After I was diagnosed with Hashimoto’s, I eventually connected all of the dots between my acid reflux, IBS, bloating, stomach pain, and autoimmune thyroid condition. Research has shown that every case of autoimmunity is associated with intestinal permeability, and I was sure that I had intestinal permeability – I just wasn’t sure what was driving it. [1]
I knew foods could play a factor, and I saw incredible improvements in my IBS and acid reflux when I cut out gluten and dairy. But then I hit a healing plateau, despite eliminating more and more foods. Some of my digestive symptoms even started to come back! I didn’t realize that I had underlying gut infections until I used the BioHealth 401H test – this revealed that I had a protozoal infection, while other tests showed high levels of yeast and H. pylori (all three are drivers of gut permeability and Hashimoto’s). This particular test is no longer available, but a readily available test that has helped many of my clients is the Gastrointestinal Microbial Assay Plus (GI-MAP®).
This is a comprehensive stool test that detects a wide range of bacteria, opportunistic organisms, overgrowth in normal flora, viruses, fungi, and parasites. The test also reports on several key markers of inflammation, digestion, and immune function.
I have found that this test covers many of the commonly seen gut pathogens that I come across with my Hashimoto’s clients, including H. pylori, the parasite Blastocystis hominis (Blasto), and any number of common bacteria such as Staphylococcus and Streptococcus.
Additionally, digestion and immune markers can be very helpful in pointing to other root cause issues to explore.
Along with evaluating symptoms and identifying your health and family history, this type of testing is often the best way to identify your particular set of triggers. Based on my experience, most people with Hashimoto’s have one or more of these pathogens, or abnormal markers, show up on their GI-MAP test.
I wrote this article because I believe it is so important that you understand how to interpret your test results.
This article discusses:
- Why the GI-MAP test can be valuable (pros and cons of the test)
- How to order the GI-MAP test and what the collection process entails
- What you need to know to interpret the GI-MAP report
- How to learn more about finding your root cause
Why the GI-MAP Test Can Be Valuable (Pros and Cons of the Test)
The GI-MAP test is one of my “go-to” fundamental tests for those with Hashimoto’s and/or gut-related symptoms. (It is also a great test to take if you have non-GI symptoms, as we know that so much of our health, including our immune system, nutrient absorption, and detoxification, takes place in the gut.)
Compared to other stool tests available, the GI-MAP test provides a unique benefit. It indicates the quantities of bacteria, viruses, fungi, and parasites present in the stool using a testing methodology called qPCR (versus simply reporting a positive or negative result, like many other tests).
Accurately assessing how much of an organism’s DNA is present in a patient’s stool sample is helpful for practitioners in determining the clinical significance of pathogenic organisms, and gives insight into overall gut dysbiosis patterns.
The GI-MAP is an incredibly helpful tool for determining root causes such as gut infections, microbiome imbalances, inflammatory conditions, and leaky gut. The test results can also point to potential triggers to investigate, such as possible food sensitivity concerns, exposure to environmental toxins, low stomach acid, and nutrient deficiencies.
In my clinical practice, some 90 percent of clients who seem to have stopped improving with regards to symptoms and/or thyroid lab results – even after dietary changes, supplements, and other protocols – find they have some type of gut infection or microbiome imbalance. The GI-MAP test can help identify these types of triggers.
In 2015, my team and I analyzed the data from 298 clients and participants enrolled in our Hashimoto’s Self-Management Program (HSMP) who took the GI-MAP. We found that many gut-related conditions are commonly associated with Hashimoto’s. You can read about these common gut conditions and their treatment protocols here.
The GI-MAP has consistently given me helpful insights for my clients (and myself) on potential triggers to investigate, such as low stomach acid, PPI or medication use, possible food sensitivity concerns, nutrient deficiencies, and exposure to environmental toxins.
It’s also important to bear in mind potential shortfalls. The GI-MAP test may miss some of the following common root causes found in Hashimoto’s:
- To detect SIBO, I recommend a SIBO breath test instead (available via Rupa, Direct Labs, MyMedLab, or the Trio Smart breath test).
- For Candida and mold, the Organic Acids Test (OAT) by Mosaic Diagnostics may be more accurate than the GI-MAP test.
- Yersinia is best detected via blood tests.
- For the Epstein-Barr virus, I recommend a blood test like the EBV Panel Plus test (most important in my experience is the Early Antigen Test).
- Some pathogens and parasites will not be detected on the GI-MAP because parasites may not shed in every single bowel movement. My workaround, which I cover later in this article, is to take samples from at least three different bowel movements. Other tests on the market may have more impressive parasitology testing methodologies, including the Gut Zoomer and ParaWellness Research Test.
Other stool tests besides the GI-MAP test that are helpful include the Comprehensive Stool Analysis + Parasitology 3-Day test by Doctor’s Data, the Comprehensive Stool Analysis by Mosaic Diagnostics, and the Gut Zoomer test. I have used all of these tests with clients. There’s a lot of discussion in the functional medicine space about which tests are best, but I have the most experience with the GI-MAP, so this is why I decided to write about it. 🙂
Please note that no test on the market is perfect; false negatives and false positives have been reported in various tests!
This is why I typically recommend multiple tests (if your budget allows), such as including one or more of the above. But I have found that the GI-MAP test results in fewer false negatives than some others, due to the fact that the report data is quantified (giving you specific levels of different microorganisms) versus just telling you if your results are positive or negative (with no specific levels provided).
Remember that all test results should be evaluated along with a person’s family history, health history, symptoms, thyroid labs, and other labs. Here’s an article outlining some key lab tests I routinely recommend.
How to Order the GI-MAP Test
Your functional doctor will likely be more than happy to order you the GI-MAP test, but you do not need a practitioner to order it. You can order the GI-MAP test yourself online through my Rupa portal or my testing portal at DirectLabs®. Once you have ordered the test, you will receive the GI-MAP Collection Kit.
Note that comprehensive stool tests such as the GI-MAP may not be covered on your insurance plan, so you will need to check. Some insurance companies may pay a portion only if ordered by an Osteopath (DO), Medical Doctor (MD), Physician Assistant (PA), or Nurse Practitioner (NP), and one who has registered – or who will register – on the DirectLabs site. Unfortunately, I’ve found that not many conventional doctors are willing to do so. Note that testing services are not available in MD, NY, NJ, or RI.
