Female hormones are thought to play a role in the development of autoimmune thyroid conditions. Pregnancy, puberty, and perimenopause (periods of major changes in female hormones) are three of the most common times in a woman’s life for the onset of thyroid disease to occur.
Sex hormones have an important role in modulating the immune system and may impact autoimmune disease. Estrogen can also change the requirements for thyroid hormone, and this may result in an autoimmune condition, especially in the presence of nutrient deficiencies.
While my own thyroid journey started much earlier (likely around puberty), and my thyroid hormones were well balanced in my 30s thanks to taking charge of my own health, I had a dreaded health flare in 2020. This health flare occurred in my late thirties and caused me to have to increase my thyroid meds. I also developed skin issues, anxiety, irritability, weight gain, and insomnia, and had super heavy periods twice per month. 🙁
The health flare happened right when the pandemic started, and I think the cause was likely stress, taking care of a young child 24/7, coming off all of my supplements, having toxic exposure, and transitioning from eating a high protein/low carb diet to skipping breakfast, chugging my thyroid meds with coffee, and subsisting on toddler leftovers for three months. 😉 And perhaps moving closer to 40 may have had something to do with it as well!
I did a lot of detective work to get out of that health flare, which led me to do a deep dive on perimenopause as a trigger and exacerbating factor for Hashimoto’s (and what to do about it to get back into balance).
Perimenopause can start as early as 35, and is a time of hormonal fluctuation where many women struggle with symptoms like fatigue, weight gain, hair loss, and brain fog – symptoms that are often seen in thyroid conditions!
In this article, we explore:
- The thyroid and perimenopause connection
- Symptoms of low progesterone
- Strategies to naturally raise progesterone levels
- How to use topical progesterone to balance hormones
The Thyroid and Perimenopause Connection
Perimenopause refers to the time that the body starts making the transition to menopause. It is usually thought to start between the ages of 40-44, but for some women, it can begin in their mid-thirties! It’s marked by changes in menstrual cycle length, frequency, and flow, as well as changes in hormone levels, including surges in estrogen. It’s also associated with various symptoms that are often brushed off by conventional medicine.
Perimenopause can last anywhere from a few months to a few years, and that transition to menopause is complete once you’ve gone more than 12 months without having a menstrual cycle.
Many women struggle with “hormonal” symptoms during perimenopause, including hot flashes, irregular periods, breast tenderness, fibrocystic breasts, decreased libido, and other symptoms that are similar to PMS.
Additionally, women in perimenopause struggling with hormonal balance may experience non-specific symptoms that may not be obvious symptoms of hormonal imbalance, such as weight gain/increased fat storage (especially in the thighs, hips, and breasts), water retention, fatigue, brain fog, sleep challenges, mood swings, insomnia, headaches, hair loss, and joint pain.
Furthermore, women are more likely to develop a thyroid condition during perimenopause, or experience a worsening of thyroid symptoms, because of the hormonal changes that are happening during this time.
Estrogen dominance is one of the main drivers of perimenopause symptoms and thyroid symptoms. Both estrogen and progesterone start declining during perimenopause, but progesterone declines at a faster rate, resulting in relative estrogen dominance, which you can see illustrated in the chart below (created by my friend and hormone expert, Magdalena Wszelaki, and used with permission).
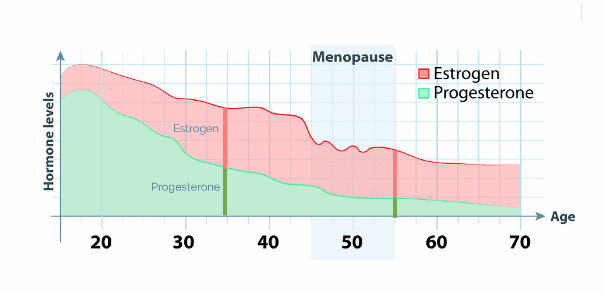
Source: Hormones & Balance, 2019
This means that sometimes a woman may have normal progesterone, but may have symptoms of progesterone deficiency due to a hormonal imbalance caused by estrogen levels that are too high. Other times, women are symptomatic due to unopposed estrogen relative to progesterone, meaning that they have normal estrogen and low progesterone.
When there is estrogen dominance, this can result in poor T4 to T3 conversion, leading to thyroid symptoms.
