From my own personal experience with Hashimoto’s, I know that diet and food are one of the best ways that we can address Hashimoto’s symptoms, feel better, and even put the condition into remission. In the early years of my journey toward healing, I tried just about every diet out there in order to feel better… some with better results than others.
Eventually, I landed on a way of eating that looks a lot like a modified Paleo-style diet and now I feel better than ever, but I always like to remind my clients and readers that there is no one diet out there that will be a cure-all for everyone. Most of us will have to do some trial and error, elimination, and investigation to land on what works best for our own bodies.
One of the diets that I have found to be helpful for a percentage of people with Hashimoto’s — especially those dealing with SIBO (small intestine bacterial overgrowth) — is the low FODMAP diet. While the name sounds a bit funny, the diet itself has a great track record for relieving irritable bowel syndrome (IBS) symptoms and could be a good starting place for some people with Hashimoto’s.
In this article, I’ll go into more detail on:
- What are FODMAPs?
- How FODMAPs help with IBS
- How FODMAPs can affect Hashimoto’s
- What a low FODMAP diet looks like
- Further resources to follow a low FODMAP diet
What are FODMAPs?
FODMAPs are a collection of short-chain carbohydrates (sugars) that occur naturally in a variety of foods. (I’ll share which foods are high in FODMAPs further on in this article.) These carbohydrates aren’t absorbed properly in the intestines of those with IBS and certain intestinal disorders; and they can trigger symptoms such as abdominal pain, bloating, gas, diarrhea and constipation.
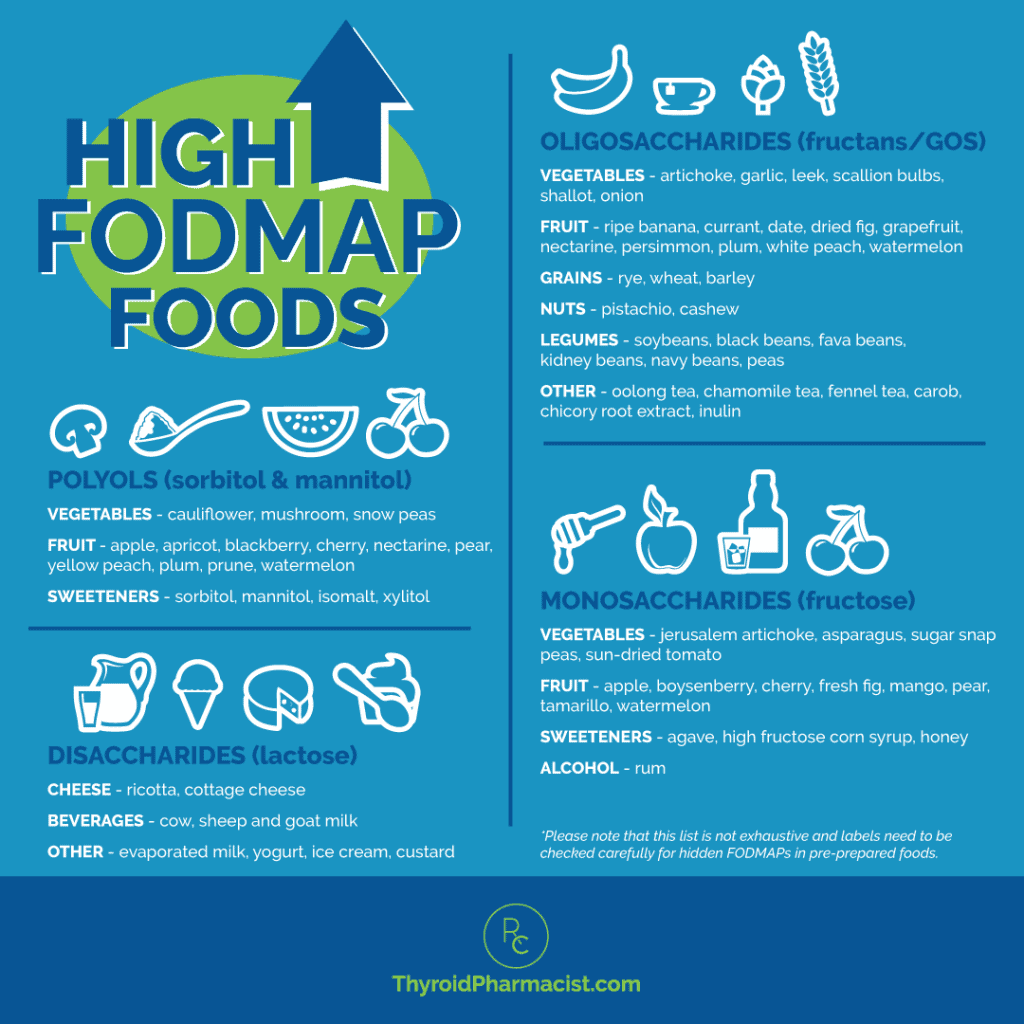
The term FODMAP is an acronym for the categories of carbohydrates that have proven to be problematic:
- Fermentable: Fermentation is the process through which gut bacteria ferment undigested carbohydrates, which in turn can produce intestinal gases.