When your collection kit arrives, you’ll see the following contents:
- 1 – Kit box
- 1 – Test request form (you’ll need to fill out this information)
- 1 – Stool collection tray
- 1 – Stool specimen vial
- 2 – Gloves
- 1 – Zip closure specimen bag
- 1 – Absorbent pad
- 1 – FedEx Clinical Pak Mailer (provides free shipping back to the lab)
It’s important that you review the collection instructions and materials prior to starting your collection. The stool sample collection process is time-sensitive.
Should you want to read through the collection instructions prior to ordering or receiving your kit, they can be found online on the GI-MAP vendor site (Diagnostic Solutions Laboratory) as well as in this PDF.
The Collection Process
The collection instructions in the test kit are very clear, but may need to be slightly modified should you want to collect samples from multiple bowel movements.
Three-day collection process: To do this, instead of taking four separate spoonfuls of stool samples from one bowel movement, you will take one spoonful per day for two days, and two spoonfuls on the third day, keeping the specimen vial in the refrigerator in between samples. Make sure to add a sufficient sample amount from each bowel movement. Note that this method requires you to use a paper plate or other plate as a collection tray after you use the one collection tray provided (you only get one disposable tray, and you may require additional gloves). Always use clean plates and gloves so as not to contaminate the stool sample.
This three-day collection process will give you a greater opportunity to find any parasites that may otherwise be missed in a single bowel movement collection.
Time sensitivity: Note that if you do the three-day collection, please plan to ship the sample by the third day. Stool samples must be received by the lab within six days of the first day of collection.
Turnaround time frame: The GI-MAP processing time is roughly seven to ten days from receipt by the lab, and you will receive a notification when the results become available in your portal.
Interpreting Your GI-MAP Report
When you receive your GI-MAP results, the initial page will look something like this, and the entire report will be five or six pages, depending on if you ordered any add-on tests.
The different test categories are highlighted with a blue tab, and the layout of the report starts with reporting results of pathogens (bacterial, parasitic, and viral). The subsequent sections of the report then cover:
- H. pylori and virulence factors
- Levels of normal (commensal) bacteria flora
- Opportunistic bacteria
- Fungi/yeast
- Viruses
- Parasites
- Intestinal health markers
- H. pylori Antibiotic-resistant genes
- Any add-on tests, such as zonulin
Overview of Data
Here is an overview of the format and how to interpret each section.
You’ll notice that most sections have three columns. The first indicates what is being measured, the second reports your result, and the third offers you reference values. Any results out of the normal range are denoted in red, along with a comment relating to the particular result being high or low.
Other sections show your result as a colored bar with a black arrow indicating whether you fall into the “normal” reference range, or outside of the normal range (shown below).
Normal reference ranges were created by studying samples known to have specific harmful microbes. These ranges help identify the levels of microbes that can cause disease.
It’s important to keep in mind, however, that for some people (especially people with Hashimoto’s or other autoimmune conditions), levels of bacteria and pathogens even just slightly outside of the reference range can still contribute to symptoms.
For example, when I reviewed around 300 GI-MAP stool pathogen tests that I conducted with my clients and readers with Hashimoto’s over a three-year period, I found H. pylori to be positive in 21 percent of people. However, when looking at the results of people who had any level of H. pylori present (not just what the lab showed to be positive), 33 percent of people had the pathogen present.
In the past, I would only treat H. pylori if someone had a positive test result for it. However, as I began speaking to other clinicians about this test, I learned that some clinicians treat any detected levels of H. pylori with more natural, gentle protocols (instead of antibiotics).
I have found this to be beneficial, as in my experience, even low levels of pathogens can impede healing and contribute to symptoms.
The GI-MAP is most effectively interpreted when all factors from the entire report are considered together. A skilled practitioner will use the data from the GI-MAP to help them understand the patient’s overall condition and tailor treatment recommendations accordingly. Instead of treating each abnormal result as a separate issue, they evaluate each finding within the context of the complete report and the patient’s symptoms.
For the science nerds out there (like me), results are reported as “colony-forming units per gram of stool” (CFU/g).
One CFU is roughly equivalent to one microorganism. Results are expressed using standard scientific notation, per this table:
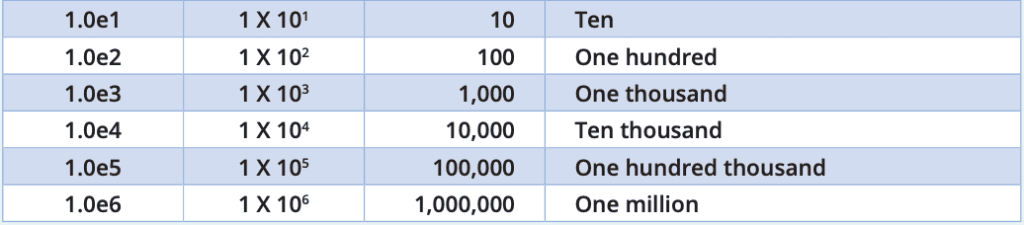
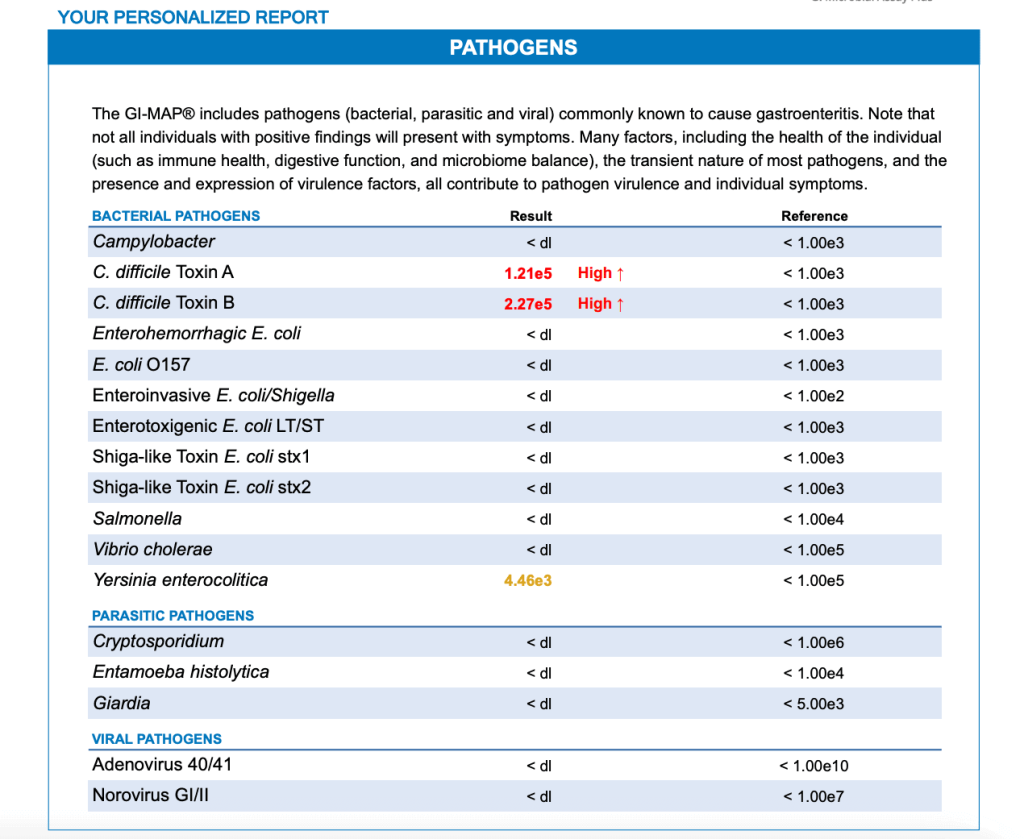
So in the following chart, a reported result of 8.79e4 for Campylobacter is equivalent to 87,900 CFUs per gram of stool (with normal being anything less than 1,000).
