Sponsored Post: This post is sponsored by Tirosint. However, all thoughts and opinions expressed are those of Dr. Izabella Wentz. More information about IBSA Pharma can be found here.
Over the last few weeks, many of us have put our efforts into current world affairs and may have put some of our goals and chronic needs on hold. My goal is to always share information that I hope will serve you best… This week, I want to switch gears from talking about world affairs, and get back into giving you specific and actionable information that can help you with your thyroid health. Regardless of what’s going on in the world, when we have a chronic condition, it’s imperative that we take care of ourselves. This article on a new thyroid medication option is long overdue, and I hope it will help you on your healing journey!
As a pharmacist trained in conventional, integrative, functional, and natural medicine, I have a deep respect for various healing modalities… including medications, which will be the focus of this week’s article. While I agree with some of my colleagues in natural medicine that medications can be overused, my years of experience as a clinical consultant pharmacist have also taught me that medications are often underutilized and used inappropriately.
I certainly see this all of the time with respect to thyroid medications. People with overt thyroid symptoms are denied thyroid medications because their “numbers are normal.” Other times, they’re given the wrong meds, or not enough of the right ones.
While I often talk about various healing modalities that we can use to take back our health, thyroid hormone medications are also often a critical part of the healing journey for many of us with Hashimoto’s. I want to make sure you are aware of the options you have and educated about the options that may work best for you, so that you can advocate for your best care.
Medications were the first healing modality that I was trained in, and before I learned about nutrients, gut health, adrenals and various complementary, integrative and functional medicine therapies, my area of specialty and passion focused on the appropriate use of medications. In 2010, I was one of the first pharmacists in the United States to become certified in Medication Therapy Management (MTM). I took a red-eye from California, where I lived at the time, to get to an early morning MTM certification training in Washington, DC, at a meeting of the American Pharmacists Association. As the training was so new, it was not available in other states at the time. In my career as a consultant pharmacist, I performed comprehensive medication reviews for thousands of people, many of whom had very complex medical histories that included disabilities, mental health issues, multiple diagnoses, and multiple medications.
I focused on ensuring that the person had the best possible medication-related outcomes. I looked for potential side effects, medication errors, drug interactions, and adverse reactions. I also looked to see that each person was treated appropriately and received the right medication at the right time. Time and time again, I saw one common error in medication use in just about every client. This error was so common, that I ended up creating a short-code for it in my reports, as I was tired of typing it up time and time again. The error was with how thyroid medications were taken. Most thyroid medications need to be taken apart from food, coffee, and other medications, due to the fact that such substances can prevent medications from being properly absorbed. This can lead to a fluctuation of thyroid hormones, and thus, a re-emergence of thyroid symptoms… yet just about everyone I saw was taking their thyroid medications with food, coffee, and/or other medications!
I always say that optimizing a person’s thyroid medication is both an art and a science: so many factors can impact your medication’s effectiveness. As you may know, I recommend finding a trusted functional practitioner who is able to titrate and prescribe the perfect dose and formulation (T4, T3, or a combination of both) for your particular thyroid health status. Ideally, your practitioner has also made you aware that certain factors, such as having acid reflux, food sensitivities, or digestive issues, or taking your medications with your morning cup of coffee, can potentially sabotage your medication’s effectiveness.
The inactive ingredients (fillers) within your given hormone medication also need to be considered, as those can sometimes impact how your body will respond to your medication, and many of my clients experience sensitivities to the many fillers found in their T4 medications. These have also been shown to affect the absorption rate and effectiveness of the very medication meant to help the thyroid!
This is what happened to Debra Shultz, who had been taking Levoxyl for a few years before suddenly developing a variety of wide-reaching symptoms (including a stiff neck, fibromyalgia pain, breathlessness, flushing, fatigue, stomach aches, and more). She eventually learned that Levoxyl’s manufacturer had changed the formulation for the popular medication, adding a rapid disintegrant (which helps make the tablet dissolve quickly with water), causing Debra the negative reaction and symptoms. After that, Debra and her doctor were left tinkering with every conceivable brand and dosage – for almost a decade – to try and alleviate the symptoms brought on by this seemingly insignificant ingredient change.
But, everything she tried triggered her immune system to react. Debra needed a hypo-allergenic version of levothyroxine.
Fortunately, around that same timeframe, she found liquid Tirosint®. This medication is a gel cap (not a tablet) that contains only three hypoallergenic ingredients in addition to levothyroxine; gelatin, glycerin and water. Her body started to more consistently absorb the thyroid hormones from the medication. After taking the Tirosint gel caps, she felt well again, had more physical and mental energy, and shed the symptoms she had been experiencing.
This is why I was SO excited to learn that the liquid version of levothyroxine, Tirosint-SOL, finally became available in the United States recently. I had this medication on my radar for quite some time, as it had shown a lot of benefits in Europe over the last few years — but I delayed writing about it, as most of my readers are based in the United States. In addition to Tirosint-SOL, the hypoallergenic capsule version of Tirosint has been a favorite T4-thyroid medication used by many of my clients and readers.
Tirosint-SOL and Tirosint are potential options that may be better absorbed (leading to fewer thyroid symptoms) for people who have certain gastrointestinal challenges, who are taking antacids/acid blockers/PPIs, or who are otherwise experiencing low stomach acid.
Tirosint can also be better absorbed with your morning cup of coffee, compared to other T4 meds! I was so excited when the research came out supporting this.
While Tirosint, just as any thyroid hormone replacement medication, isn’t right for everyone, it may be a helpful option for some, especially those on conventional T4 medication that may just not be working optimally.
In today’s article, you’ll learn:
- How Tirosint is different
- Who might benefit from taking Tirosint
- The feedback on Tirosint
- Details on availability and cost
- Where to start (and how to talk to your doctor about Tirosint)
Do You Take a T4 Medication?
The standard of care for hypothyroidism and Hashimoto’s is to utilize a synthetic thyroid hormone replacement medication identical to the T4 hormone (levothyroxine) produced by the body’s thyroid gland.
Most conventional doctors will prescribe levothyroxine to their patients (either generic or brand name versions); a few of the brand names (all available in tablet form) include Synthroid®, Levoxyl®, Eltroxin® (in Canada), Euthyrox® (in the EU), and Oroxine® or Eutroxsig® (in Australia).
While this article focuses on things that can sabotage the effectiveness of different T4 medications, it’s worth noting that some people may just never feel their best taking only T4 medication.
Some may do better on T3-containing medications (Cytomel and compounded T3) or combination T4/T3 medications (Nature-Throid, Armour, WP Thyroid, compounded T4/T3 medications). This will often depend on a person’s ability to properly convert levothyroxine (T4) to liothyronine (T3), the more metabolically active thyroid hormone. You can learn more about options beyond T4 medications here.
While most T4 medication comes in tablet form, Tirosint is a newer T4 medication that is available in gel caps. As of last year, a brand new liquid formulation, Tirosint-SOL, became available in the U.S. This liquid solution containing just three hypoallergenic ingredients (levothyroxine, glycerol, and water), is sold in single-dose ampules.
So how are these newer T4 medications different, and how do you know which T4 medication might be the best for you?
How Tirosint is Different
All T4 medications have the same active ingredient, levothyroxine, and different brands have varying packaged dosages that can be prescribed. There are also compounding pharmacies that can provide more of a customized dose.
