thought this article was helpful. I’m a 73 yr old male diagnosed with and treated for hypothyroidism for over 25 years. Originally I was treated with Synthroid, then switched to levothyroxine at 125 mcg. I found a nurse practitioner in my area who specializes in thyroid treatment and after extensive testing placed me on NP Thyroid 75mg (60+15). This is my current treatment, and my Walmart pharmacy is still able to provide this brand of medicine. Your article makes reference to this medicine but omits it from your current recommendations as if it were no longer available. Should I be inquiring on my healthcare specialist about switching to something different?
Carmen – thank you so much for sharing! ❤️ I’m so glad you have found a medication that works for you. In the article I mentioned recent recalls on lots of NP Thyroid and some other brands due to certain lots being found to be sub-potent. If you have concens about your medication it is best to discuss this with your practitioner and or pharmacist.
Thank you so much for the tremendous knowledge you share with us as well as the resources you provide. I have Hashimotos. I feel best with a combination of Synthroid plus Cytomel. I have also been taking LDN (1.5 mg) for the last 18 months. The LDN is finally helping my antibodies go down. They were so high we weren’t even able to get the number, now at least I know they are at 999 and getting lower. My question is with regard to TSH. I feel best when my TSH is very, very low. I was told by an endocrinologist in the Chicago area that Cytomel artificially surpresses TSH and so he didn’t worry too much about it as long as my other symptoms were fine. I am feeling the best ever after 20 years have hell, but my new functional medicine doctor keeps wanting to change my sythroid. I am worried I will gain the weight that has taken me 18 months to lose back and will again get the horrible fatigue and hairloss and body aches back. Can you point me in the direction of how Cytomel suppresses TSH?
Karen – thank you for reaching out. ❤️ Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. I recommend discussing your concerns with your practitioner. Have you read these articles?
MEDICATIONS FOR HASHIMOTO’S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
Hello Dr. Wentz,
Thank you so much for such valuable information. You are my “go to” doctor when I need help.
Question: do you know the T4 to T3 ratio in 30mg of bovine thyroid? I have severe Celiac’s/IBS and cannot tolerate anything other than synthetic liquid thyroid medication. I would like to supplement my medication with the above mentioned thyroid medication in order to get some of the T1 and T2 hormones as I felt better when taking NP Thyroid (aside from the digestive issues related to corn in the tablet).
Your thoughts?? Thank you so much!! ❤️ Constance!
Constance – you are very welcome! I’m so glad you are finding my research helpful! ❤️ I am not able to advise on the ratio or whether the bovine supplement would be appropriate for you and your specific health needs without a comprehensive health assessment. I recommend that you discuss the addition of this with your personal doctor.
Hi Dr. Wentz! I have a question regarding thyroid symptoms. Is shortness of breath as it relates to Hashimoto’s more often considered a sign of hypo or hyper thyroid? I have a very low TSH (less than 0.01), slightly low T4 and normal to slightly high T3. Other symptoms besides the shortness of breath include cold hands and feet, constipation and feeling tired. Antibodies are at 24, which is higher than usual. I’m looking for a functional medicine dr. currently to help me heal Hashi’s vs. just medicating. Thank you for dedicating your career to help those who suffer from this autoimmune disorder!
-Jia
Jia – thank you for reaching out. <3 This is something that Hashimoto’s can be known for. Some symptoms may also be due to underactive adrenals. I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It's a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
Dr Wentz I just purchased both of your books, thank you for all that you are doing for the health community! I wanted to ask whether women trying to conceive with “normal” TSH ranges (2.7), but slightly high T4 and low T3 levels should be treated with desiccated thyroid or meds?? Or is having only slightly abnormal thyroid numbers only considered “subclinical” hypothyroidism not worth treating with medication? I am confused based on your writing when exactly it is appropriate to follow diet/lifestyle changes only, and when it is appropriate to get a prescription for some sort of T4/T3 therapy?
All the best and thank you for your time and these wonderful online posts. Please write a book about pregnancy and fertility!
Katie – thank you for reaching out. If you have subclinical hypothyroidism, it’s a gray area for treatment. For me, this is the way I think about it: if you don’t have any symptoms and you are trying to reverse Hashimoto’s the natural way, you can give yourself three months or so to get into remission. But, if you continue to worsen, and if it doesn’t get better, then I would start considering medications. Medications can help reduce many patients’ symptoms. They may also help reduce thyroid antibodies. In people who have really high antibodies or who have a lot of symptoms and antibodies, it may be a good idea to get on medications right away. There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication you are looking for, you may consider asking your local pharmacist for doctors in your area who prescribe the medication you are looking to try. I’m a big fan of using everything we can to get ourselves better, and medications are not always life-long. Some people are able to get off of them if they figure out their triggers and root causes. Have you read these articles? ❤️
MEDICATIONS FOR HASHIMOTO’S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
IS YOUR T4 MEDICATION WORKING FOR YOU? (Tirosint)
https://thyroidpharmacist.com/articles/is-your-t4-medication-working/
Thanks so much for your informative web site. I’m learning quite a bit.