The <dl notation means the detection was under detectable limits.
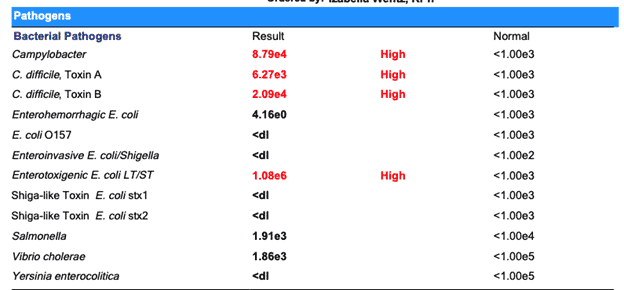
While some of the pathogens are over the normal detectable levels and marked in red, others are quantified, but not flagged. For example, we see that Salmonella was detected, but because levels are below the normal range, it is not flagged as “high.” As a practitioner, I use this information in the context of the whole report to determine a treatment plan.
A wealth of information is contained in the GI-MAP report. While the quantified numbers can be helpful, don’t let this information overwhelm you. The test identifies the most abnormal highs and lows, which is a great place to start in terms of treatment protocols.
For example, if your test results show you have “high” levels of H. pylori and detectable (but not “high”) levels of Staphylococcus, I would target the H. pylori with a treatment protocol first.
You can find common patterns I see on the GI-MAP and treatment protocols in this article.
While I find that many people have had success interpreting their own reports and implementing the suggested protocols, there is value in having a good functional practitioner look at the overall report. In particular, if you have positive findings or unexplained symptoms, it could be helpful to seek additional support.
Let’s go over the report, section by section, to help you get started on interpreting your GI-MAP.
Report Interpretation By Section
The GI-MAP is divided into sections – I’ll talk briefly about what each section of the report includes.
Pathogens
The GI-MAP provides measures of bacterial, viral, and parasitic pathogens known to cause intestinal issues. It also provides measures of toxin levels produced by certain pathogens. In our example above, we see that C. difficile Toxin A and Toxin B are both high. High levels of these toxins may mean the person is more likely to have leaky gut or other inflammatory conditions.
Based on the example report above, I would guess that this individual is likely dealing with many gastrointestinal symptoms. Please see my article on the common pathogens we find in Hashimoto’s using the GI-MAP test for more information and initial treatment protocols.
Bacterial Pathogens
Bacterial pathogens found on the GI-MAP include:
- Campylobacter
- C. difficile Toxin A
- C. difficile Toxin B
- Enterohemorrhagic coli
- E. coli O157
- Enteroinvasive E. coli/Shigella
- Enterotoxigenic E. coli LT/ST
- Shiga-like Toxin E. coli stx1
- Shiga-like Toxin E. coli stx2
- Salmonella
- Vibrio cholerae
- Yersinia enterocolitica
While any abnormal levels of these pathogens are worth noting, please also know that pathogens do not necessarily cause symptoms in everyone. If you have high levels of a bacterial pathogen and high levels of healthy commensal (friendly) bacteria, there may be enough good bacteria to limit any detrimental activity from the pathogen.
On the other hand, if you have high levels of a pathogen with low levels of commensal bacteria, then you’ll want to consider an intervention such as high doses of Lactobacillus and Bifidobacterium, to increase friendly bacteria in order to help keep the pathogenic infection at bay. If you’re experiencing symptoms such as digestive symptoms or pain, or if you’re unintentionally losing weight, please see your doctor as soon as possible. This may indicate a more severe infection that needs to be treated with antibiotics.
This is a great example of using the whole picture that the GI-MAP provides in order to inform a treatment protocol:
Parasitic Pathogens
- Cryptosporidium
- Entamoeba histolytica
- Giardia
Viral Pathogens
- Adenovirus 40/41
- Norovirus GI/II
The next section of the report focuses solely on a very common type of bacterium, H. pylori.
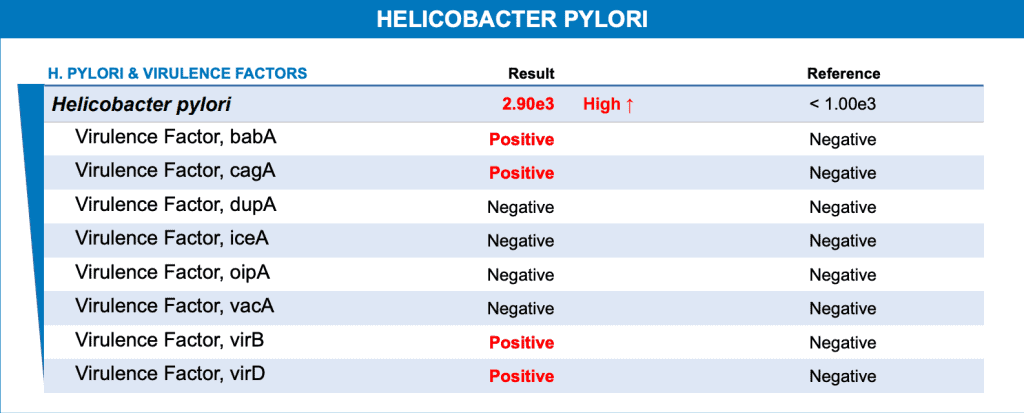
Helicobacter pylori
H. pylori is a common trigger for both Hashimoto’s and Graves’ disease. [2]
The GI-MAP provides an in-depth report on H. pylori, which also includes something called virulence factors. Virulence factors are molecules in pathogens that can cause disease.