- Oligosaccharides: These include fructans and GOS (galacto-oligosaccharides or galactans), which can be found in foods such as wheat, rye, onions, garlic and legumes.
- Disaccharides: Lactose – found in dairy products like milk, soft cheeses and yogurt.
- Monosaccharides: Fructose – found in honey, high fructose corn syrups, and many fruits, such as apples.
- And
- Polyols: Sorbitol & mannitol – found in some fruit and vegetables and used as artificial sweeteners.
FODMAPs and IBS
Irritable bowel syndrome (IBS) is a chronic disorder that affects the large intestine with symptoms such as cramping, abdominal pain, bloating, gas, and either diarrhea or constipation, or both. For some people diagnosed with IBS, symptoms are mild and can be managed with diet and lifestyle interventions. Other people experience more severe symptoms that may need to be managed with medications. It is a relatively common disorder, with an estimated 10-20 percent of the global population being affected.
The symptoms of IBS tend to wax and wane, and can be triggered by food intolerances, stress, and hormonal changes. There is no definitive test for IBS, but it is usually diagnosed based on the presence of gastrointestinal symptoms when other conditions (such as celiac disease) have all been ruled out. While the precise cause of IBS isn’t known, there are several factors that have been shown to play a role:
- Damage to the intestinal wall. The walls of the intestines are lined with layers of muscle that contract as they move food through your digestive tract. When these muscles have suffered damage, such as in the case of intestinal permeability or leaky gut (a common pre-existing factor for those who develop Hashimoto’s), contractions that are stronger than normal can cause gas, bloating and diarrhea. Weak intestinal contractions can slow food passage and lead to constipation.
- Nervous system abnormalities. A disruption to the signals between the brain and the intestines can cause your body to overreact to changes that normally occur in the digestive process, resulting in pain, diarrhea or constipation.
- Inflammation in the intestines. Some people with IBS have an increased number of immune-system cells in their intestines, which can result in pain and diarrhea.
- Infection. IBS can develop after a severe gut infection caused by bacteria or a virus. It may also occur as a result of a surplus of bacteria in the intestines (ie. as is the case with small intestinal bacterial overgrowth).
- Changes in bacteria in the gut. Microflora are the “good” bacteria that reside in the intestines and play a key role in health, and there is some indication that microflora populations might differ in those with IBS. While lifestyle factors such as diet, certain medications, stress, and invasive medical procedures can all influence one’s gut microflora. A previous infection, the use of antibiotics, dietary allergies and food sensitivities have all been associated with IBS.
When FODMAPs are consumed by people with IBS, they are rapidly fermented by the bacteria living in the intestines. By pulling more water into the gut, the FODMAPs can cause more gas to be produced. This results in bloating and distension, and impacts the ability of the gut to contract properly. It is the reason why so many people with IBS suffer from either loose bowels or constipation.
Removing FODMAP-containing foods from one’s diet has been shown to relieve many of the symptoms of IBS and is often recommended as a dietary intervention for people living with the condition.
How Do FODMAPs Affect Hashimoto’s?