Many people do very well on T4-containing medications once they are dosed appropriately and become stabilized on them. Also important to how well the medication works is how consistently it is absorbed, and whether its ingredients may cause a reaction for any given person.
T4 medications may differ in:
- The inactive ingredients they contain.
- The consistency of their absorption.
- How well they support people’s ability to consistently take them as indicated.
Let’s talk about these and how Tirosint in particular is different.
1. Can you tolerate the inactive ingredients found in your T4 medication?
If you were to check the ingredient information listed for most T4 medications, you’d find a number of inactive ingredients. These may be used as bulking agents to stabilize the tablets, as preservatives, as coloring agents, or as an aid in manufacturing in some way.
Disintegrants (some examples being starches and cellulose) are added to help promote the breakup of the tablet into smaller pieces when the tablet hits an aqueous environment (such as when you drink water with your meds, or when your meds touch the saliva in your mouth). This promotes a more rapid release of the medication. (Remember, it was the addition of a disintegrant that initially seemed to cause symptoms for Debra.)
Synthroid, for example, may cause people (especially those with dairy sensitivities, lactose intolerance or lactose allergies) absorption challenges, given that the medication’s fillers include lactose. Synthroid also contains other inactive ingredients which may trigger a negative response, including corn starch, confectioners’ sugar, magnesium stearate, talc, povidone and color additives.
As another example, Levoxyl contains five inactive ingredients including an anti-caking agent, a filler, a rapid disintegrant, an antacid, and a flow agent (along with two dyes made from coal tar). Any one of these can cause a sensitive individual an adverse reaction.
Here’s a list of some of the inactive ingredients (also referred to as excipients) that you might find in your T4 medication:
- Lactose monohydrate
- Modified wheat starch (gluten)
- Confectioners’ sugar (may contain corn starch)
- Dyes
- Sucrose
- Talc
- Microcrystalline cellulose
- And many more…
While these ingredients are only present in small amounts within thyroid medication and are well tolerated by some individuals, others may have adverse reactions to them. We know that sensitivities in general are more common in people with autoimmunity, and while gluten is the most common reaction in those with Hashimoto’s, an individual can be reactive to just about anything, so the fewer filler ingredients are present in our medications, the less likely we are to react, and the more likely we are to absorb them. Additionally, some fillers are more reactive than others.
In one of the most comprehensive surveys ever conducted amongst hypothyroid patients, the CONTROL Surveillance Project (2012) found that 15.2 percent of the 925 respondents receiving levothyroxine, reported allergies to the inactive ingredients found in their tablet drug formulations. The most frequently reported allergies were to lactose (11.9 percent), gluten (3.78 percent), and sucrose or food dyes (1-2 percent each). (1)
Lactose and gluten are very common sensitivities found in many people with Hashimoto’s. Other common ingredients that can cause problems include grains (especially corn), eggs and soy. For people with sensitivities, even the smallest amount of a given ingredient found in their medication, such as the lactose in Synthroid, can cause a reaction. (A few years ago, in my own clinical practice, I also found that Synthroid may be cross-reactive with gluten as well. I actually started a petition to remove gluten containing ingredients from Synthroid and called Abbvie, the maker, to request this back in 2016!)
To address these issues, I have recommended Tirosint to many of my clients. Tirosint contains the fewest inactive ingredients, as it does not contain any gluten or lactose.
Tirosint comes in two forms: gel caps and liquid single-dose ampules.
Tirosint gel caps: These levothyroxine sodium gelatin capsules that contain T4 dissolved in gelatin, glycerin and water, came on the market in the United States in 2017. The gel caps are free of inactive filler ingredients such as gluten, lactose, dyes, and preservatives that might cause tolerability or absorption issues.
Tirosint gel caps initially worked well for Debra and reduced her symptoms, but due to her longstanding history of intestinal permeability, she became sensitive to the gelatin in Tirosint’s gel caps, which was derived from bovine and porcine sources. She wondered if she could have developed a beef and pork allergy, as she knew her system was prone to developing food sensitivities.
She felt she needed something even more hypoallergenic than the gel caps. That’s when she found that the manufacturer of Tirosint had brought a new liquid version of Tirosint to the US market (in 2019), that did not contain any gelatin. This liquid version had already been studied and utilized in Europe with the backing of several published studies, showing it to be very hypoallergenic as well as providing “barrier-free” medication absorption (to allow faster and consistent effectiveness).
Tirosint-SOL liquid ampules: Debra was happy to find that the liquid version of Tirosint was free of gelatin. Tirosint-SOL is available in liquid single-dose ampules and only contains two inactive ingredients (glycerol and water).
While Debra loves the ease and effectiveness of Tirosint-SOL, she continues to make tweaks to best optimize her absorption of the medication. Like many of my clients, she has found that there are other things that can affect her medication’s consistent absorption and effectiveness, including underlying health conditions, as well as other prescriptions, OTC medications, supplements, and even the intake of some foods.
2. Is your T4 medication being consistently absorbed?
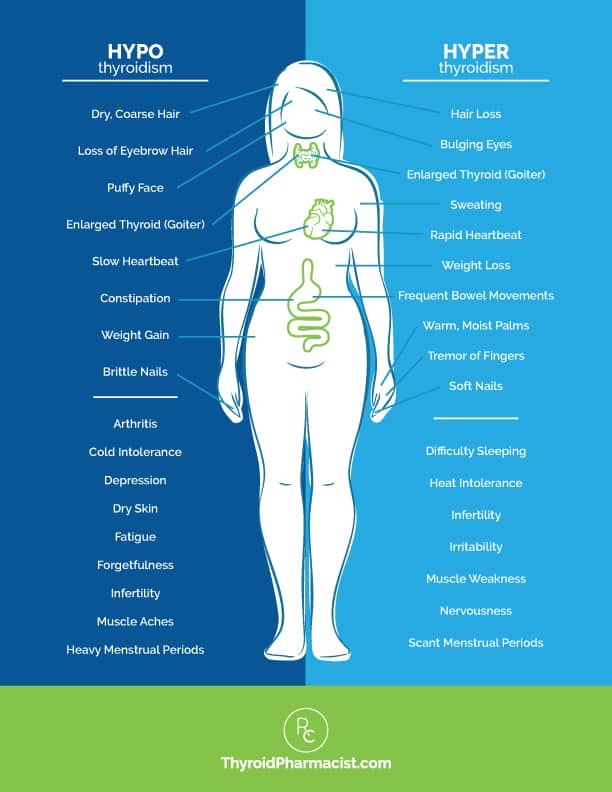
Because thyroid medication has a narrow therapeutic index (they are referred to as “Goldilocks” medications, as they have to be dosed “just right” to be effective and to prevent adverse effects), if the absorption is inconsistent, you can sometimes get a bit too much or a bit too little. This can cause fluctuations between hyperthyroidism and hypothyroidism symptoms.
Several studies consisting of patients receiving levothyroxine therapy, have shown that a large percentage of patients (some 40-48 percent) are over- or undertreated. One 2014 study found that, even with frequent dose adjustments and monitoring, 37 percent of people taking levothyroxine often still had TSH levels outside of the normal reference range. This is often a result of inconsistent absorption.
Why is consistent thyroid medication absorption so important?
Fluctuating thyroid hormone levels can cause a person to swing back and forth between hyper- and hypothyroid symptoms, and these changes can be triggered simply by combining medication with the wrong food or drink, or underlying digestive issues.