In the following example, the patient tested high for H. pylori and was positive for several virulence factors. Virulence factors of H. pylori can lead to various stomach and upper intestinal diseases. [3] For example, the virulence factor cagA is associated with an increased risk for gastric cancer and peptic ulcer. [4]
When you see a virulence factor come back positive, I highly suggest consulting with your practitioner about all the details listed in the report.
H. pylori can cause a number of symptoms like acid reflux, food sensitivities, and an increase in thyroid antibodies. See my article on H. pylori for more information and treatment protocols.
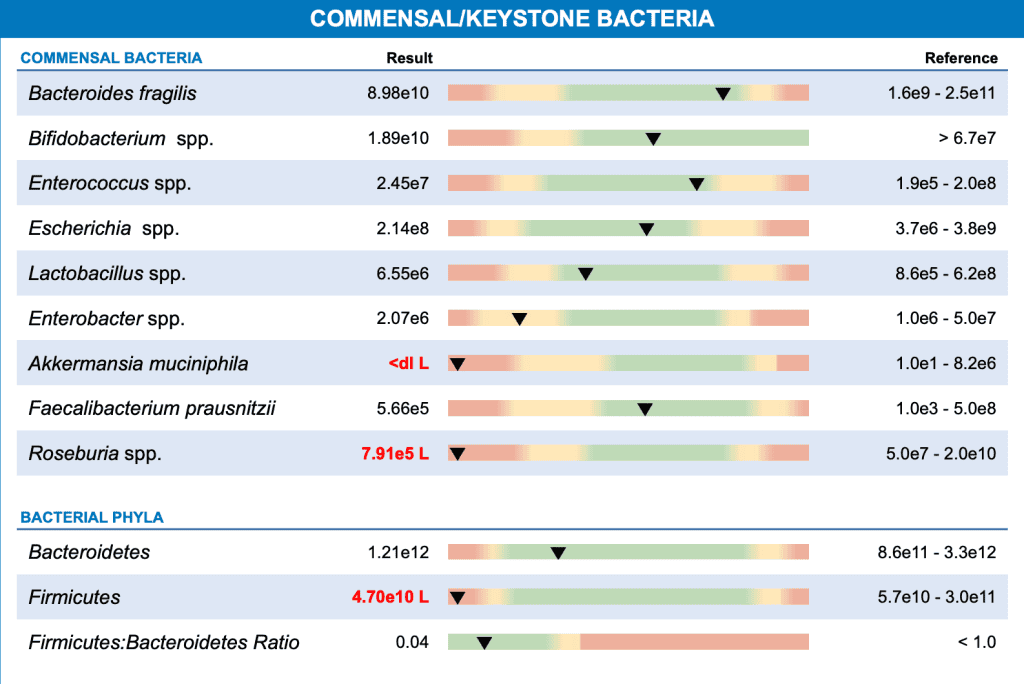
The next section of the GI-MAP report focuses on levels of commensal (beneficial) bacteria.
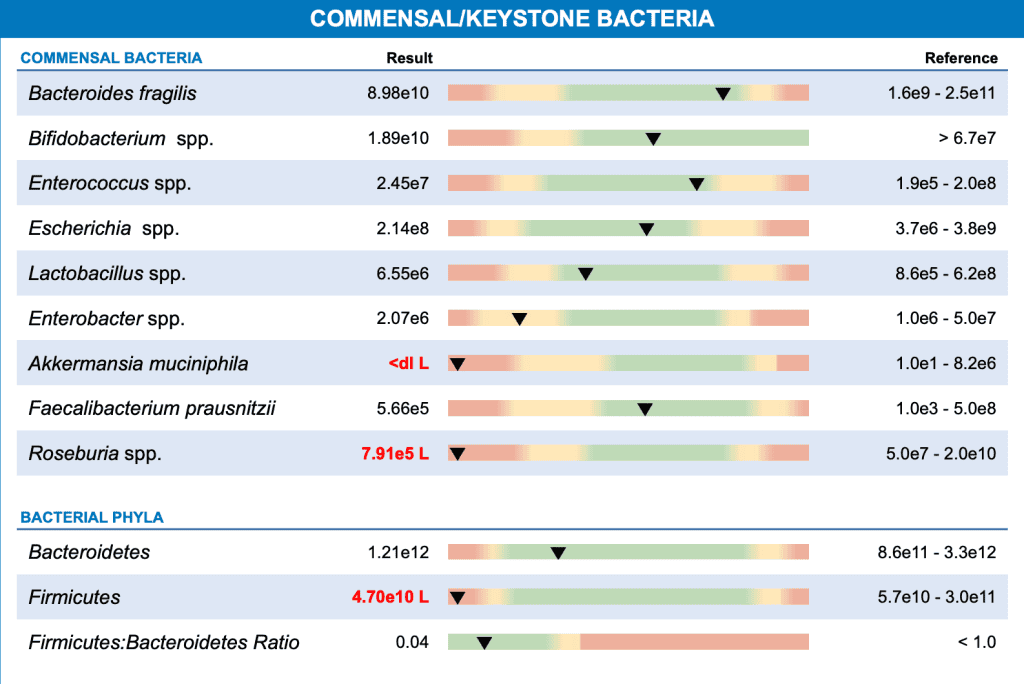
Commensal/Keystone Bacteria
Commensal bacteria are typically friendly and play numerous beneficial roles in our health – they help extract nutrients from our diets, maintain healthy gut barrier function, support our immune health, and protect us from potential pathogens. [5] A diverse and balanced gut microbiome also has anti-inflammatory and antioxidant activity. [6] An out-of-balance microbiome has been associated with inflammatory bowel diseases, autoimmune conditions, obesity, neurological disorders, and cancer. [7]
In part 1 of this article, I talk about some of the patterns I typically see in my Hashimoto’s clients. One very common pattern I see is low levels of beneficial Lactobacillus bacteria. You can read about common patterns I see on the GI-MAP in the linked article.