I have Hashimotos and was on NatureThroid for many years prior to the recent recall. I started a compounded T4 (Levothyroxine) and slow release T3 (I know no after reading your blog that fast release T3 might be a better option.
I was taking 1.5 GR on Naturethroid daily. The new compounded formula is 60 MCG T4 and 8 MCG T3. I’ve been on this for a little over 6 weeks.
I had my labs done yesterday and my TSH was off the charts at 24.69. My Free T3 and Free T 4 are in the lower range. Needless to say I feel awful. and have gained about 8 lbs. I do have a very sensitive chemical make up to fillers , binders, and dyes. I do not have any gluten in my diet. I did take Armour many years ago and did ok on it until that was recalled and hence started with the Naturethroid. I’m hesitant to keep trying to dial in the compound formula and I’m thinking of just going on Armour. This is running my life and need to get this medication dialed in and it’s so hard to find a good dr. to work with. Any input would be appreciated.
Thanks
Jill – thank you so much for sharing. I’m so sorry to hear you are struggling with all of this! I understand how hard it is. As you know, there are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication which you are looking for, ask your local pharmacist for doctors in your area who prescribe the medication you are looking to try. ❤️ I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
Hi Isabella
I have high antibodies, over 1000 and t3 and t4 in normal range but slightly elevated ths levels.
Do I need medication or can I go the natural route to heal?
Also I have huge amount of mucus in my throat and constantly throat clearing which is affecting my voice. I know this is linked to my hasimoto’s.
Any suggestions for what could help this?
Thank you so much
Carmel – thank you for following! ❤️ If you have subclinical hypothyroidism, it’s a gray area for treatment. For me, this is the way I think about it: if you don’t have any symptoms and you are trying to reverse Hashimoto’s the natural way, you can give yourself three months or so to get into remission. But, if you continue to worsen, and if it doesn’t get better, then I would start considering medications. Medications can help reduce many patients’ symptoms. They may also help reduce thyroid antibodies. In people who have really high antibodies or who have a lot of symptoms and antibodies, it may be a good idea to get on medications right away. There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication you are looking for, you may consider asking your local pharmacist for doctors in your area who prescribe the medication you are looking to try. I’m a big fan of using everything we can to get ourselves better, and medications are not always life-long. Some people are able to get off of them if they figure out their triggers and root causes. Here are a couple articles you might find helpful as well:
HASHIMOTO’S AND THYROID ANTIBODIES: PART 1
https://thyroidpharmacist.com/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://thyroidpharmacist.com/articles/part-2-mechanisms-reduce-thyroid-antibodies/
It’s very difficult to read this article with the “share” bar running down the left side of the screen. It covers the writing.
Alex – thank you so much for sharing your feedback! ❤️ I’m so sorry, it can be closed by selecting the arrows at the bottom of the share bar (they appear if you hover over it)!
Dear Dr. Wentz,
I have only just now come upon your helpful article. I was on Naturethroid for RAI treated Grave’s Disease for 5 years and did great on it. I started taking Armour after Naturethroid was recalled, but have never done well on it. Just wondering if you feel that NP Thyroid is a viable option? Thank you!
Karen – thank you for reaching out. ❤️ There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication which you are looking for, ask your local pharmacist for doctors in your area who prescribe the medication you are looking to try. Have you read these articles? ❤️
MEDICATIONS FOR HASHIMOTO’S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
Hi! Thanks a lot for this detailed information!
How can a Nutrition genome test help me? Do I receive recommendations with the results? If I have a problem with the DIO2, will they tell me which diet is better for me?
Where can I find more information on the specific diets for specific gene predisposition?
Sandrine – thank you for reaching out! ❤️ Nutrition Genome provides the test results. I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. Here are some resources I hope you find helpful:
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://thyroidpharmacist.com/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
Hi Doctor Wentz,
First of all I want to thank you for educating us regarding to hashimoto’s. It was until I bought and read your books that I knew what was going on my body. I struggle with this condition for almost three years until I asked my regular doctor to test me for Hashimoto’s. They prescribed me levo at first but I had a severe reaction to this medication that I ended up in ER. They tried Synthroid but it happened the same. Finally after a lot of battle my endocrinologist put me on Nature-Throid. I was doing pretty well ( a flare up a year but not too bad) until it was recalled. My journey started over. My doctor tried tyrosint but I had a severe reaction again. The doctor put me on a low dose of armour. I noticed I started gaining a lot of weight and I have gained 30 pounds in only four months. I do not have any other symptom like at the beginning. My battle now is with the weight. The doctor did adrenal test, heart test, liver and kidney enzymes test but everything came back to normal. I am also with perimenopause and I do not know if it is more related to this one.