Please note that low progesterone levels aren’t just of concern for women approaching menopause – it can happen anytime! As you can see on the chart, our progesterone levels start declining in our twenties.
Factor in all the other ways we can end up with higher-than-normal levels of estrogen such as hormonal birth control, poor detoxification, estrogen-mimicking toxins, gut issues, stress, and thyroid conditions – and it’s easy to see how someone could end up with relative estrogen dominance.
Symptoms of Low Progesterone
Progesterone is often known as the hormone necessary for fertility and a healthy pregnancy, but its role is far wider than that. It also influences our mood, sleep, and bone health. It can also help reduce hot flashes and night sweats, and has anti-inflammatory properties.
Having a short luteal phase (the time between ovulation and your period) is a clue you may have low progesterone levels. Other symptoms of low progesterone include: [1]
- Hot flashes and night sweats
- Insomnia and mid-night waking
- Fertility or menstrual problems
- PMS or PMDD
- Anxiety and restlessness
- Irritability and nervousness
- Low mood and depression, especially around ovulation and pre-period
- Mood swings
- Weight gain and cellulite, especially around the thighs and buttocks
- Fluid retention – your fingers and toes swell up
- Brain fog
- Sagging skin
- Low thyroid
- Pain and inflammation
- Osteoporosis
- Excessive menstruation
- Hypersensitivity
- Migraine headaches before cycles
- Decreased libido
- Decreased HDL (“good” cholesterol)
If you are trying to conceive, progesterone is especially important, but having adequate levels at all stages of life is essential for well-being.
How to Naturally Balance Progesterone Levels
The good news is, there are many ways to naturally support your body’s production of progesterone. These are strategies I’ve used personally. 🙂
- Vitamin C: Research shows that women who take vitamin C have significantly increased levels of progesterone. [2] One study showed that women who took 750 mg of vitamin C daily increased their progesterone levels by 77 percent. Vitamin C is also helpful for autoimmune thyroid conditions, as its high levels of antioxidants can help mitigate the high levels of reactive oxygen species (ROS) seen in thyroid conditions. [3] Good food sources of vitamin C include camu camu (Peruvian berry), sweet potato, kiwi, strawberries, oranges, papaya, pumpkin, broccoli, mustard greens, tomatoes, Brussels sprouts, and lemons. Higher doses of vitamin C are often needed to fully benefit from its antioxidant properties, so I typically recommend a supplement. Because I don’t love “horse pills,” I have added vitamin C to my Electrolyte Powder as an easy way to support hormone and energy levels. You can also get a standalone supplement, such as NOW Vitamin C, available via Fullscript. If you don’t have a Fullscript account, you can sign up with my credentials here.
- Zinc: Zinc helps the pituitary gland to release follicle-stimulating hormone (FSH). [4] FSH is needed for ovulation, and it also signals to your ovaries to produce more progesterone. Zinc is also incredibly important for thyroid function, and most people with Hashimoto’s are deficient. A depletion in zinc prevents the conversion of the T4 hormone into the active T3 version. [5] This could lead to symptoms like hair loss, fatigue, and weight gain, even while taking thyroid medications. Zinc is also needed to form TSH, which is why those with hypothyroidism and who are constantly producing TSH, are more likely to develop deficiencies in this important mineral. Oysters, shrimp (prawns), beef, lamb, liver, shellfish, red meat, pumpkin, and cashew nuts are all good food sources of zinc. Pure Encapsulations Zinc is a good option for supplemental zinc. A dose of 30 mg is a good starting point, though some people may need a higher dose (please work with a practitioner if using anything above 30 mg of zinc per day).
- Magnesium: This important mineral can help support progesterone levels by supporting stress and helping you feel calmer. It also assists in the breakdown of the antagonistic estrogen metabolites, which helps to reduce estrogen dominance. [6] I often recommend magnesium for people with thyroid conditions, as it can help with a range of symptoms, including stress, anxiety, muscle pain, and constipation – not to mention, most people are deficient in it! Good food sources of magnesium include cashews, leafy greens such as kale and Swiss chard, pumpkin seeds, black beans, lentils and other legumes, cacao, mackerel fish, and whole grain brown rice. It can be difficult to get enough magnesium from food alone, so I usually recommend a supplement as well, like Rootcology Magnesium Citrate. Please note that the citrate version can have a mild laxative effect, so for people who tend towards diarrhea, I recommend Magnesium Glycinate by Pure Encapsulations. This type of magnesium has been shown to relieve magnesium deficiency on blood tests, but does not loosen stool. However, for some people, magnesium glycinate can worsen anxiety symptoms.