Symptoms seen in overmedication (resulting in symptoms often seen in hyperthyroidism) can include:
- Weight loss
- Palpitations
- Anxiety
- Eye bulging
- Tremors
- Irritability
- Infrequent menstrual periods
- Fatigue
- Heat intolerance
- Increased appetite
- Hair loss
- Enlarged thyroid gland
- Sweating
- Frequent bowel movements
- Infertility
- Soft nails
- Warm, moist palms
- Finger tremors
- Insomnia
- Muscle weakness
- Nervousness
Symptoms associated with under-medication (resulting in symptoms associated with hypothyroidism) can include:
- Slower metabolism leading to weight gain
- Forgetfulness
- Feeling cold or cold intolerance
- Depression
- Fatigue
- Dry skin
- Constipation
- Loss of ambition
- Dry, coarse hair
- Muscle cramps
- Stiffness
- Joint pain
- A loss of the outer third eyebrow
- Heavy menstrual periods
- Infertility
- Muscle aches
- Puffy face
- Slow heartbeat
- Brittle nails
- Arthritis
As discussed above, inactive ingredients in T4 medication can cause tolerability or allergic reactions in some people, triggering gut issues and inconsistent absorption of thyroid medication.
Inconsistent absorption can also be compounded by:
- Active and inactive ingredients found in other prescription medications. During pharmacy school, we spent a lot of time learning about drug interactions. Quiz time… do you know which medication was notorious for interacting with just about everything? If you guessed thyroid medication, you are correct! Thyroid hormones interact not only with other medications, but also with some supplements and even fillers found in medications. There can be an additive effect caused by adding up all of the inactive ingredients in a number of the medications a person might take. This is especially true for older people taking multiple medications. A study by MIT researchers found that 93 percent of medications contain inactive ingredients with the potential to cause an adverse reaction.
- OTC medications for GERD/acid reflux, gastritis and heartburn. Antacids and proton pump inhibitors (PPIs such as Pepcid, Prilosec, Protonix, Nexium, Omeprazole, Zantac, Tagamet, Maalox and Rolaids, to name a few) can impede the dissolution (breaking apart) of T4 tablets, as gastric acidity is required to break down the tablet. Traditional T4 tablet formulations require you to have at least four hours of time between taking your thyroid medications and these types of medications. I have found that many people with Hashimoto’s who have acid reflux symptoms (and may be taking PPIs) actually have low stomach acid, which may already be affecting their absorption of thyroid medication (this condition also primes the gut for other issues such as infections, which can even further impact medication absorption).
- Ingredients found in supplements. Calcium and iron supplements in particular can affect the absorption of levothyroxine (especially when taken less than four hours apart). Yet, 51.8 percent of respondents in the CONTROL Surveillance Project Switch Study said they frequently took these types of supplements.
- Consuming foods/beverages known to cause malabsorption of levothyroxine. This includes foods high in iodine (plain yogurt, lobster, dried seaweed, cod, and cranberries), soy-based foods, or high-fiber foods (broccoli, fiber drinks, fiber bars, bran flakes). In a recent survey of over 31,000 patients, only 33.4 percent reported telling their conventional practitioner about their diet and nutritional supplement use relating to potential interaction with their thyroid medication.
- Taking levothyroxine with coffee and/or breakfast or later in the day. Many people aren’t aware that taking their current thyroid medication with coffee and/or breakfast in the morning may be sabotaging its effectiveness. (Tablet formulations are supposed to be taken 30 minutes to an hour before breakfast or coffee.) However, 20 percent of respondents in the CONTROL Switch Study indicated that they took their medication with coffee, breakfast or another meal, versus following the directions to fast while taking their medication. Studies have shown that intestinal absorption of T4 tablets is reduced when taken with food and/or coffee. One study found that eating while taking one’s T4 tablet medication reduced absorption from approximately 80 to 40 percent, and is associated with higher serum TSH concentrations.
- Having other underlying health conditions (in particular those relating to gastrointestinal health or food allergies). Thyroid hormones are absorbed in the small intestine, and absorption is dependent on gastric acidity levels. Conditions like untreated celiac disease lactose intolerance and infections (H. pylori, small intestinal bacterial overgrowth, or SIBO) in the small intestine, may prevent proper thyroid hormone absorption. In one study, of the 13.4 percent of patients who reported difficulty controlling their hypothyroid symptoms, significantly more patients with comorbid gastrointestinal (GI) conditions reported such difficulty, and were nearly twice as likely to need a change in thyroid medication dosage compared to those without GI conditions. (These dosage changes were likely due to their GI conditions affecting the absorption of their medication.) Food sensitivities are also factors that can affect the GI system’s ability to absorb thyroid medication. While most people with Hashimoto’s will have a sensitivity to gluten and dairy, up to 15 percent are diagnosed with celiac disease, and 76 percent as lactose intolerant! Additionally, 80 percent of the clients I have tested have been positive for one or more gut infections.
Many people are not even aware that these factors can affect their levothyroxine therapy. The CONTROL Surveillance Project found that few of the 925 respondents (only around 10 percent) ever discussed any of these potential impacts with their doctor.
While some of these issues are unrelated to the particular T4 medication you are taking (and require other interventions such as removing offending foods or supplements), several can actually be mitigated by using one or both forms of Tirosint.
Tirosint is different and may help with:
- Minimizing additive effects across multiple medications that cause food allergies and reactions to inactive ingredients, given that both forms of Tirosint contain the fewest inactive ingredients, and no gluten or lactose.
- Minimizing the effects relating to a person taking medications such as PPIs for GERD/acid reflux. Tirosint is more stable due to the way it’s encapsulated, compared to thyroid medications available in tablet form, and can be better absorbed alongside PPIs. In studies, gel caps and liquid formulations showed a dissolution pattern, which resulted in more consistent absorption and bioavailability, and was minimally affected by changes in gastric acidity caused by taking PPIs/antacids or having low stomach acid (due to inflammation or infection). Patients with these forms of altered stomach acid secretion taking tablet formulations, needed a higher dose than those with normal acid secretion. In another study, patients with impaired gastric acid secretion were able to achieve similar TSH levels as they did with tablet formulations, despite having a 17 percent lower dose with the gel cap.
- Removing the morning coffee concern! While Tirosint’s package insert recommends spacing your coffee a few hours away from your thyroid meds, I believe it is more of a precaution for all medications of that class. (In fact, in pharmacy school, the answer to “Which of these medications may interact with XYZ?” was most often “thyroid medications”!) Further studies have shown that Tirosint is better absorbed with coffee compared to other forms of T4. In fact, new research has found that gel caps and liquid forms are unaffected when taken with coffee (unlike tablet formulations).
- Possibly removing the restriction of taking medication with breakfast in some people. While more research is needed, there have been a few studies focused on taking Tirosint with breakfast. One 2016 study concluded that both gel cap and liquid forms could be taken with breakfast, but the absorption of the gel cap form eroded over time while using the prescription. Researchers concluded that, for certain people (i.e. those who need to avoid even small changes in T4 and T3 levels), the liquid form would be preferred at breakfast. (25) Another study done in 2018 found that ingestion of the liquid form taken with breakfast did not affect thyroid function in the majority of patients. However, 12 percent of patients did have an increase in serum TSH levels, and while researchers weren’t sure why, noncompliance could have been to blame. Studies have shown that ingesting food with tablet T4 medication decreases its absorption from approximately 80 to 40 percent. Additionally, taking the medication within 20 minutes of breakfast, instead of 60 minutes before breakfast, resulted in a TSH increase of about 2.4 times. The dissolution of the tablets themselves is delayed when the gastric pH is increased, and food may delay this process both by a direct effect and/or by increasing the gastric pH. Therefore, Tirosint liquid, which does not need to dissolve, will be more quickly absorbed, even in the presence of food.