I would really appreciate your help.
Thank you,
Consuelo
Consuelo – thank you for reaching out. ❤️ I’m sorry to hear you are struggling with weight. When it comes to weight gain these are a couple of things to think about.
1) What was your recent TSH, Free T3 and Free T4? Sometimes when those numbers are on the outskirts of normal, your metabolic rate may still be impaired making it more difficult for you to burn calories. Most people report feeling well with a TSH between 0.5-2.
2) What type of medication are you on? Some report more weight loss with T4/T3 combinations (Armour, Nature-Throid, compounded medications) versus T4 medications (Synthroid, Levoxyl, Tirosint) alone. T4 is a precursor to T3, but some individuals do not convert T4 to T3 properly, and the T3 component is the metabolically active one.
3) What type of diet are you eating? Some report more weight loss with T4/T3 combination vs T4 alone. Some do not convert T4 properly.The Standard American Diet (S.A.D.) full of sugar and simple carbohydrates is perfectly designed to cause us to gain weight year after year. Even yogurts that are marketed as “healthy” contain the equivalent of 16 teaspoons of sugar. Divorcing the S.A.D. is often a step that many of us must take to not just lose weight, but to also feel better. Some diets that have been helpful include the Body Ecology Diet, the Paleo Diet, the Virgin Diet, Autoimmune Paleo Diet, GAPS diet, SCD diet, Weston A. Price Diet, or the Mediterranean Diet. You may need to modify these diets to your own individuality.
BEST DIET FOR HASHIMOTO’S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/best-diet-for-hashimotos-hypothyroidism
HOW TO LOSE WEIGHT WITH HASHIMOTO’S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/how-to-lose-weight-with-hashimotos
Hi Dr.
I am 35 years old, I have hashimoto’s, I have fixed more less some gut problems, adressing blasto. My TSH is around 2.5, I exercise 5 times a week with an empty stomach, I take probiotics, I have improved a lot the reduction of hair loss, I follow an anti-inflammatory diet, taking some supplements. but for the first time I am having a hard time losing weight. I gain weight with out any reason and not sure what to do or what I am doing wrong. Should I consider starting thyroid medication?
Thank you very much.
Cecilia – thank you for reaching out. Exercise can be very healthy, but for people with Hashimoto’s it can create stress. Stress causes our adrenals to pump out extra hormones, and shifts our body from a relaxing, digesting, healing state to a fight or flight state. The body’s energy is shifted from doing “useless” things like growing beautiful hair, metabolizing, making hormones, digesting and repairing itself, and instead, all of the body’s resources are reserved to make cortisol and adrenaline that is pumped through our veins so that we can keep going. Eventually, we run out of nutrients that are required for proper adrenal function and we get to a state of adrenal fatigue. This is when our body is no longer able to heal itself. As for medications, if your thyroid hormone levels are not optimal, thyroid medications can help you optimize them. Taking thyroid medications can also help reduce symptoms and thyroid antibodies. I’m a big fan of using everything we can to get ourselves better. That said, many people find that thyroid medications do not eliminate all of their symptoms, and they need to address their personal root causes of Hashimoto’s in order to feel better.
You may also find these articles helpful:
ARE YOUR ADRENALS SABOTAGING YOUR HEALTH?
http://thyroidpharmacist.com/articles/are-your-adrenals-sabotaging-your-health
MEDICATIONS FOR HASHIMOTO’S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/
What is the effect of synthroid on (and options for) people with low ferritin (and high iron)?
Hi Sarah, thank you for following. Here is an article that I hope is helpful: https://thyroidpharmacist.com/articles/balancing-iron-levels-can-help-your-thyroid/
Is WP Thyroid still being manufactured? I was called Westhroid in the past I think. Which ones are still bien manufactured other than Armour and NP Thyroid?
Linda – thank you for following. Unfortunately, I do not have more information than what is available to the public. I recommend contacting your practitioner, pharmacist or the manufacturer for more info.
Dr. Wentz,
In your article dated July 19, 2024 on comparing medications, you only mention NP Thyroid one time saying that it has been recalled in the past. I have Hashimoto’s and I have successfully used Acella’s NP Thyroid through all of 2023 and 2024, I feel great and all my labs are optimal. I think the fillers are slightly cleaner than Armour Thyroid. I wanted to let your readers know that it is another T4/T3 option that is currently in production, is working well for me, and has not had any recent recalls.
Sherry – thank you so much for sharing what has worked for you.