- Vitamin E: Research shows that vitamin E can help to improve luteal blood flow and raise progesterone levels in some women. [7] It’s also an antioxidant, and incredibly important for thyroid health. We can find vitamin E in sunflower seeds, almonds, and hazelnuts, and in smaller amounts in avocado, red peppers, collard greens, pumpkin, asparagus, butternut squash, broccoli, and mango. Vitamin E is an antioxidant at a dose of 268 mg (keep in mind the RDA is 15 mg). I recommend NOW Sun-E 400.
- Vitamin B6: B vitamins help combat stress, and also assist the liver in breaking down estrogen byproducts, which can help reduce estrogen dominance. [8] Studies have shown that 200-800 mg per day of vitamin B6 can raise progesterone levels and reduce estrogen, with noticeable improvements in PMS symptoms. [9] B vitamins are also required for thyroid function. Good food sources include salmon, tuna, bananas, spinach, walnuts, beef, chicken, sweet potato, beans, and prunes. Supplemental B6 may be helpful to ensure you’re getting a high enough dose to boost progesterone levels. That said, I get nervous about vitamin B6 in doses above 300 mg in the pyridoxine form due to the potential for B6 buildup and peripheral neuropathy from a toxic pyridoxine metabolite, or perhaps another biochemical mechanism that is not yet fully understood. [10] Instead, I prefer to focus on the P5P version. I recommend Rootcology P5P.
- Good cholesterol: Cholesterol is needed in your body to make pregnenolone, which is considered the “mother hormone,” as it’s the precursor to many of our hormones, including progesterone. You may have heard that cholesterol is “bad” and you want to keep your dietary intake of cholesterol low. The reality is that, as mentioned, we need adequate amounts of cholesterol to produce hormones in the body. We now know that dietary cholesterol does not translate to blood cholesterol levels in the body, and that there is a weak link between dietary cholesterol consumption and cardiovascular risk. [11] In fact, the 2015–2020 Dietary Guidelines for Americans removed the recommendations to restrict dietary cholesterol to 300 mg/day. You can find good sources of cholesterol in foods like coconut oil, coconut butter, turkey, red meat, eggs (if tolerated), yogurt (if tolerated), olives, and olive oil.
- Fiber: Toxins, waste, and excess hormones like estrogen are detoxified in the liver and then excreted through the stool. Fiber is essential for regular bowel movements, and increasing your intake can be helpful if you’re experiencing constipation, or not having a daily bowel movement. Both soluble and insoluble fiber can be helpful for those who have constipation. Insoluble fiber doesn’t dissolve in water, so it can bulk up stool and help speed up the passage of food through the stomach. [12] This can be helpful for those with hypothyroidism as well, who often experience constipation. Some of the best sources include whole grains, apples, and pears with skin, avocado, almonds, walnuts, and berries. PureLean is one option that I have found to be tasty and easy to add to smoothies.
- L-Arginine: This amino acid is found in high-protein foods. It helps your body make nitric oxide, which helps relax your blood vessels, which increases blood circulation to your ovaries and corpus luteum (which produces progesterone following ovulation). [13] This improved blood flow may help your body produce more progesterone. You can find L-arginine in lentils, chickpeas, salmon, tuna, trout, turkey, chicken, pork, pumpkin seeds, walnuts, and dairy foods (if tolerated). Pure Encapsulations L-Arginine is one potential option.
- Limiting Caffeine: Caffeine intake has been associated with higher levels of estrogen. Soda, tea, and coffee all have the potential to alter estrogen levels and metabolism in a dose-related fashion, but as coffee tends to be much higher in caffeine content compared to tea, it’s often the more likely culprit. [14] One potential mechanism may be due to caffeine causing the adrenals to release more cortisol. If this happens, the body may favor making more cortisol over making progesterone, and this can lead to an imbalance of estrogen. Consuming high levels of caffeine may also deplete B vitamins and magnesium levels, which are necessary for the production of progesterone. [15] Reducing caffeine can help to lower cortisol levels, balance the adrenals, and improve the progesterone to estrogen ratio. I’ve found reducing or eliminating caffeine to be helpful for those with thyroid conditions as well, because of the beneficial effects on the adrenals.