- Providing more effective treatment for people with co-occurring gastrointestinal and digestive conditions such as lactose intolerance, H. pylori infections, celiac disease, malabsorption issues, and other gastric pH-related issues. (28) In various studies, including the CONTROL Switch study, patients who switched from tablets to gel caps found they needed to take less thyroid medication, while also gaining significant improvements in symptom control. The gel cap formulation was shown to be consistently absorbed in the presence of factors that commonly affect the consistent absorption of levothyroxine tablets, such as patients with other health issues that alter gastric acidity and interfere with absorption.
3. Does your medication promote easy adherence?
Improved adherence is all about making taking medication easy! If taking medications is unpleasant, disrupts routines, or has too many unwanted side effects, people will be much less likely to stick with their routines. Based on existing research, Tirosint may help with this in a number of ways:
- Can be easier to swallow (than intact tablets)
- Can be better absorbed when taken with coffee
- Can be taken with breakfast (studies show the liquid form can be used by most people)
- Can be better absorbed alongside many other medications (such as antacids and PPIs) compared to tablet forms of T4
Of course, other adherence issues, such as those related to the consumption of specific foods (high iodine or high fiber foods) and supplements (calcium and iron), still need to be addressed with other interventions, regardless of T4 medication.
Who Might Benefit From Taking Tirosint?
There is a subset of people who find their hypothyroidism (thyroid hormone levels or symptoms) difficult to control. We know that tweaking dosages, especially going too high on levothyroxine, occurs a lot. (Studies show this happens to 14 to 22 percent of patients and can be associated with bone loss, adverse cardiovascular events and hyperthyroid symptoms!) It can also make people feel like they just can’t get better.
I find that many of my clients and readers whose TSH levels continue to fluctuate, have food sensitivities, are lactose intolerant, may be taking PPIs or have stomach acid problems, or may have other underlying conditions causing poor absorption of their medication (such as gastrointestinal infections or underlying diseases such as irritable bowel syndrome). If this sounds like you, Tirosint might be worth discussing with your doctor as an option to try.
Community Feedback on Tirosint
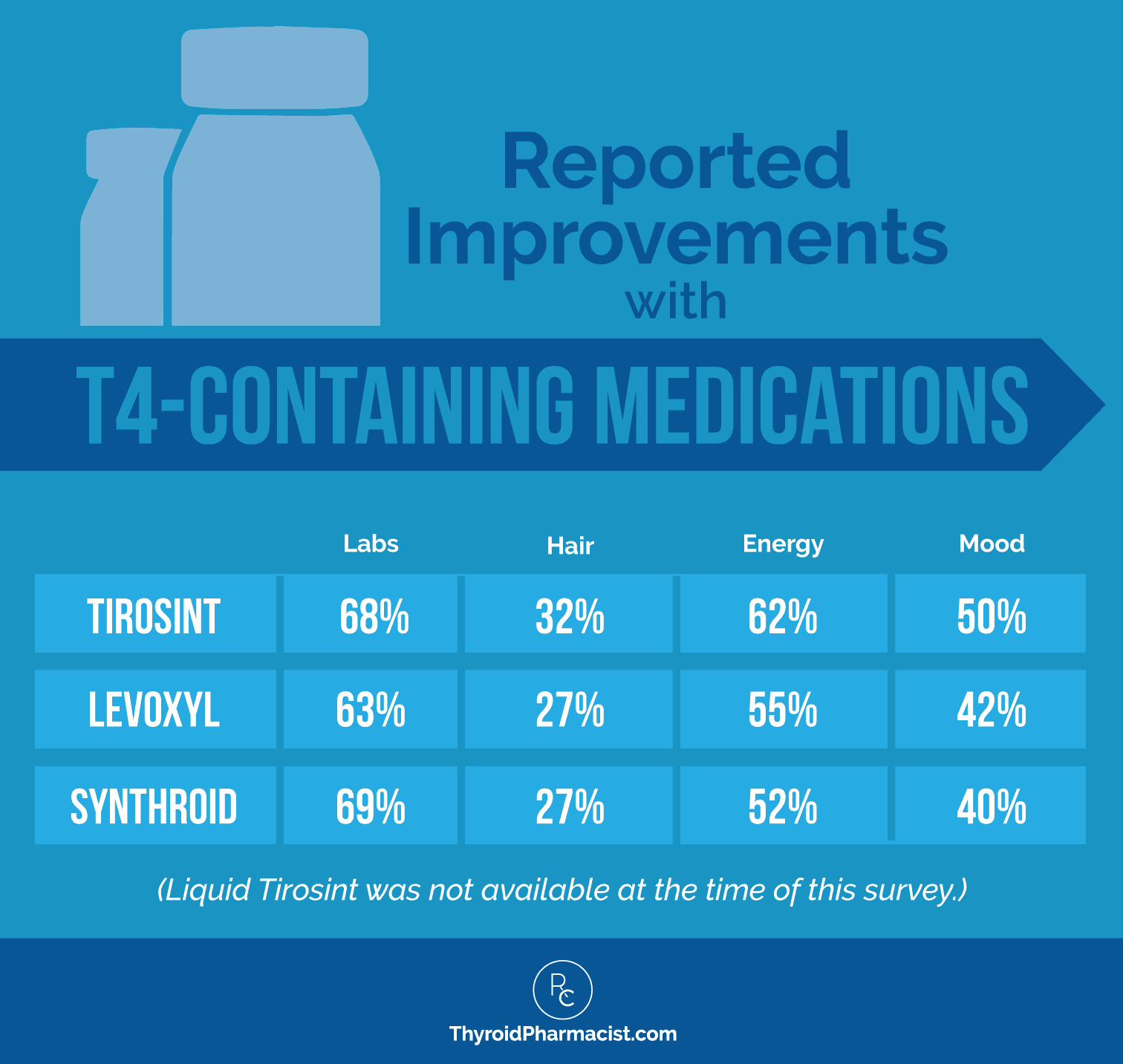
Many in my community have shared with me that they have felt better after switching to Tirosint. In a 2015 survey I did of over 2,000 readers, those that switched to Tirosint (gel caps) experienced a 68 percent improvement in their labs, a 32 percent improvement in hair loss, a 62 percent improvement in energy levels, and a 50 percent improvement in mood.
I personally believe that the ability of this formulation to be absorbed consistently, with limited fluctuations, contributes to the benefits seen in hair appearance, energy levels, and mood — some of the most subtle symptoms that can be especially sensitive to levels that are outside of the ideal range. For me personally, I can tell that my thyroid hormone levels are off when my hair becomes more difficult to brush! And of course, when I had unstable thyroid hormone levels, my mood and energy were also unstable!