Another common pattern I see is low levels of Akkermansia. Low levels of this beneficial bacteria are associated with metabolic dysfunction, inflammation, type 2 diabetes, and obesity. [8] Supplementing with Akkermansia can be especially helpful for people who struggle to lose weight (Pendulum makes an Akkermansia-specific probiotic – use code THYROID20 for 20% off when you purchase a membership).
Here is a sample report showing commensal bacteria:
The next section of the GI-MAP report is focused on opportunistic bacteria.
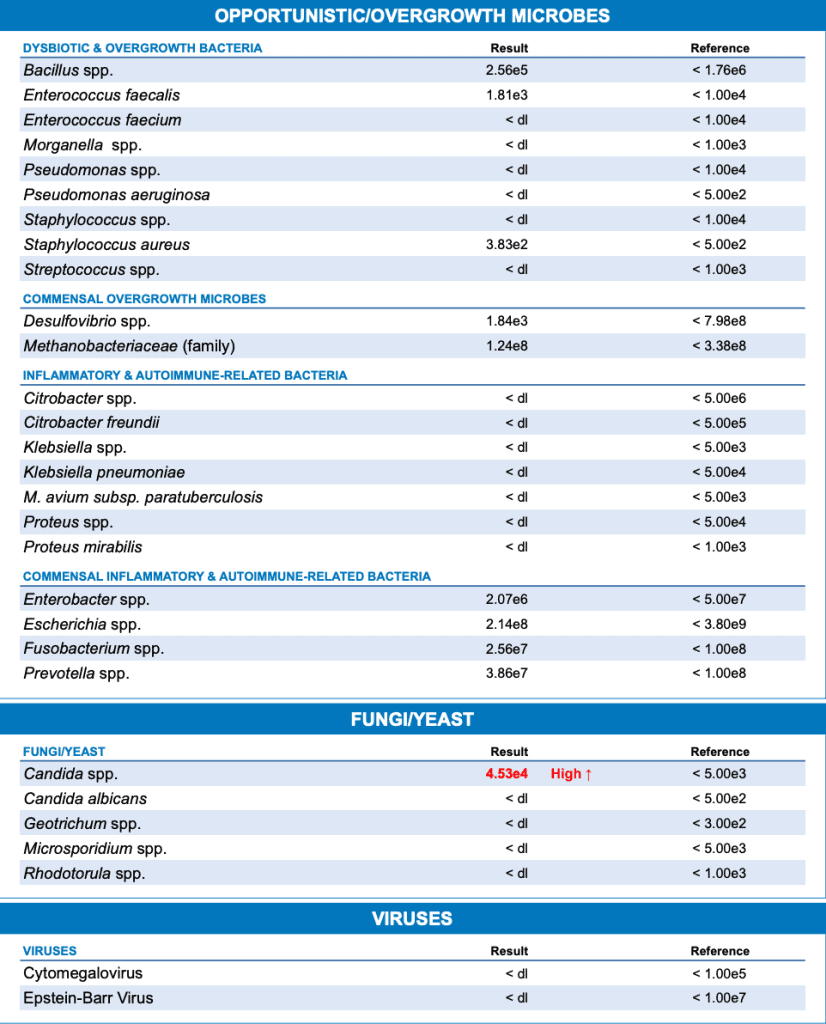
Opportunistic/Overgrowth Microbes
In my analysis of stool test samples, my team and I found various overgrowths of opportunistic bacteria in 59 percent of the samples.
Keep in mind that overgrowths don’t always cause disease or symptoms – in healthy people with robust levels of beneficial bacteria, opportunistic bacteria may not cause any issues. However, in people with compromised guts or immune systems, it’s more likely that these overgrowths will cause symptoms or lead to disease.
Certain bacteria have also been associated with triggering autoimmune conditions in susceptible individuals. [9] Chronic stress has been shown to suppress levels of beneficial bacteria in the gut, which makes it more likely for potentially pathogenic bacteria to proliferate. [10] I’ve found chronic stress to be a super common trigger for people with Hashimoto’s. Addressing both bacterial overgrowths and chronic stress can support a healthy gut in the long term.
This section also reports on yeasts such as Candida, a very common culprit in Hashimoto’s, which can cause symptoms such as fatigue, bloating, food sensitivities, brain fog, depression, constipation, and diarrhea. I used to routinely recommend the GI-MAP test for Candida, but after writing Hashimoto’s Protocol, I became more familiar with the Organic Acids Test (OAT) by Mosaic Diagnostics. I have found that this test is much more accurate and can find many more cases of Candida, as well as mold!
Staphylococcus and Streptococcus are other common overgrowths I see in those with Hashimoto’s, which can contribute to a number of ongoing symptoms. There is also a fascinating OCD connection with Streptococcus (important for us Type A individuals to understand!). I wrote a full article about the OCD-Hashimoto’s connection if you’d like to learn more.
I cover more common overgrowths and protocols in part 1 of this article.
Here is a sample report for this section of the test results.
The next section in the GI-MAP report focuses on parasites. I know many of you will be freaked out to find you have parasites (I know I was!), but a surprising number of people with Hashimoto’s are found to have parasites as a trigger. A parasite can cause a tremendous amount of damage, and it can cause intestinal permeability (leaky gut) and food sensitivities.
Parasites
In part 1 of this article, I discuss a commonly seen parasite called Blastocystis hominis (and review a number of treatment options). This parasite was found in about 29 percent of the people in our test population of 298 people. It can contribute to symptoms such as bloating, diarrhea, nausea, flatulence, abdominal pain, hives, fatigue, and food sensitivities.
I personally had Blasto at one point (along with chronic hives, IBS, and food sensitivities – all associated with the parasite), and getting rid of it helped me put Hashimoto’s into remission (I’ve seen this experience with others as well). To learn more about Blasto specifically, read my full article on it.