- Myo-Inositol: Myo-inositol is the most abundant inositol form found within the ovary, with approximately 99 percent of the ovarian intracellular inositol being myo-inositol. [16] Myo-inositol also plays a role in producing progesterone, so it can be supportive when trying to boost progesterone levels. Due to its blood sugar-balancing properties, and its ability to reduce thyroid antibodies, reduce TSH levels, and even achieve remission in people with Hashimoto’s, I also love this nutrient for thyroid support. [17] I recommend Rootcology Myo-Inositol Powder.
- Seed Cycling: By eating certain seeds during certain phases of your cycle, you can naturally support progesterone production, and hormone levels in general. During the first half of your cycle (days 1-14), eat 2 tablespoons of fresh ground flax or pumpkin seeds per day (supports estrogen production). During the second half of the cycle (days 15-28), eat 2 tablespoons of fresh ground sunflower seeds or sesame seeds per day (to support progesterone production). Beeya has pre-made blends of the right seeds for the right phases, for an easy way to incorporate seed cycling into daily life.
- Vitex: Vitex is an herb that has long been used to help balance hormone levels and boost progesterone. [18] Pure Encapsulations Vitex is one option.
- CoQ10: For those trying to conceive, CoQ10 has been shown to be helpful, due to its ability to reduce oxidative stress and support the production of other key hormones that produce progesterone. [19] Pure Encapsulations makes a great CoQ10 supplement.
- Balance the Adrenals: Stress is a major hormone disruptor, and is known to lower progesterone levels, not to mention be a potential trigger for Hashimoto’s. Supporting your adrenals and reducing stress may be one of the most important things you can do for thyroid support and hormone balance. This is the topic of my latest book, Adrenal Transformation Protocol. I also created an Adrenal Support supplement that may be helpful.
- Sleep: Sleep and progesterone go hand-in-hand — low progesterone levels have been linked to poor sleep, and conversely, poor sleep may lead to low progesterone levels. [20] Improving the quality and duration of your sleep can help raise progesterone and balance hormones, and hopefully, once progesterone levels are higher, you will have an easier time sleeping. See my article on sleep support for strategies to support sleep.
- Sulfur: In the case of relative estrogen dominance, cruciferous vegetables, which contain glucosinolates (sulfur-rich compounds), are a great way to reduce estrogen levels in the body. Glucosinolates activate phase II detoxification in the liver, helping to filter estrogen metabolites from your body. You may have heard that you should avoid these types of vegetables (also known as goitrogens) if you have a thyroid condition, because of their potential to block absorption of iodine. These vegetables are only truly goitrogenic and affect the thyroid’s absorption of iodine in a raw state, and cooking or fermenting them eliminates the goitrogens. Cruciferous vegetables like broccoli, collard greens, kale, Swiss chard, cauliflower, cabbage, and Brussels sprouts, contain many beneficial nutrients. A supplement like Wellena’s Brocco Power can also be used for extra support.
Balancing Progesterone by Addressing Estrogen Dominance
Progesterone and estrogen work best if they’re in balance. Some women may have enough progesterone, but too much estrogen. In that case, clearing the extra estrogen will be needed. Additionally, some women have too much estrogen and not enough progesterone, so they may need to both clear out excess estrogen AND add more progesterone.
In addition to the estrogen that our body naturally produces, there are also many estrogen-mimicking toxins in our environment, that can build up in the body and act like estrogen. Estrogen-mimicking toxins can disrupt the endocrine system by binding to estrogen receptors. These chemicals can be found in some foods (phytoestrogens), synthetic chemicals, pesticides, plasticizers (BPA), and personal care products.
One of the best ways to clear excess estrogen is by supporting the liver. This is because poor liver (and gut health) can lead to undesirable estrogen metabolites that are responsible for symptoms.
To reduce exposure to estrogen-mimicking toxins, individuals can take steps such as avoiding plastics with BPA, choosing organic foods to reduce pesticide exposure, and using natural and non-toxic personal care products.