Good afternoon, a question about synthetic T3/T4 combo therapy. If recent tests of FT3 is 2.9 (a bit low?) and FT4 is 1.4 (midrange?), TSH 1.92, and trying to raise T3 dosage into optimal range, does the T4 need to be decreased at the same time for balance? I don’t want to worsen the anxiety and edginess, among other symptoms, that I’m trying to fix. Thanks!
Jeff – thank you for sharing. I recommend discussing this with your practitioner who is familiar with you health history to help you determine what will work best for you.
Thank you so much for this great informational article. I had a thyroidectomy in 2011 and did great on a T4/T3 combo for 10 years. First 8 years Levothyroxine and Liothryonine. Then switched to Synthroid and Lio.
But the last several years, I’ve was having all kinds of legs pains, like joint pain and my endo said I was getting too much medication so she lowered it to 112 mcg of Tirosint SOL only. The leg pains went away. I also have huge sleep issues. I also started taking Thryroid glanular in July.
Now after 8 weeks she said levels are too high and today added 5mg of Cytomel and wants me to retest in 6 weeks. My leg pains did go away pretty quick after starting Tirosint SOL but now hip joints are hurting. Does high or low levels of thryoid levels cause these pains?
Krista – thank you for reaching out. I have found that most people will experience pain on some level with Hashimoto’s. For some, it may manifest as a chronic condition, such as migraines or joint pain. I have a great article titled “Natural Solutions to Managing Pain” I will link below. I go through dietary triggers, supplements to help pain, and hidden infections which you may find helpful.
https://thyroidpharmacist.com/articles/pain-management-and-hashimotos/
Dr. Wentz,
Thank you for the info, very helpful for all of us looking for answers and relief. I have a question regarding being in peri-menopause and dealing with hypothyroidism. I’m struggling to determine if my symptoms are menopause related or due to needing a change in my medication. Seems like so many overlapping symptoms—and my labs are within normal range according to doctors but I still feel awful. Trying to figure out what to ask for and where to even start.
Thanks again,
Jenny
Hi Jenny, I understand how hard this is as symptoms can overlap. Here is an article that you might find helpful: https://thyroidpharmacist.com/articles/thyroid-condition-start-worsen-during-perimenopause/
Thank you! I am on a low dose (30 mg) of NP Thyroid and my free T3 isn’t optimal. I am working with a local naturopathic physician on gut health (I have some opportunistic overgrowth) and do take several of the suggested supplements (selenium/myo-inositol, LDN…). Perhaps my thyroid med dosage is still too low, or perhaps I need to add a T3 combination (but I am reluctant due to the short half-life and quick acting and potential side effects). I keep hearing about raw dessicated thyroid supplements (non prescription) from places like Forefront Health. Are they helpful?
Shari, Thank you for your question. If your free T3 isn’t optimal on your current NP Thyroid dose, it’s possible your dose may need adjustment or that adding a T3 medication could be considered under medical supervision. I do not recommend non-prescription raw desiccated thyroid supplements, as they are not regulated and may have inconsistent hormone levels. It’s important to work closely with your healthcare provider to find the safest and most effective treatment for you.
How to get tirosint in Tasmania.
Woman in early 70s tsh suddenly 8. Covid 3 months ago, sinus operation after that. Too many antivirals given.
I’ve been managing subclinical hypo for 10 years without medication. Fairly active.
Worried about fillers in levothyroxine due to allergies and
Various other medical issues eg osteoporosis
Marianne, Thanks for reaching out. Tirosint can be a helpful option for those with sensitivities to fillers, as it’s a clean formulation of levothyroxine without common allergens like gluten, lactose, dyes, or alcohol. While I’m based in the U.S., Tirosint may be available in Australia under a different name or through special order. I recommend speaking with your local pharmacist or practitioner about import options or compounding pharmacies that can provide a cleaner levothyroxine formulation if Tirosint isn’t directly available in Tasmania. A sudden rise in TSH, especially after illness or surgery, can occur due to stress on the thyroid. Given your history and current symptoms, you may want to discuss your concerns with your practitioner to help determine the best options for you. Wishing you continued health and healing!
I have been taking compounded T3 slow release for over 15 years. I currently only take 20mcg in the mornings. My labs are within normal range. I am currently post menopausal and having been dealing with gut issues for several years. I also have adrenal issues that I have been dealing with for over 20 years. Are these issues interrelated? Also, is it possible to wean off the thyroid medication at this point in time and go a more natural route?
Sharon – thank you for sharing your experience. Gut health, adrenal function, and thyroid health are closely interconnected, and imbalances in one area can often impact the others. Many of my readers have found that supporting gut and adrenal health can lead to improved overall well-being. That said, decisions about thyroid medication, especially weaning off, should always be made in partnership with a knowledgeable healthcare provider. While some people have been able to reduce or discontinue thyroid meds through lifestyle changes and root cause approaches, this isn’t appropriate or possible for everyone. Monitoring labs and symptoms closely is essential during any transition.