In my survey of 2232 people with Hashimoto’s, I found that 30 percent of them felt better on a low FODMAP diet. I believe that this benefit may be seen because a large number of people with Hashimoto’s have small intestine bacterial overgrowth (SIBO), which is often a trigger for IBS and can be improved with a low FODMAP diet.
What is SIBO?
The small intestine is designed to be relatively clear of bacteria, while the large intestine houses most of our intestinal bacteria. In some cases, bacteria from the large intestine may make their way up and overgrow into the small intestine.
Once bacterial overgrowth has taken place in the small intestine, it can lead to intestinal permeability and a long list of digestive symptoms, including acid reflux, belching, bloating, constipation and diarrhea. SIBO often presents with bloating after eating, caused by bacteria in the small intestine forming excess gas.
When fibrous foods, fermented foods, histamine-containing foods, prebiotics, cruciferous veggies, or the use of probiotics cause a flare up in digestive symptoms, it is very likely that an overgrowth of bacteria is present in the small intestines.
Conditions like IBS, hypothyroidism, fibromyalgia, and restless leg syndrome have all been tied to SIBO. It is estimated that over 50 percent of people with hypothyroidism also have SIBO.
SIBO is a very important root cause, and I’ve written a great article on SIBO and Hashimoto’s that summarizes the causes, tests, and treatment options for SIBO, including the low FODMAP approach. This article will go a bit deeper into the low FODMAP approach so that you’ll have a good idea on how to implement it.
Using the low FODMAP Diet to Relieve SIBO
By removing foods high in fermentable sugars, the low FODMAP diet essentially cuts off the food supply to the bad bacteria that may be growing out of control in the intestines.
In other words, by avoiding the foods that are to be fermented by the pathogenic flora, a low FODMAP diet can help eradicate SIBO by potentially starving the pathogenic flora and by allowing the good flora we need for absorption to multiply without resistance from the bad bacteria.
Essentially, it is an elimination diet that avoids the carbohydrates that could be fermented by gut bacteria and contribute to gut-related symptoms. However, in more severe cases, diet alone may not be enough to eradicate SIBO, and other forms of treatment, such as antibiotics and probiotics, may need to be pursued.
What Does a Low FODMAP Diet Look Like?
The goal of the low FODMAP diet is to allow the gut to heal and to, eventually, reintroduce certain foods back into the diet over a controlled period of time. It is recommended that the strict low FODMAP diet (elimination of all high FODMAP foods) be followed for 2 to 6 weeks. After the reintroduction of high FODMAP foods that you are able to tolerate, you will land on your own version of the low FODMAP diet that you may stay on for a longer period, depending on how long it takes your gut to heal. When working to heal your gut, you will want to look for a resolution of symptoms such as diarrhea or constipation, bloating, acid reflux, gas, and stomach pain.
After the initial restrictive diet, many people are able to reintroduce most foods, with just a few high FODMAP foods that need to be avoided in large amounts. There is some indication that following a strict low FODMAP diet in the long term can reduce levels of certain beneficial bacteria in the gut, so it is not recommended that you follow an unnecessarily strict low FODMAP diet indefinitely.
The low FODMAP diet is really about monitoring your reaction to high FODMAP foods and finding a diet that suits your individual body. As such, you will test each group of food to see how your body reacts to it, eliminating the ones that cause negative reactions for you, in order to give your gut the chance to heal.
The low FODMAP diet is divided into three stages:
Stage 1: Start the Low FODMAP Diet
You’ll eliminate all high FODMAP foods for a period of 2 to 6 weeks. Wait to move on to the next stage of the diet until your gastrointestinal symptoms have been relieved. If you experience a relief of your symptoms within that timeframe, you’ll move on to the next stage. If you are still experiencing symptoms, it might be time to try a different dietary approach or undergo food sensitivity testing. (You can read more about food sensitivity testing here.)
Stage 2: Reintroduce FODMAP Foods
During the re-introduction phase, you will reintroduce higher FODMAP foods back into your diet, focusing on one subcategory of FODMAPs at a time. This helps to determine which types of FODMAPs you tolerate, as few people are sensitive to all of them. It also helps to establish the amount of FODMAPs you can tolerate.