To help support your liver in clearing out excess estrogen, I’ve seen great success with calcium D-glucarate, milk thistle, glutathione, antioxidants, sulforaphane, and DIM. Most of these herbs and nutrients are featured in my Liver Reset powder, or can be purchased as standalone supplements via Fullscript (you can sign up with my credentials here).
For further support, I recommend my Root Cause Reset, a four-week program that guides you through gentle liver support, to jump-start your healing, making you feel brighter, happier, and more alive — quickly, without opting for a forceful detox.
I’m excited to announce that I have created a new self-paced version of the program that you can purchase now and begin anytime!
You can also check out this article for more information on liver support.
Using Supplemental Progesterone
While many of these interventions are helpful for many women (especially younger women), sometimes extra support will be needed. This is where using supplemental progesterone can be a game-changer.
Oral and topical progesterone are the two most common options for supplemental progesterone. I personally like topical progesterone (vs. oral), because it bypasses digestion and the liver, which can help to ensure efficient absorption, while reducing the burden on the liver (also, fewer people report nausea with the topical version). If you also have a thyroid condition, the gut and the liver may be compromised, so this can be really helpful.
I love Wellena’s topical progesterone, ProgestPure Cream. ProgestPure Cream is a natural topical progesterone cream providing 25 mg of bioidentical progesterone in every serving (of 4 pumps). This highly bioavailable progesterone cream is very clean, contains a gentle preservative system, and is free of parabens, mineral oil, and petroleum. It has been super helpful for me and my hormones. 🙂
Topical progesterone can be so helpful for some women experiencing perimenopause or a hormonal imbalance. However, there are a few important things to know about using it, and there are certain women who should not use it.
Where to Apply Topical Progesterone and Why
It’s important that you rotate where you apply the topical progesterone, preferably switching between “fatty” and non-fatty areas. Progesterone applied to the more fatty areas will be stored and absorbed more slowly over time, while progesterone applied to areas with less fat will more readily be taken up into the body and be metabolized.
Interestingly, topical progesterone absorption works best in the places where you blush – such as the face, neck, and chest. Rotating the application of progesterone between fatty and less-fatty areas of the body can help to produce both immediate and sustained benefits of topical progesterone.
When to Use Progesterone
Please note that progesterone should not be used continuously. Wellena, the maker of the topical progesterone that I use, recommends the following instructions for whichever stage you’re in:
- Women going through perimenopause, menopause, and post-menopause, and who suffer from sleep disruption, hot flashes, or night sweats, can use topical progesterone for up to 25 days out of a 30-day “cycle,” with 5 to 7 days off, or as recommended by your healthcare provider.
- For women who are still menstruating, topical progesterone can be used for 5 to 7 days after the first day of your period, and continue until the next period begins. Day 1 is the first day of your period. If your period is irregular, start using topical progesterone 7 days after you begin a period and teach your body to learn a new cycle. Stop whenever your period comes back again, and repeat, or apply as recommended by your healthcare provider.
- Women with no ovulation (as in the case of PCOS) can start 7 days after the first day of the period, and continue until the period starts again.
Dosing Recommendations
Dosing will depend on how low your progesterone levels are, and how symptomatic you are. As a pharmacist, I usually recommend starting on the lower end and gradually increasing if needed for most supplements and medications, and progesterone is no exception. 😉
If you choose to use ProgestPure Cream, Wellena recommends starting with four pumps, which will provide 25 mg of bioidentical progesterone. This dose can be doubled to 50 mg per day if symptoms don’t improve.
Another way to dose is using body weight:
- Women under 150 lbs: start with 20-30 mg of bioidentical progesterone.
- Women over 150 lbs: start with 40-50 mg of bioidentical progesterone.
If you want to try a higher dosage, I recommend working with a skilled functional practitioner who knows the ins and outs of bioidentical hormones, and can test your levels.
Generally speaking, I have found that while many supplements and medications can be taken “whenever you remember them,” and still have pretty decent results, they work best with consistent dosing and timing. Skipping a day or two can cause menstrual spotting.
Risks of Topical Progesterone
For some women, topical progesterone can be a lifesaver, but it’s not for everyone. Here are some potential side effects and risks, as well as who shouldn’t use topical progesterone:
- Side effects from progesterone aren’t common, but they do happen. Some women have reported weight gain, insomnia, lumpy breasts, bigger fibroids, feeling dizzy, lightheaded, angry or depressed, experiencing rising heart rate, and water retention. Using topical progesterone, versus oral, reduces, but does not eliminate, the risk of these side effects.