Here’s how the reported improvements with Tirosint compare with improvements seen using other T4-containing medications:
I also had a positive experience using Tirosint during my pregnancy. Pregnant women typically need about a 30 percent higher dose of their thyroid medication early on in their pregnancy. Although I usually take a combination T4/T3 medication, my T3 was in great range, while my T4 needed a boost. I ended up choosing Tirosint, as it is lactose-free and I knew I would have the best chance of adequate absorption, at a time when this was important not just for my symptoms, but potentially for the survival of my baby as well. I also thought at the time that I had a little case of SIBO (I never did test — it could have just been bloat from my pregnant belly, lol), so I knew that Tirosint was the best option. I also liked that it came in a little pill planner with days of the week, much like birth control pills, so it was easy to remember to take even with my “pregnancy” brain.
The research supports positive results with both forms of Tirosint; they are shown to be well absorbed in the presence of multiple factors that limit the consistent absorption of other levothyroxine tablets. Patients switching from tablets to gel caps were found to have improvements in symptoms, and they were able to significantly reduce their dose. The CONTROL Switch Study found that almost 62 percent of patients who switched from T4 tablets to Tirosint, experienced improvement in their hypothyroid symptoms.
Finally, as Tirosint is a T4-only medication, this is an option that conventionally-trained physicians and endocrinologists might be more open to, compared to T3-containing medications. Doctors who have been in practice for quite some time and are not integrative-minded, might still be resistant to the use of natural desiccated thyroid medication (NDT), as they remember the problems associated with the inconsistent product in its early years, before the process was improved to ensure accurate dosing. I know so many of my readers have issues with asking their endocrinologists to prescribe T3-containing medications, and most endocrinologists are not comfortable in doing so, but they may be comfortable in prescribing Tirosint, as it’s a T4 option.
My colleague Dr. Christine Maren, a functional medicine physician who specializes in thyroid health, says:
“While I’m a big fan of natural desiccated thyroid (NDT), I’ll use synthetic T4 in certain patients.
Tirosint is my synthetic T4 of choice because it’s clean and has very few fillers. I’ll especially recommend this for people with a lot of food sensitivities/allergies, or for people who have severe gastrointestinal symptoms or malabsorption issues, since the Tirosint solution is an effective option.
There are four main instances when I prescribe Tirosint:
- Some patients do not tolerate (or need) the T3 component of NDT, so a synthetic T4 is a better fit. These patients typically do not have a conversion issue between T4 and T3.
- Some patients do better on synthetics than NDTs, and I will often prescribe Tirosint with a synthetic T3 medication (Liothironine or Cytomel).
- People on NDTs sometimes need a little additional T4, so I will add a small dose of Tirosint to an NDT to get the right ratios of T4 and T3.
- I have several patients that are very sensitive to tiny dosage adjustments in their thyroid medication, with widely fluctuating TSH. In these patients, I’ll use the Tirosint solution to bypass issues with absorption. This has helped to even out the wide swings in thyroid labs.”
How to Get Started with Tirosint
Product Availability
- Tirosint gel caps are available in 12 different dosage strengths ranging from a 13 mcg dose to a 200 mcg dose. You can find the full Tirosint package insert, ingredients list, precautions, drug interactions, and other information at https://www.accessdata.fda.gov/drugsatfda_docs/label/2007/022121lbl.pdf.
- Tirosint-SOL is available in single-dose liquid ampules. There are 12 dosage strengths for your doctor to choose from. Find the Tirosint-SOL package insert, ingredients, precautions, drug interactions and other information at https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/206977s000lbl.pdf.
Possible adverse effects: As with other T4 medications, adverse effects are those of hyperthyroidism due to therapeutic over-dosage. These include irritability, nervousness, weight loss, increased appetite, arrhythmias, myocardial infarction, menstrual irregularities, muscle spasms, dyspnea, insomnia, headache, tremors, muscle weakness, diarrhea, heat intolerance, and skin rashes.
Drawbacks
One of the challenges with new medications is that they often cost more than generic counterparts, even if they are more effective. Insurance companies may charge higher copays or not cover newer, branded medications for some people. Some may also require that a reason has a prior authorization from their prescriber, detailing why they need this specific medication, such as having failed the generic versions. As a retail pharmacist, I was often helping patients navigate medication costs, and oftentimes found that pharmaceutical manufacturers would set up special patient assistance programs in these cases, to help with costs.
Programs Currently Available to Help with Medication Costs
Tirosint is marketed and distributed by IBSA Pharma Inc. IBSA offers several programs to provide patients with cost-effective access.
Tirosint/Tirosint-SOL Copay Savings Card
For patients with commercial health insurance who want to get their prescription at a retail pharmacy, the Tirosint Copay Savings Card (or Tirosint-SOL Copay Savings Card) may be the best option. Eligible patients may pay as little as $25 per prescription, with a savings of up to $85 per fill. Find out more and download your copay savings card.
Tirosint/Tirosint-SOL Direct Program
For patients with high copays/deductibles or without insurance, the Tirosint Direct Program (Tirosint-SOL Direct Program) is available through participating mail order pharmacies and offers the lowest cash price available.
IBSA Patient Assistance Program
IBSA offers a patient assistance program to individuals who meet eligibility requirements. Eligibility is based on your annual household income and prescription insurance status. For more information on eligibility and how to enroll, visit www.ibsapap.com.
Another challenge with new medications is that pharmacies may not keep them in stock, and thus, a person may have a difficult time in getting their prescription filled. Some of my clients have dropped off prescriptions for Tirosint, only to find out that the pharmacy called the doctor to switch to a medication that was in stock instead! You can be proactive in preventing this by getting in touch with your pharmacy and asking the team if they have Tirosint in stock, or by asking them to order Tirosint specifically when dropping off your prescription.
The Takeaway
Tirosint isn’t for everyone, as no thyroid medication is one-size-fits-all.
But, if you are finding that your current T4 prescription…
- Isn’t resulting in a reduction in symptoms or improvement in labs
- Is resulting in new symptoms related to possible ingredient reactions (nausea, bloating, diarrhea, headaches, upset stomach or rashes), or
- Is requiring ongoing dosage tweaking to meet your TSH and antibody goals (and you’re still not feeling well)
…you might want to talk to your doctor about Tirosint.
If you are just starting out with thyroid hormone therapy, review the “Who Might Benefit From Tirosint” section in this article. Do any of these sound like you? If so, I encourage you to print out this article and bring it to your doctor. (Tirosint’s manufacturer also provides some online patient tools that can help when talking with your doctor. You can find them here.)
While you are at it, complete a health history timeline as well. This is a helpful tool for identifying your medical and dental health history. It also focuses on what was going on in your life the last time you remember feeling well. Spending some time upfront to create your own health timeline, can help you and your doctor identify potential triggers (including lactose intolerance, GERD or low stomach acid, viruses, etc.) of your thyroid condition. This can help identify the best thyroid hormone medication for you as well.
Enter your email below to download a Free Health Timeline!
Before discussing starting thyroid hormone replacement therapy with your doctor, you might benefit from reading this article, “11 Things to Know About Thyroid Medications.” Remember, finding the perfect medication for you is part art and part science, with many aspects to obtaining what will work best for you. Don’t get frustrated or discouraged!
Utilize the cost savings info referenced above, as well as the manufacturer’s customer service line 800-587-3513 or email medinfo@ibsapharma.com, to answer other questions you might have. Tell your doctor he/she can get free samples of Tirosint and Tirosint-SOL from IBSA Pharma, via their website, to try as well.
Finally, remember that some people will just not do well on a T4-only medication. To learn a bit more about why that is so, read this earlier article on how to find the best thyroid medication for you.