In this stage, you will test specific FODMAP groups one by one, for three days each. Note your reactions, if any, during this time period. Try foods in different quantities at different times, and note your reactions. For example, if you are testing monosaccharides (by reintroducing fructose-containing foods), try one slice of apple and see how you react. Wait a few hours, then try eating a whole apple and note any reactions you experience. As soon as you experience symptoms, stop eating that food. This will give you an idea of your tolerance level for that type of food (e.g. none at all, only a couple of bites, etc.) An immediate reaction is an indication that you are highly sensitive to that food group and may need to avoid it for a longer period of time.
After three days of testing one subgroup of FODMAPs, move to another group and test foods in that category.
You don’t need to try all sources of food in each category to determine if the foods in that particular category are problematic for you. Remember, we are not looking for food allergies here, rather we are eliminating categories of food whose particular form of carbohydrate is not broken down well by the gut bacteria.
It is important to continue a low FODMAP diet throughout the reintroduction stage. This means that even if you can tolerate a specific high FODMAP food, you should continue to restrict it until Stage 3.
It is also important to note that, unlike people with most food allergies, people with IBS can tolerate small amounts of FODMAPs.
Stage 3: Personalize Your FODMAP Diet
After testing all of the food groups during the reintroduction stage, you will be able to reintroduce the foods that you are able to tolerate back into your diet. Although individual FODMAP tolerance levels vary, most people find that they don’t have to be as strict about their FODMAP intake as they were during the initial stage, as some of the food groups may not cause any reactions for them, or may only cause a reaction in large quantities. Many people are able to reintroduce quite a few high FODMAP foods back into their diet, but may not be able to eat them as often, or in the same quantity, as they did before.
After about three months of staying away from the food groups that you reacted to, you can once again try to reintroduce them into your diet. The goal is that, with time, you will eventually be able to heal your gut and tolerate each sub-category of FODMAPs.
One caveat for those with Hashimoto’s is that I recommend removing gluten and dairy completely from the diet and skipping such foods during the reintroduction stage. A few people with Hashimoto’s are able to tolerate those foods, but I have found that most do better long term by eliminating them. (Find out why I recommend avoiding gluten and dairy for most people with Hashimoto’s in these articles.)
What Foods Are Included on the Low FODMAP Diet?
The low FODMAP diet allows some fruits, but advises against eating too many of them. Bananas, blueberries, boysenberries, cranberries, grapes, grapefruit, honeydew melon, kiwi, lemons, limes, oranges, raspberries, and strawberries are allowed.
Vegetables included on the low FODMAP diet are carrots, celery, endives, ginger, green beans, lettuce, olives, parsnips, potatoes, pumpkin, red bell peppers, spinach, squash, sweet potatoes, tomatoes, turnips, and zucchini, as well as most herbs.
Gluten free cereals and grains, such as rice, oats, polenta, quinoa, psyllium, sorghum, tapioca, and arrowroot are allowed.
Most dairy products are not permitted unless they are lactose free. Sweeteners such as sugar and maple syrup are allowed, but not in large quantities.
Meats and eggs are not restricted on the low FODMAP diet, as they do not contain fermentable carbohydrates.
For those following another type of diet, such as Paleo or gluten free, modifications can be made to the low FODMAP diet to meet your specifications. Examples of how you may want to modify your diet include:
- Gluten Free: Eliminate all gluten-containing grains (wheat, barley, and rye in all variations).
- Dairy Free: Eliminate all sources of dairy, including lactose free dairy products.
- Paleo: Eliminate all grain, dairy, legumes, and processed food products. Focus on meats and low FODMAP vegetables and fruit.
- Autoimmune Paleo: Avoid all processed foods, grains, legumes, dairy, eggs, soy, sugar, food additives, alcohol, and most nuts and seeds. Focus on pasture-raised meats, and low FODMAP fruits and vegetables.