- Women with progesterone receptor-positive breast cancer should not use topical progesterone, even though progesterone is likely not the main culprit in this form of breast cancer. According to functional oncologists and functional endocrinologists, the problem is in how the body breaks down progesterone (they can turn into “dirty” progesterone metabolites).
- Women with abnormal vaginal bleeding that is not due to their menstrual cycle, should not use progesterone or any other hormone therapy until a diagnosis is made.
Takeaway
Whether you recently discovered you have low progesterone levels for another reason or are in the thick of perimenopause, there are many strategies to support progesterone production! As a bonus, many of these strategies also support thyroid function, and can help you feel better, whether or not you have a thyroid condition.
I know that hormonal imbalances can be frustrating, especially if you’re not feeling well because of them. As someone who has corrected my own hormonal imbalances many times, and helped other women in all stages of life balance their hormones, I assure you — it will happen!
I hope this encourages you, and I wish you all the very best on your healing journey! 🙂
P.S. You can download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free by signing up for my newsletter. You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow me on Facebook, Instagram, TikTok, and Pinterest!
References
[1] Cable JK, Grider MH. Physiology, Progesterone. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 1, 2023.
[2] Mumford SL, Browne RW, Schliep KC, et al. Serum Antioxidants Are Associated with Serum Reproductive Hormones and Ovulation among Healthy Women. J Nutr. 2016;146(1):98-106. doi:10.3945/jn.115.217620
[3] Khordad E, Alipour F, Beheshti F, et al. Vitamin C prevents hypothyroidism associated neuronal damage in the hippocampus of neonatal and juvenile rats: A stereological study. J Chem Neuroanat. 2018;93:48-56. doi:10.1016/j.jchemneu.2017.11.011; Farasati Far B, Behnoush AH, Ghondaghsaz E, Habibi MA, Khalaji A. The interplay between vitamin C and thyroid. Endocrinol Diabetes Metab. 2023;6(4):e432. doi:10.1002/edm2.432
[4] Garner TB, Hester JM, Carothers A, Diaz FJ. Role of zinc in female reproduction. Biol Reprod. 2021;104(5):976-994. doi:10.1093/biolre/ioab023
[5] Nishiyama S, Futagoishi-Suginohara Y, Matsukura M, et al. Zinc supplementation alters thyroid hormone metabolism in disabled patients with zinc deficiency. J Am Coll Nutr. 1994;13(1):62-67. doi:10.1080/07315724.1994.10718373
[6] Kolanu BR, Vadakedath S, Boddula V, Kandi V. Activities of Serum Magnesium and Thyroid Hormones in Pre-, Peri-, and Post-menopausal Women. Cureus. 2020;12(1):e6554. Published 2020 Jan 3. doi:10.7759/cureus.6554
[7] Takasaki A, Tamura H, Taniguchi K, et al. Luteal blood flow and luteal function. J Ovarian Res. 2009;2:1. Published 2009 Jan 14. doi:10.1186/1757-2215-2-1
[8] Rose DP. The interactions between vitamin B6 and hormones. Vitam Horm. 1978;36:53-99. doi:10.1016/s0083-6729(08)60982-6
[9] Abraham GE. Nutritional factors in the etiology of the premenstrual tension syndromes. J Reprod Med. 1983;28(7):446-464.