Please keep me posted on your progress by joining my community on Facebook. I’d love to know how you do if you try Tirosint. Sharing your journey helps others who might be wondering if it might be a viable option for them as well.
As always, I wish you well on your journey to better health!
P.S. Be sure to sign up for my weekly newsletter to get a free book chapter, recipes, the Thyroid Diet Starter Guide, and notifications about upcoming events and my latest research!
References
- McMillan M, Rotenberg KS, Vora K, et al. Comorbidities, concomitant medications, and diet as factors affecting levothyroxine therapy: results of the CONTROL surveillance project. Drugs R D. 2016;16(1):53–68.
- Cappelli C, Castello R, Marini F, et al. Adherence to levothyroxine treatment among patients with hypothyroidism: a northeastern Italian survey. Front Endocrinol (Lausanne). 2018;9:699.
- Brancato D, Scorsone A, Saura G, et al. Comparison of TSH Levels with liquid formulation versus tablet formulations of levothyroxine in the treatment of adult hypothyroidism. Endocr Pract. 2014 Jul;20(7):657-62.
- Reker, D. Blum, S. Steiger, C. et al. Inactive ingredients in oral medications. Science Translational Medicine. 2019 Mar13: Vol. 11, Issue 483.
- In-pharmatechnologist.com, “Researchers call on manufacturers to provide excipient allergy info”.HTTPS://WWW.IN-PHARMATECHNOLOGIST.COM/ARTICLE/2019/03/18/EXCIPIENTS-AND-THE-RISK-OF-ALLERGIC-REACTIONS. Updated 3/18/2019. Accessed March 21, 2020.
- Centanni M, Gargano L, Canettieri G, et al. Thyroxine in goiter, helicobacter pylori infection, and chronic gastritis. N Engl J Med. 2006 Apr 27;354(17):1787-95.
- McMillan M, Rotenberg KS, Vora K, et al. Comorbidities, concomitant medications, and diet as factors affecting levothyroxine therapy: results of the CONTROL surveillance project. Drugs R D. 2016;16(1):53–68.
- Tirosintsol.com. “Talk to your doctor.” https://tirosintsol.com/getting-started/talk-to-your-doctor/. Accessed March 29, 2020.
- Centanni M. Thyroxine treatment: absorption, malabsorption, and novel therapeutic approaches. Endocrine. 2013;43(1):8–9.
- Benvenga S., Bartolone L., Squadrito S., et al. Delayed intestinal absorption of levothyroxine. Thyroid. 1995;5(4):249–253.
- Bach-Huynh TG, Nayak B, Loh J, et al. Timing of levothyroxine administration affects serum thyrotropin concentration. J Clin Endocrinol Metab. 2009;94(10):3905–3912.
- Centanni, M. The New England Journal of Medicine, April 27, 2006; vol 354: pp 1787-1795.
- Vita R, Fallahi P, Antonelli A, et al. The administration of L-thyroxine as soft gel capsule or liquid solution. Expert Opin Drug Deliv. 2014 Jul;11(7):1103-11.
- Pabla D, Akhlaghi F, Zia H. A comparative pH-dissolution profile study of selected commercial levothyroxine products using inductively coupled plasma mass spectrometry. Eur J Pharm Biopharm. 2009 May;72(1):105-10.
- Santaguida M. G., Virili C., Duca S. C. D., et al. Thyroxine softgel capsule in patients with gastric-related T4 malabsorption. Endocrine. 2015;49(1):51–57.
- Vita R., Saraceno G., Trimarchi F., et al. A novel formulation of l-thyroxine (l-T4) reduces the problem of l-T4 malabsorption by coffee observed with traditional tablet formulations. Endocrine. 2013;43(1):154–160.
- Cappelli C, Pirola I, Gandossi E, et al. Oral liquid levothyroxine treatment at breakfast: a mistake? Eur J Endocrinol. 2013 Nov 22;170(1):95-9.
- Vita R., Saraceno G., Trimarchi F., et al. A novel formulation of l-thyroxine (l-T4) reduces the problem of l-T4 malabsorption by coffee observed with traditional tablet formulations. Endocrine. 2013;43:154–160.
- Cappelli C, Pirola I, Daffini L, et al. A double-blind placebo-controlled trial of liquid thyroxine ingested at breakfast: results of the TICO study. Thyroid (2016) 26:197–202. 10.1089/thy.2015.0422
- Pirola I, Gandossi E, Brancato D, et al. TSH evaluation in hypothyroid patients assuming liquid levothyroxine at breakfast or 30 min before breakfast. J Endocrinol Invest. (2018) 41:1301–6. 10.1007/s40618-018-0867-3
- Benvenga S., Ducharme M.P. Comparison of the intestinal absorption of levothyroxine (LT4): Tablet vs. soft gel capsule formulation. Endocr. Rev. 2011;32:3–625. doi: 10.1210/er.2009-0043.
- Vita R., Saraceno G., Trimarchi F., et al. A novel formulation of l-thyroxine (l-T4) reduces the problem of l-T4 malabsorption by coffee observed with traditional tablet formulations. Endocrine. 2013;43:154–160. doi: 10.1007/s12020-012-9772-2.
- Saraceno G., Vita R., Trimarchi F., et al. Two novel formulations of l-T4 (oral solution and soft gel capsule) are refractory to the coffee-induced intestinal malabsorption of tablet l-T4. Eur. Thyroid J. 2013;2:P132–P145.
- Virili C, Giovanella L, Fallahi P, et al. Levothyroxine therapy: changes of TSH Levels by switching patients from tablet to liquid formulation. A systematic Review and meta-analysis. Front Endocrinol (Lausanne). 2018;9:10. Published 2018 Jan 26.
- Cappelli C, Pirola I, Gandossi E, et al. Thyroid hormone profile in patients ingesting soft gel capsule or liquid levothyroxine formulations with breakfast. Int J Endocrinol. 2016;2016:9043450.
- Guglielmi R, Grimaldi F, Negro R, et al. Shift from levothyroxine tablets to Llquid formulation at breakfast improves Qqality of life of hypothyroid patients. Endocr Metab Immune Disord Drug Targets. 2018;18(3):235-240.
- Cappelli C, Pirola I, Gandossi E, et al. Thyroid hormone profile in patients ingesting soft gel capsule or liquid levothyroxine formulations with breakfast. Int J Endocrinol. 2016;2016:9043450.
- Fallahi P, Ferrari SM, Ruffilli I, et al. Advancements in the treatment of hypothyroidism with L-T4 liquid formulation or soft gel capsule: an update. Expert Opin Drug Deliv. 2017 May;14(5):647-655.
- Ernst FR, Sandulli W, Elmor R, et al. Retrospective study of patients switched from tablet formulations to a gel cap formulation of levothyroxine: results of the CONTROL Switch Study. Drugs R D. 2017;17(1):103–115.
- Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III) J Clin Endocrinol Metab. 2002;87:489–499.
- Ernst FR, Sandulli W, Elmor R, et al. Retrospective study of patients switched from tablet formulations to a gel cap formulation of levothyroxine: results of the CONTROL Switch Study. Drugs R D. 2017;17(1):103–115.
- Ernst FR, Sandulli W, Elmor R, et al. Retrospective study of patients switched from tablet formulations to a gel cap formulation of levothyroxine: results of the CONTROL Switch Study. Drugs R D. 2017;17(1):103–115.