Though the low FODMAP will look different for individuals, a typical day on the diet for a person following an Autoimmune Paleo diet might look something like this:
Breakfast: Rosemary Sweet Potato Hash
Lunch: Balsamic Chicken Thighs with Herbed Mashed Potatoes
Dinner: Parsnip and Shrimp Slaw
Snack: Coconut Berry Salad
For these recipes, and more, download my free Root Cause Recipes One Week Low FODMAP Autoimmune Meal Plan below!
This infographic should help you understand the four different categories of FODMAPs and the foods that have the highest content of fermentable carbohydrates in each one:
Resources to Help Navigate the Low FODMAP Diet
It can be a bit overwhelming when you start out on a low FODMAP diet, as the list of foods to avoid may seem long and can be complicated by the need to take into account the volume of the FODMAPs you are eating.
Fortunately, there are many resources online to help you navigate the diet. The foremost of these is Monash University in Australia, where the diet originated. Their website includes lists of foods to eat and avoid on the diet, as well as a very useful app that includes a guide to the low FODMAP diet.
A few final notes…
The low FODMAP diet is a way to eliminate, challenge, and reintroduce certain categories of food that can be particularly problematic for a lot of people with IBS, SIBO and Hashimoto’s. Most people who go on this diet find that some FODMAPs are well tolerated, while others cause mild to severe symptoms. While it’s possible that some people will find that they need to avoid certain foods for a longer period of time, most will be able to rechallenge and reintroduce those foods in the future, as their body heals from the removal of problematic foods, and as they rebalance their gut flora.
I always like to remind people that there is no “one size fits all” diet for Hashimoto’s, and that each individual will need to do some experimenting to find the diet that works best for them. And that diet will likely change over time as new foods are tolerated, or other foods may need to be eliminated for a period.
The goal is to find a way of eating that is sustainable for you and provides you the most relief from your symptoms. For some, that will be a Paleo or Autoimmune Paleo approach. Others may need to do an elimination diet to get to the root of their food sensitivities, while some people will need to undergo food sensitivity testing by a lab to help them uncover the foods that are causing their reactions.
A low FODMAP diet can be very effective for those dealing with SIBO or symptoms of IBS, but it is only one approach. Some people have found that an Elemental Diet, herbal remedies, medications, prokinetics, LDN, or other specific approaches are needed to truly eradicate SIBO (see my full article on the various approaches). As always, I encourage you to keep digging until you find the way of eating that works for you and allows you to live your best life!
P.S. You can download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter for free by signing up for my newsletter. You will also receive occasional updates about new research, resources, giveaways and helpful information.
For future updates, make sure to follow us on Facebook too!
References
- The Low FODMAP Diet. Monash University. https://www.monashfodmap.com/. Accessed August 14, 2018.
- Irritable Bowel Syndrome. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016. Accessed August 14, 2018.
- Kwiatkowski L, Rice E, Langland J. Integrative Treatment of Chronic Abdominal Bloating and Pain Associated With Overgrowth of Small Intestinal Bacteria: A Case Report. Altern Ther Health Med. 2017 Jul;23(4):56-61.
- Zannini E, Arendt EK. Low FODMAPs and gluten-free foods for irritable bowel syndrome treatment: Lights and shadows. Food Res Int. 2018 Aug;110:33-41. doi: 10.1016/j.foodres.2017.04.001.
- Dieterich W, Schuppan D, Schink M, Schwappacher R, Wirtz S, Agaimy A, et al. Influence of low FODMAP and gluten-free diets on disease activity and intestinal microbiota in patients with non-celiac gluten sensitivity. Clin Nutr. 2018 Apr 4. S0261-5614(18):30129-8. doi: 10.1016/j.clnu.2018.03.017.
- Distrutti E, Monaldi L, Ricci P, Fiorucci S. Gut microbiota role in irritable bowel syndrome: New therapeutic strategies. World J Gastroenterol. 2016 Feb 21; 22(7): 2219–2241.
- Patil AD. Link between hypothyroidism and small intestinal bacterial overgrowth. Indian J Endocrinol Metab. 2014 May-Jun; 18(3): 307–309.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Thank you so much for this information. It has improved the quality of my life greatly.
Marianne – you are very welcome! <3 I appreciate your support! I hope you will keep me posted on your progress.