The GI-MAP reports on this parasite and many others. Here is a sample report on this section of parasites and protozoa:
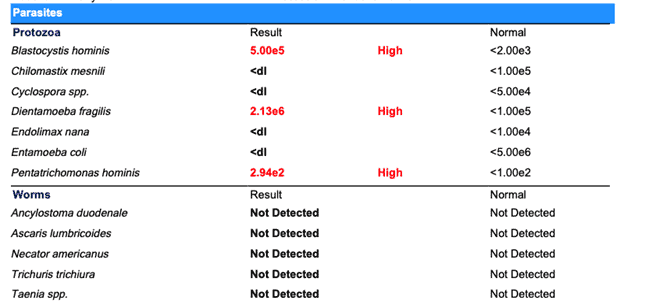
Remember, with all detected pathogens, there are a variety of resources available to help you – check out part 1 of this article, my website (you can search by topic such as “parasites” or “Blasto” here), and my books, Hashimoto’s: The Root Cause and Hashimoto’s Protocol. My latest book, IBS: Finding and Treating the Root Cause of Irritable Bowel Syndrome, also provides guidance in addressing parasites and numerous other overgrowths and infections that can contribute to IBS.
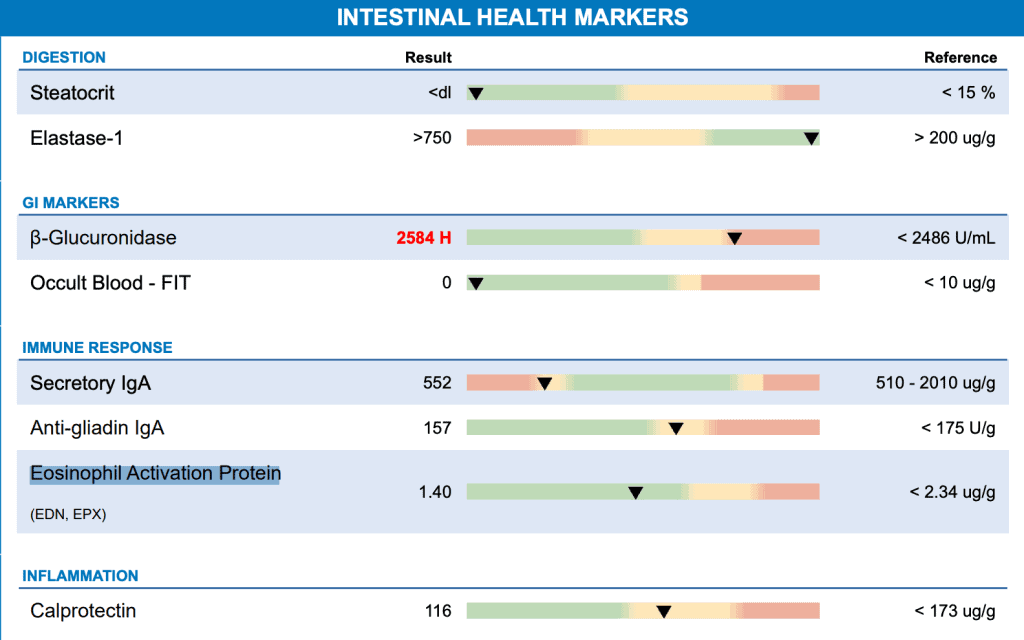
The next section of the GI-MAP test is focused on intestinal and immune health markers. This is a really interesting set of data.
Intestinal Health Markers
I will walk you through each of these markers.
Digestion
- Steatocrit – This digestion marker measures fecal fats in the stool, with high levels pointing to fat malabsorption issues, pancreatic insufficiency, small intestinal absorption issues, or even celiac disease. My article on fat digestion and pancreatic enzymes sheds more light on how this influences Hashimoto’s, and how to support optimal fat digestion.
- Elastase-1 – This marker provides the measure of fecal pancreatic elastase, a fat digestive enzyme that is secreted solely by the pancreas (so it is a direct indicator of pancreatic function). Low levels of elastase are often found in people with hypothyroidism and may point not only to suppressed pancreatic function, but to other issues such as low stomach acid, celiac disease, or SIBO, and should be explored further. Learn more in my article on pancreatic enzymes.
- If either of these two are elevated, this can lead to digestive issues, dry skin, and even asthma!
GI Markers
- B-Glucuronidase (Beta-Glucuronidase) – High levels of this marker can signal gut dysbiosis, leaky gut, SIBO, toxin (or medication) exposure, or a reduced ability for the body to detox estrogens. It may be associated with stomach cancer as well. [11]
- Occult Blood– FIT – Provides a quantitative measure of any blood found in your stool, even at microscopic levels. Blood presence can mean any number of gastrointestinal issues and needs to be evaluated further. The reference range is based on research suggesting that a measure greater than 10 ug/g may be a positive indicator of conditions such as polyps or colorectal cancer. [12] Many conditions can cause lower measures (< 10 ug/g) of blood in the stool, such as upper GI infections, liver disease, anal fissures, hemorrhoids, and some pathogenic infections (such as Giardia). Positive occult blood results should be evaluated further with your practitioner ASAP, as it can be an indication of something serious.
Immune Response
- Secretory IgA – SIgA is the primary immunoglobulin secreted into the gastrointestinal tract. Its main role is to protect the intestinal mucosa from pathogens. Higher than normal levels may indicate chronic infections or other inflammatory reactions (often due to food sensitivities). Low levels may indicate an impaired immune response in the gut, sometimes caused by mold or multiple infections.
- Anti-gliadin IgA – Gliadin is a component of gluten. The presence of fecal anti-gliadin antibodies can indicate an immune response to gluten. The presence of anti-gliadin antibodies is often used as a marker for non-celiac gluten sensitivity, which is common in those with Hashimoto’s (and why a gluten-free diet can be such a game-changer for so many people). Whenever I see the marker for this positive, it leads me to believe that someone is both gluten-sensitive and has been gluten-exposed. If they were eating gluten and not sensitive, this would be negative. If they were gluten-sensitive and not eating gluten, it would be negative as well.
- Eosinophil Activation Protein – This is a protein called eosinophils, released by immune cells. High levels are associated with intestinal inflammation and tissue damage, and serve as a marker for chronic inflammation in the GI tract. This may also indicate intestinal parasites.
Inflammation
- Calprotectin – This is a marker for intestinal inflammation. It can be elevated in a number of serious health conditions, including intestinal infections, inflammatory bowel disease, diverticulitis, polyps, and colorectal cancer. [13] Certain food allergens, drugs (such as non-steroidal anti-inflammatory drugs known as NSAIDs), and toxins can also be at the root of elevated calprotectin levels.