- Brancato D, Scorsone A, Saura G, Ferrara L, Noto A, Aiello V, et all. Comparison of TSH Levels with Liquid Formulation Versus Tablet Formulations of Levothyroxine in the Treatment of Adult Hypothyroidism. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 20. 1-17. 10.4158/EP13418.OR.
- McMillan M, Rotenberg KS, Vora K, Sterman AB, Thevathasan L, Ryan MF, et al. Comorbidities, Concomitant Medications, and Diet as Factors Affecting Levothyroxine Therapy: Results of the CONTROL Surveillance Project. Drugs R D. 2016 Mar;16(1):53-68. doi: 10.1007/s40268-015-0116-6.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Very interesting post indeed!
Why is coffee and food OK with liquid T4? What is different with the tablets?
Standard information we hear is that the absorption of the coffee / food blocks T4. But as I write that, if this, if was a block issue wouldn’t it eventually get absorbed? Or maybe the T4 gets inactivated aka converted to something else. Or it’s just one section of the small intestine that absorbs T4 and the coffee / food blocks things there causing the T4 to move on to where it cannot get absorbed.
Regarding general absorption issues, wouldn’t fixing an underlying gut issues be better than just switching to liquid T4?
John – thank you for reaching out. <3 While I advocate for healing the gut, those with healthy gut function still need to take their tablet thyroid meds at least 30-60 mins apart from food, as the dissolution of the tablets themselves is delayed when one’s gastric pH is increased, and food may delay this process both by a direct effect and/or by increasing the gastric pH. Furthermore, thyroid medication can interact with certain foods and minerals found in them. However, Tirosint liquid, which does not need to dissolve, will be more quickly absorbed, even in the presence of food.
I have been taking tirosint for about 3 years. I feel so much better with it. My current problem is it is hard to get as a prescription now, and I will be 65 in a few weeks. Medicare will kick in and my new Dr. doesn’t know anything about it. It is very expensive and my previous insurance canceled it,so cannot get it. I only have 9 pills left. Spreading them out, and can feel the difference, little depression and joint pain. Any solutions on where or how to get another prescription? Thank you,Clare
Clare – thank you for following.❤️ You may want to try utilizing the cost savings info referenced in the article above, as well as contact the manufacturer customer service line 800-587-3513 or email medinfo@ibsapharma.com, to see if they are offering discount programs. I also recommend checking with your practitioner to see if they can get free samples as well. I recently wrote a comprehensive overview of the available medication options out there, that you might find helpful as well. Here is a link so you can check it out:
MEDICATIONS FOR HASHIMOTO’S AND HYPOTHYROIDISM
https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/
It is my understanding that it is not the coffee that interferes with thyroid medication absorption but the milk/cream that people use in their coffee. That’s why there is a blanket statement saying that coffee interferes with thyroid medication. True or false? Please clarify.
Kathy – thank you for reaching out. <3 Here is an article I wrote that you might find helpful: https://thyroidpharmacist.com/articles/controversy-coffee-bad-thyroid-myths-truths/
I have been taking Tirosint for about six months now, at first I was excited to be able to participate in my family breakfast again! My TSH did jump to 2.5, so now I wait at least an hour before eating or drinking anything. Before, I had to wait more than 2 hrs before having anything at all. I get to eat breakfast again, to have a more ‘normal’ start to my day. Also, it’s helping me eliminate all dairy, which was what I learned after completing your protocol. Thanks for writing about this, it could definitely help others.
Emily – thank you so much for sharing! I hope you will continue to keep me posted on your progress. <3
Dr. Wentz,
I have been taking Tirosint 50MCG Cap IBS for a couple years due to problems with other medications , so far I have been satisfied except for the cost. I will look into the liquid.
You may not want to answer this question but, I will ask anyway. I am schedule to fly to Ireland in late August 2020 on a prepaid travel package. I do not feel I should attend as I have an Autoimmune Disease in addition to being in a high risk age group (79 years of age). My primary said that he would write a letter but, what wording would you suggest allowing me a medical cancellation? As of now, a decision to cancel the package will not be told to participants until June 1, 2020.
I appreciate your input.
Roberta Randall
Roberta – thank you for reaching out and sharing! <3 I am not able to advise on this without a comprehensive health assessment. I will have to defer to your practitioner who is familiar with your health history.
Dear Dr.Izabella Wentz,
I greatly appreciate your great informations.
What is your opinion about metabolic treatment of fibromyalgia and connection fibromyalgia and thyroid?
Thank you.
Dr.Anna Fischbein.
Dr Anna – thank you so much for following! <3 Here is an article I wrote on fibromyalgia that you might find interesting: https://thyroidpharmacist.com/articles/pain-hashimotos-and-fibromyalgia/
I take Tirosint but it doesn’t come in a Pill Planner.
Lisa – thank you for sharing! <3
It would not work for me because I need T 3 also. I take pig thyroid
NP thyroids and it works
Marjie – thank you so much for sharing! <3 I'm so glad you have found what works for you!
I have been taking half of 25 mcg synthroid (so 12.5 mcg) and have elevated HR and heart palpitations despite an extremely low dose. Struggling to find something I can tolerate. No terrible symptoms in general, healthy 30 yo female trying to conceive.
Melanie, thank you for reaching out. <3 I understand how frustrating this can be. There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication which you are looking for, ask your local pharmacist for doctors in your area who prescribe the medication you are looking to try. Have you read these articles?
HOW THE DOSE OF YOUR THYROID MEDICATION CAN UNCOVER YOUR ROOT CAUSE
https://thyroidpharmacist.com/articles/the-dose-of-your-thyroid-medication-can-uncover-your-root-cause/
WHICH THYROID MEDICATION IS BEST?
https://thyroidpharmacist.com/articles/which-thyroid-medication-is-best/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
Yes – but…
I was on Tirosint several years ago and while it initially increased my energy – after a while all that zip basically disappeared. One of my doctors gave me a prescription for NP Thyroid, which worked wonders for almost 2 years (it gave me my active lifestyle back). Then in the fall of 2019 the wheels fell off. Energy crashed and all sorts of symptoms appeared. Was glad to discover I wasn’t the only one, many people were having trouble with the med after the company switched their source material supplier. Tried a combo of generic T3/T4 – gave me a lovely rash… Finally decided to head back to Tirosint.
Can’t truly say how well it was working initially since I was recovering from ankle surgery (late January). But energy just wasn’t coming back and I seemed to have a combination of hypo and hyper symptoms (TSH gradually increasing). Asked for a slightly higher dose – that resulted in hot flashes, insomnia, weird heart rates and pains in my chest. And it only randomly improved my energy. I’ve read of a number of people having problems getting it balanced.
So now I’m back to square one and dealing with doctors who just look at TSH and tell me that once you have Hashimoto’s your thyroid problems will continue to get worse.
Recently gave up dairy (have been gluten free for years) – jury still out on that. All the other dietary recommendations may make sense for some people, but an enormous problem for people like me who have IBS.
Sally – thank you so much for sharing your journey with me. I’m so sorry you have had to experience all of this. <3 My heart goes out to you. We know that intestinal permeability (aka leaky gut) is present in every case of autoimmunity and often precedes the development of Hashimoto’s. Symptoms of leaky gut may include bloating, diarrhea, constipation, stomach aches, acid reflux and irritable bowel syndrome. According to the Institute of Functional Medicine, many people develop IBS 5-10 years before an autoimmune diagnosis. I was one of them and didn’t take my gut health as seriously as I should have. Gut problems are often caused by infections like H. pylori, parasites like Blasto, SIBO, an imbalance of bacteria, and enzyme deficiencies or food sensitivities (especially to gluten, dairy, and/or soy). Even stress can be a factor in gut permeability. Here is an article you might find interesting.