I have been taking thyroid hormone for over 40 years. Recently I discovered that grapefruit, soy and raw cabvage family and gluten is an absolute no no for hypothyrodism. Please do not advise grapefruit. It intetfears with many medications blocking the proper functions. Ie for excample. Blood pressure and cholestrol medications as well as thyroid hormones.
Cecilia – thank you so much for sharing!
Izabella, have you seen anyone seeing a drop in anti tpo following goitrogen restriction? I had a huge drop while on holiday were I made some changes, primarily excluding goitrogens, my antibodies went from 1360 to 520. I am wondering if this could be it? I was already eating paleo prior.
Titti – thank you for reaching out. Most cruciferous vegetables and goitrogen-containing foods are safe for those with Hashimoto’s. However, if you seem to react to them, you may wish to look into SIBO, sulfur sensitivity, iodine deficiency and the CBS gene mutation. Here is an article I wrote that has more details you might find helpful:
WHAT ARE GOITROGENS?
https://thyroidpharmacist.com/articles/what-are-goitrogens-and-do-they-matter-with-hashimotos/
I am so confused. I have Hashi’s and have been off of dairy, soy, sugars, gluten, seeds, nuts, processed foods, night shades, grains, etc. for 2 years now. Still have inflammation 🙁 The FODMAP plan has some of those “dont’s” such as night shades. Please help!
Jan – thank you for reaching out and sharing your journey. I am so sorry you are struggling with all of this. <3 I know how overwhelming everything can be. Gut healing is a journey; you may need various interventions like removing reactive foods and infections, taking enzymes and probiotics, and balancing nutrients. Remember, be kind to yourself and learn to listen to your body so that you can support and feed it properly! You are worth it! You may find this article helpful as well!
WHAT'S CAUSING YOUR LEAKY GUT
https://thyroidpharmacist.com/articles/whats-causing-your-leaky-gut/
6 DIFFERENT ROOT CAUSES
https://thyroidpharmacist.com/articles/6-different-hashimotos-root-causes/
SUPPLEMENTS ACTUALLY HELP HASHIMOTO’S
https://thyroidpharmacist.com/articles/which-supplements-actually-help-hashimotos/
Hello Doctor Izabella,
Two months ago I was given levothyroxine (50mcg) 1x a day. I took it for the two months and it did bring my tsh down from 45! to 13. I’ve never had any hypo symptoms, other then some constipation. I had to stop the levothyroxine. It became very toxic to me. Awful joint, muscle and tendon pain and hair thinning. It has now been a week off medicine, drinking lots of water, and pain is somewhat better. My primary care now whats me to see an endo who does not agree with natural approaches which means more medication! I do know of an endo who perscribes amour dessicated thyroid. Would there be side affects from amour as well? I am normal weight and height. My appt is in a month. Before I see another doctor, I would like to try a better diet as you suggested, take supplements and see if that would bring down the tsh. (also t4free is low .72.) Is that ok to try for a month with my tsh so high? Also could doing this bring down the tsh on its own? Thank you Doctor Izabella for any advice you can give me. Much appreciated. Theresa
Theresa – thank you for reaching out. I am so sorry you experienced this! I understand how frustrating this can be. <3 There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication which you are looking for, ask your local pharmacist for doctors in your area who prescribe the medication you are looking to try. Have you read these articles?
WHICH THYROID MEDICATION IS BEST?
https://thyroidpharmacist.com/articles/which-thyroid-medication-is-best/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
I am on a vegetarian diet. What do you recommend as a substitute for protein??
Sandra – thank you for reaching out. <3 Pea protein is an alternative that may be easier to digest and is less likely to cause food sensitivities. I have created my own line of supplements, which also includes an Organic Pea Protein. Here's the link: https://rootcology.com/collections/supplements/products/copy-of-purepaleo-protein-vanilla
Eggs, some seeds, and nuts would be the preferred sources of protein for vegetarians. However, some people with Hashimoto’s may be intolerant to those as well, especially in the early stages of starting a healing diet. Being a vegan is even more challenging, and nuts and seeds would be the go-to source of protein, which are usually too difficult to digest for many in the beginning of their thyroid healing journeys.