Here’s a sample test result of this section:
H. pylori Antibiotic Resistance Genes
The final section of the report (other than any add-on tests) indicates whether the specific DNA of H. pylori found in your report may be resistant to given antibiotics. These results will only be reported if the H. pylori result is 5.0e2 or greater.
Note that this section is really more useful for practitioners, as it shows them which antibiotic to prescribe. Also, as an aside, many functional practitioners (including me) would not necessarily address a given pathogen with antibiotics, but would instead prioritize the use of specific antimicrobial herbs. (Herbal protocols haven’t shown to pose the same risk for resistance, and typically have a low risk of negative side effects.) But should antibiotics be the choice of treatment, it is obviously good to know where there is built-in resistance.
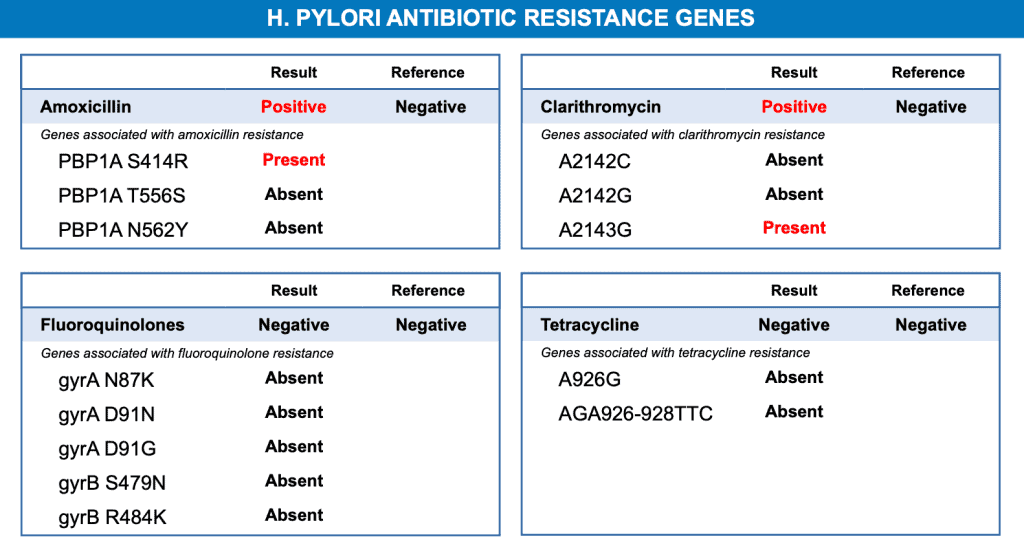
In this sample report, the individual’s result came back indicating their particular strain of H. pylori is resistant (“positive”) to the antibiotic clarithromycin. The numbers here represent individual SNPs (single nucleotide polymorphisms) that contain the antibiotic resistance trait.
This means that your practitioner would not want to use clarithromycin to treat your H. pylori, as it likely wouldn’t be effective. In fact, your practitioner wouldn’t want to treat you with clarithromycin for any identified gut infection, as gut microbes can share DNA, including the antibiotic resistance trait.
Optional Add-Ons
The following are optional and can be added onto your GI-MAP if desired:
- Zonulin – Fecal zonulin is viewed as a marker for intestinal permeability (leaky gut). Zonulin is the protein that is responsible for regulating the tight junctions in the gut lining that keep the gut lining intact. Elevated zonulin levels are generally associated with impaired intestinal barrier function, or leaky gut. I don’t usually recommend this test as it is an additional cost, and most people with Hashimoto’s have leaky gut.
- Gluten Peptide – This detects the presence of gluten in the stool. A positive result can indicate dietary exposure to gluten within the previous two to four days. If you eat gluten, this is to be expected, but for those who don’t, this marker can indicate accidental exposure or food cross-contamination. I don’t usually recommend this test unless you suspect you’re being exposed to gluten through an unknown source. In any case, I recommend reading all your food and supplement labels carefully first.
- Universal Antibiotic Resistance (AR) Genes Panel – Like the H. pylori resistance genes report mentioned above, this add-on panel detects the presence of genetic elements associated with antibiotic resistance. It can be useful in the case of stubborn or chronic infections, and again is a great tool for practitioners to help inform their treatment choices. As you may have gathered by now, I will often suggest herbal protocols for many overgrowths and infections, as they tend to be effective, even with antibiotic-resistant bacterial strains.
Learn More About Finding Your Root Cause
I find the GI-MAP test can be a valuable tool in your journey to discovering your own unique root causes, due to its comprehensive findings and ability to find root cause triggers, whether you’re experiencing gastrointestinal symptoms or not.
I recommend it because:
- People with Hashimoto’s nearly always have intestinal permeability. Intestinal permeability is one of the three requirements for having Hashimoto’s, the other two being genetic susceptibility and one or more triggers – so I always recommend people with Hashimoto’s focus on their gut health. The GI-MAP can help you understand what to focus on. [14]
- We know Hashimoto’s is an autoimmune disorder and about 70 to 80 percent of our immune system is in our gut. [15] Therefore, our gut microbiome is central to our ability to resolve Hashimoto’s and feel better. Research has found a link between the composition of the intestinal microbiota and susceptibility to many different systemic immune disorders. [16]
- Based on my experience with clients as well as my own personal Hashimoto’s journey, most people with Hashimoto’s will find they have microbial imbalances and/or gut infections of some kind.
- Our bodies’ response to pathogens, recognition and tolerance of self-antigens, sensitization to foods, and many other common functions that are also Hashimoto’s triggers, take place in the gut.
- I have found that non-GI symptoms such as brain fog, fatigue, depression, and joint pain, are often rooted in gut imbalances due to impacts on nutrient absorption, the health of our mitochondria, and overall inflammatory responses.
You can learn much more about common GI-MAP patterns I routinely see in Hashimoto’s in part 1 of this article. Seeing common patterns may help you identify one of your own triggers!
Additionally, there are many other resources pointed out in that article, both for learning more about a particular pathogen or marker, as well as treatment protocols should you test as positive.
If you are just starting your root cause journey, I suggest checking out the articles below, or scanning this list for any articles of interest:
- 6 Root Causes Behind Leaky Gut and Autoimmunity, which discusses some common root causes behind Hashimoto’s.
- The Fundamental Gut Health Protocol, which will give you a deeper understanding about the relationship between gut and thyroid health.
- Finding Your Root Cause: Key Lab Tests, which lists some important lab tests that can help identify your root causes.