6 DIFFERENT ROOT CAUSES
https://thyroidpharmacist.com/articles/6-different-hashimotos-root-causes/
Wow, I’m blown away at how much I learned by reading your article! I started with Graves disease about 15yrs ago. Took radioactive iodine and immediately went hypothyroid. Over a spam of 11yrs Synthroid never worked for me. My levels were never normal. A year ago I found a clinical study on Tirosint. I immediately requested from my endo at Mayo Clinic. I saw immediate results and for the first time in 15yrs I had normal thyroid levels! All of a sudden the Tirosint isn’t working though. Your article mentions gastritis, which I have. I’m super curious on what I can do to make this medication absorb. I take it 1.5 hrs before any coffee. I’m confused and angry, I just want to feel better.
Carrie – thank you so much for sharing. I’m sorry to hear that it is not working for you. <3 Please understand, I am not able to advise you without a comprehensive health assessment. I recommend discussing this with your practitioner whose familiar with your health history.
Hello Izabella!
I´ve been struggling many years to find the right thyroid medication until I found Tirosint – they are working much better than any others! I´m still very sensitive to raise the dosage, so needed to go back to less than 50 mcg. In this case, its easier with Tirosint, because they have their exclusive 13 mcg! Today I take three 13 mcg – as it absorbs better, they probably are stronger than the normal medication on the market. What do you think, are they stronger?
thanks for an intresting study!
all the Best
Claudia Radomska
Claudia, thank you so much for sharing! I’m glad the Tirosint is working well for you! I hope you will keep me posted on your progress. <3
I switched to Tirosint 100mcg and 10mcg (total dose) of T3 after a decade of trying to get NDT dose right. My TSH that had been suppressed for 10 years is now in the normal range (not sure how much that really matters) but my RT3 is high now three months after the switch. Not sure if that means the Tiorsint dose is too high, the T3 is not needed or its just not being utilized correctly. No symptons of being hyper at all. My doc is no help, says RT3 is harder to clear as we age. But I didn’t have high RT3 on NDT so I’ve only aged 3 months since then. Any suggestions welcomed and appreciated. I’ve been taking the Tirosint at bedtime and Two 5mcg of T3 during the day.
Janet – thank you for reaching out. You may want to consider working on supporting your adrenals. In some cases, even natural desiccated thyroid can further stress the adrenals and increase your reverse T3. Adrenal protocols, including supplements, as well as eating frequent meals, meditating, and going to bed early can be helpful. Here is an article you might find interesting: A
ARE YOUR ADRENALS SABOTAGING YOUR HEALTH?
https://thyroidpharmacist.com/articles/are-your-adrenals-sabotaging-your-health
Tirosint has changed their coupon program since this article was published. The maximum discount is now $85 (not $105). For me this meant that my monthly cost went from $30.17/month to now $72.61/month, more than double the cost from my pharmacy.
Getting it though the Tirosint direct order program may be the most cost effective option for many people.
Though I appreciate the option to have an allergen-free medication, our laws should be as such that ALL medication ingredients/allergens/cross-contact should be fully disclosed by the manufacturer. Unfortunately, this is not the case in the US, making it very difficult for people with allergies or food intolerances to be sure they are getting safe medications (both prescription and over the counter).
Cate – thank you so much for letting me know! ❤️ I understand how frustrating this all is. It comes down to what is cost effective for the manufacturer to use as a filler. If you are highly reactive to the standard fillers, I recommend looking for a compounding pharmacy, who can make an individualized medication with an appropriate dosage and fillers right for you. Here is a resource I hope you find helpful.
COMPOUNDING PHARMACIES
https://thyroidpharmacist.com/database-recommended-compounding-pharmacies/
I live in California where I believe my naturopathic doctor is being monitored/harrassed regarding prescriptions she authorizes – in my case, Armour thyroid. I’m on medical which covers the cost but is making it more difficult to fill my prescription when I need it – refills. Any ideas how to expedite this process – alternatives. Thanks, Kirk
Kirk – thank you for reaching out. I’m so sorry for your practitioner! You could try a different pharmacy or talk to your pharmacist to see what the best optionn is to avoid all of this! Please keep me posted.❤️
Hi Izabella,
Thanks to you I took the rains of my thyroid health (my whole health) since 2018 after 15 years taking Synthroid.
Since switching to Tirosint gel caps I’m able to exercise every day and feel better overall. But the recent TSH lab results came back low. I’m having difficulty finding a knowledgeable physician who can adjust my Tirosint dosis correctly to prevent hyperthyroidism. I appreciate all the work you do.
Marie – thank you so much for sharing. I’m so glad to hear you have taking charge of your health and are feeling better overall. ❤️ I do have a practitioner database that you might find helpful. Here are a couple links:
CLINICIAN DATABASE
https://thyroidpharmacist.com/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
Hello. I have been following your work for several years and 100% attribute it to my improved thyroid health. I recently had labs done, though, and my reverse T3 levels shows <5.0. I was wondering if that was too low? It's out of optimal range, but I know the lower the number the better Free T3 should be doing. Of course, Free T3 still isn't up in optimal range, it's at 2.7 pg/ml. Thank you so much for all of the help you provide to so many people through your research!
Katie – thank you for following! Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones.
TOP 10 THYROID TESTS AND HOW TO INTERPRET THEM
https://thyroidpharmacist.com/articles/top-10-thyroid-tests/
I have been on 50 mg of Tirosint for a year and it has helped me a lot, but my hair is still shedding and dry along with my skin. I was wondering if adding a t3 to my current medication will help?
Marilyn – thank you for following. Sometimes, when your TSH is on the outskirts of the normal range, you can continue to lose hair, and your hair may lack luster and shine. If your hair tangles easily, this is a sign that you may not be getting enough thyroid hormone. Talk to your doctor. You should see a change within 4-6 weeks. Consider the type of thyroid medication you are taking. T3, the more active thyroid hormone, is your “beautiful hair” hormone that helps you grow your hair and prevents it from falling out. Synthroid, Levoxyl, and Tirosint only contain T4, the less active hormone. T4 should be converted to T3 in the body…except this doesn’t always happen. Sometimes an addition of Cytomel**may be cross-contaminated with gluten*** (a T3 medication) or a switch to a medication that contains a combination of T3/T4 such as Armour, Nature-Throid or compounded T4/T3 may result in a return of your hair’s luster and shine.
WHICH THYROID MEDICATION IS BEST?
https://thyroidpharmacist.com/articles/which-thyroid-medication-is-best/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
https://thyroidpharmacist.com/articles/top-11-things-you-need-to-know-about-thyroid-medications/
Hi, this was a great article . Did you continue on the NDT and add in tirosint during your pregnancy? I’m currently in that boat. I need more t4 and not t3 . Just wondered if you continued the NDT with the tirosint or completely switched to the tirosint . Thank you!!!
Chelsea, thank you for following. What works for one person may not work for another. I recommend discussing your options with your practitioner to help you determine the best option for you. Here is an article with more info that I hope is helpful: https://thyroidpharmacist.com/articles/medications-for-hashimotos-and-hypothyroidism/