While vegan and vegetarian diets have been reported to be extremely helpful with autoimmune and chronic conditions, I have not been able to find reports of people recovering from Hashimoto’s by following a vegan diet. Even devout vegans who are nutritionally conscious still struggle with low body temperatures, hypothyroidism and Hashimoto’s.
Many former vegans have reported improved symptoms of Hashimoto’s following transitioning to a Paleo diet. Based on this, I believe that animal proteins must play an important role in building back the health of people with Hashimoto’s. That said, while meats and fats are important for healing, eating them exclusively will produce an acidic environment in the body, hindering healing, and thus the diet should be balanced with plenty of nutrient rich vegetables (suggested ratio may be 20% meat/80% veggie).
Additionally, vegan and raw vegan diets can be extremely helpful for cleansing and detoxifying, especially for those with persistent protein digestion issues. A vegan diet can be followed for a few days to a few weeks and may help the body detoxify. B12 and iron or ferritin supplements should be utilized at this time to prevent deficiency. Please know that I’m a big proponent of bio-individuality which honors the distinct nutritional needs of every human being. I’m not saying everybody needs to eat meat, but I am saying to listen to your body if it needs meat. Here are a few articles which might help:
AUTOIMMUNE PALEO DIET
https://thyroidpharmacist.com/articles/autoimmune-paleo-diet
ELIMINATION DIET FOR HASHIMOTO’S
https://thyroidpharmacist.com/articles/elimination-diet-for-hashimotos
Dr.Wentz, I have been a Hashimoto patient for almost 40 years. I lived in Holland and worked as an RN in a hospital and moved to the USA at age 27. With the great guidance of Suzanne Tershak (FNP-BC) I have followed your protocol since last August with excellent results. My leaky gut has improved a lot and I cannot mention enough of your knowledge to friends of mine with the same problems. My antibodies used to be between 17.000 and sometimes even over 20.000. They went down from 6800 to 1800 and to 989!! I have lost weight and I am on a strict no dairy no gluten diet. My question is that I am still struggling with my lower back pain for the last year and a half. The Doctor has given twice steroid shots with good results for a while. The MRI shows arthritis and deterioration of the lower spine. Ibuprofen, even I do not like to take it, does work for the inflammation but as soon as I discontinue, the inflammation comes back. So my question: Am I still eating the incorrect food? Being raised in Holland, bread has always been part of our dietary routine. So eating gluten free bread has been a great replacement for the regular bread I used to eat. Now my question: Would the grains made of the gluten free bread be a cause for inflammation? I am looking forward getting your opinion on this matter. Henriette Brecheisen
Henriette – thank you for reaching out. I’m happy to hear you are taking charge of your health, have found a practitioner to work with you and are seeing results! <3 The most common food sensitivities found in people with Hashimoto’s are gluten, dairy, soy, grains, nightshades (potatoes, tomatoes, and peppers), nuts, and seeds. Did you know that reactive foods trigger an inflammatory response in the GI tract, leading to malabsorption of nutrients (gluten sensitivity, in particular, has been implicated in causing a Selenium deficiency, a well-known risk factor for Hashimoto's), and can also produce intestinal permeability whenever they are eaten? Most people will see a dramatic reduction in gut symptoms, brain symptoms, skin breakouts, and pain by eliminating the foods they are sensitive to. Some will also see a significant reduction in thyroid antibodies! An additional subset of people will actually be able to get their Hashimoto's into complete remission just by getting off the foods they react to, normalizing their thyroid antibodies, and some even normalizing their thyroid function! Here are a couple of articles you may find helpful.
FOOD SENSITIVITIES AND HASHIMOTO'S
https://thyroidpharmacist.com/articles/food-sensitivities-and-hashimotos
AUTOIMMUNE PALEO DIET
https://thyroidpharmacist.com/articles/autoimmune-paleo-diet
In the article it seems like FODMAP sensitivity, small indestine bacterial overgrowth, leaky gut and irritable bowel syndrome are all associated with digestive problems. So if I have Hashimoto’s and experience systemic problems, but no digestive issues, does that imply that I belong to the 70% who will not benefit from a low FODMAP diet?