If you are looking for comprehensive gut support with an actionable plan to help support intestinal permeability, microbial balance, and immune health, then I highly recommend you check out my Gut Recovery Program. It’s designed to help you get to the root causes of gut issues that are so common in Hashimoto’s.
This small group program focuses on total gut restoration where you will not just feel better, but also recover your gut health. We go deep to address the root causes of leaky gut and food sensitivities — and symptoms like diarrhea, constipation, acid reflux/GERD, stomach pain, headaches, nausea, food sensitivities/intolerance, brain fog, mood swings, and more.
Takeaway
Should you decide to take the GI-MAP test, I would love to hear from you about how it helped you in finding and resolving your triggers.
As always, we are in this together. Your findings and successes will help others in our community as well. Share your experience in the comments below!
P.S. I love interacting with my readers on social media, and I encourage you to join my Facebook, Instagram, TikTok, and Pinterest community pages to stay on top of thyroid health updates and meet others who are following similar health journeys. For recipes, a FREE Thyroid Diet Quick Start Guide, and notifications about upcoming events, be sure to sign up for my email list!
References
[1] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
[2] Dore MP, Fanciulli G, Manca A, Pes GM. Association of Helicobacter pylori Infection with Autoimmune Thyroid Disease in the Female Sex. J Clin Med. 2023;12(15):5150. Published 2023 Aug 6. doi:10.3390/jcm12155150
[3] Chang WL, Yeh YC, Sheu BS. The impacts of H. pylori virulence factors on the development of gastroduodenal diseases. J Biomed Sci. 2018;25(1):68. Published 2018 Sep 11. doi:10.1186/s12929-018-0466-9
[4] Parsonnet J, Friedman GD, Orentreich N, Vogelman H. Risk for gastric cancer in people with CagA positive or CagA negative Helicobacter pylori infection. Gut. 1997;40(3):297-301. doi:10.1136/gut.40.3.297
[5] Zhang YJ, Li S, Gan RY, Zhou T, Xu DP, Li HB. Impacts of gut bacteria on human health and diseases. Int J Mol Sci. 2015;16(4):7493-7519. Published 2015 Apr 2. doi:10.3390/ijms16047493
[6] Benameur T, Porro C, Twfieg ME, et al. Emerging Paradigms in Inflammatory Disease Management: Exploring Bioactive Compounds and the Gut Microbiota. Brain Sci. 2023;13(8):1226. Published 2023 Aug 21. doi:10.3390/brainsci13081226
[7] Zhang YJ, Li S, Gan RY, Zhou T, Xu DP, Li HB. Impacts of gut bacteria on human health and diseases. Int J Mol Sci. 2015;16(4):7493-7519. Published 2015 Apr 2. doi:10.3390/ijms16047493
[8] Verhoog S, Taneri PE, Roa Díaz ZM, et al. Dietary Factors and Modulation of Bacteria Strains of Akkermansia muciniphila and Faecalibacterium prausnitzii: A Systematic Review. Nutrients. 2019;11(7):1565. Published 2019 Jul 11. doi:10.3390/nu11071565; Abuqwider JN, Mauriello G, Altamimi M. Akkermansia muciniphila, a New Generation of Beneficial Microbiota in Modulating Obesity: A Systematic Review. Microorganisms. 2021;9(5):1098. Published 2021 May 20. doi:10.3390/microorganisms9051098
[9] National Institutes of Health. Gut microbe drives autoimmunity. NIH Research Matters. Published February 14, 2023. Accessed January 22, 2025. https://www.nih.gov/news-events/nih-research-matters/gut-microbe-drives-autoimmunity
[10] Madison AA, Bailey MT. Stressed to the Core: Inflammation and Intestinal Permeability Link Stress-Related Gut Microbiota Shifts to Mental Health Outcomes. Biol Psychiatry. 2024;95(4):339-347. doi:10.1016/j.biopsych.2023.10.014
[11] Cheng KW, Tseng CH, Chen IJ, et al. Inhibition of gut microbial β-glucuronidase effectively prevents carcinogen-induced microbial dysbiosis and intestinal tumorigenesis. Pharmacol Res. 2022;177:106115. doi:10.1016/j.phrs.2022.106115
[12] Saw KS, Liu C, Xu W, Varghese C, Parry S, Bissett I. Faecal immunochemical test to triage patients with possible colorectal cancer symptoms: meta-analysis [published correction appears in Br J Surg. 2022 Jun 14;109(7):644. doi: 10.1093/bjs/znac073]. Br J Surg. 2022;109(2):182-190. doi:10.1093/bjs/znab411
[13] Pathirana WGW, Chubb SP, Gillett MJ, Vasikaran SD. Faecal Calprotectin. Clin Biochem Rev. 2018;39(3):77-90.
[14] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
[15] Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients. 2021;13(3):886. Published 2021 Mar 9. doi:10.3390/nu13030886
[16] Shaheen WA, Quraishi MN, Iqbal TH. Gut microbiome and autoimmune disorders. Clin Exp Immunol. 2022;209(2):161-174. doi:10.1093/cei/uxac057
Note: Originally published in January 2025, this article has been revised and updated for accuracy and thoroughness.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Thank you for this information. I’m really interested in getting a GI map test done. Finding a functional doctor and testing is difficult to afford. I’ve done some research but from what I’ve read and the article above, I can order the GI map through this site that sends me to Rupa-I can order and have the test results myself? The results aren’t locked away until I hire a doctor?
Chelsea, great question! If you self order the results will be sent to you. Please feel free to email my team at info@thyroidpharmacist.com if you have any other questions and they will be happy to help.
Are you sure the 3-day collection method for GI-MAP won’t invalidate the test results? I’m following your advice and adding samples from 3 days, shaking moderately after each day’s sample to make sure it’s dissolved. Will be shipping it out on day 3. I’m concerned about parasites so am following your method, but worried about this off-label technique. Will the pink liquid in the vial still work as intended? Thank you so much for your response.
Hello, Great question! Once the stool is mixed with the solution, the GI-MAP test vial is good for 6 days starting from Day 1 of collection. Please be sure to keep the vial in the fridge during the three days you’re collecting. To keep things stress-free, send it as soon as possible, on the last day of collecting so it arrives at the lab on time. When filling out the paperwork, make sure to list the Day 1 collection date, as this lets the lab know the sample is time-sensitive. If you have any other questions please feel free to email my team at info@thyroidpharmacist.com and they will be happy to help.