[10] Hadtstein F, Vrolijk M. Vitamin B-6-Induced Neuropathy: Exploring the Mechanisms of Pyridoxine Toxicity. Adv Nutr. 2021;12(5):1911-1929. doi:10.1093/advances/nmab033
[11] Soliman GA. Dietary Cholesterol and the Lack of Evidence in Cardiovascular Disease. Nutrients. 2018;10(6):780. Published 2018 Jun 16. doi:10.3390/nu10060780
[12] Erdogan A, Rao SS, Thiruvaiyaru D, et al. Randomised clinical trial: mixed soluble/insoluble fibre vs. psyllium for chronic constipation. Aliment Pharmacol Ther. 2016;44(1):35-44. doi:10.1111/apt.13647
[13] Faustmann G, Meinitzer A, Magnes C, et al. Progesterone-associated arginine decline at luteal phase of menstrual cycle and associations with related amino acids and nuclear factor kB activation. PLoS One. 2018;13(7):e0200489. Published 2018 Jul 10. doi:10.1371/journal.pone.0200489
[14] Sisti JS, Hankinson SE, Caporaso NE, et al. Caffeine, coffee, and tea intake and urinary estrogens and estrogen metabolites in premenopausal women. Cancer Epidemiol Biomarkers Prev. 2015;24(8):1174-1183. doi:10.1158/1055-9965.EPI-15-0246
[15] Ulvik A, Vollset SE, Hoff G, Ueland PM. Coffee consumption and circulating B-vitamins in healthy middle-aged men and women. Clin Chem. 2008;54(9):1489-1496. doi:10.1373/clinchem.2008.103465; Bergman EA, Massey LK, Wise KJ, Sherrard DJ. Effects of dietary caffeine on renal handling of minerals in adult women. Life Sci. 1990;47(6):557-564. doi:10.1016/0024-3205(90)90616-y
[16] Unfer V, Nestler JE, Kamenov ZA, Prapas N, Facchinetti F. Effects of Inositol(s) in Women with PCOS: A Systematic Review of Randomized Controlled Trials. Int J Endocrinol. 2016;2016:1849162. doi:10.1155/2016/1849162
[17] Fallahi P, Ferrari SM, Elia G, et al. Myo-inositol in autoimmune thyroiditis, and hypothyroidism. Rev Endocr Metab Disord. 2018;19(4):349-354. doi:10.1007/s11154-018-9477-9; Nordio M, Basciani S. Treatment with Myo-Inositol and Selenium Ensures Euthyroidism in Patients with Autoimmune Thyroiditis. International Journal of Endocrinology. 2017;2017:2549491. doi:10.1155/2017/2549491.
[18] Shaw S, Wyatt K, Campbell J, Ernst E, Thompson‐Coon J. Vitex agnus castus for premenstrual syndrome. Cochrane Database Syst Rev. 2018;2018(3):CD004632. Published 2018 Mar 2. doi:10.1002/14651858.CD004632.pub2
[19] Thakur AS, Littaru GP, Funahashi I, Painkara US, Dange NS, Chauhan P. Effect of Ubiquinol on Serum Reproductive Hormones of Amenorrhic Patients. Indian J Clin Biochem. 2016;31(3):342-348. doi:10.1007/s12291-015-0542-9
[20] Beroukhim G, Esencan E, Seifer DB. Impact of sleep patterns upon female neuroendocrinology and reproductive outcomes: a comprehensive review. Reprod Biol Endocrinol. 2022;20(1):16. Published 2022 Jan 18. doi:10.1186/s12958-022-00889-3; Sharkey KM, Crawford SL, Kim S, Joffe H. Objective sleep interruption and reproductive hormone dynamics in the menstrual cycle. Sleep Med. 2014;15(6):688-693. doi:10.1016/j.sleep.2014.02.003
Note: Originally published in September 2023, this article has been revised and updated for accuracy and thoroughness.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Hi would love to have this cream but it does not deliver to UK. Can you recommend a UK version?
Thanks
Abigail – thank you for reaching out. Please email my team at info@thyroidpharmacist.com and they will be happy to share my international recommendations.
What about cases of low estrogen ?
Have you seen any references to people having hormonally influenced PVCs (heart premature Ventricular Contractions), that resolved by improving their hormone balance by supplementing with progesterone? I have been working through this this past year post-partum at age 42/43, and finally got some relief after working on my hormones.
Hi, what numbers would you call normal (or low/high)? — and does the cycle day of testing matter?
Les – Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. When it comes to testing,if you are taking T4 only, you can go ahead and take your medication in the morning before the test. T4 medication has a long half-life, and your levels will be stable regardless of when you take it. If you take a T3 medication, or a combination T3/T4, T3 has a shorter half-life so your blood work may not be reflected accurately. It will appear that you have more thyroid hormone on board than you do. Thus it may be helpful to delay your morning dose of a T3/T4 medication until after you do the test to see (try to schedule the test in the morning). Here are a couple articles that I hope are
helpful:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
HOW TO GET ACCURATE LAB TESTS WHEN TAKING THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/how-to-get-accurate-lab-tests-when-taking-thyroid-medications/