How have you been enjoying the winter months? This time of year, I like to focus on immune support for my family. In previous years, I used to start in January, but thanks to preschool and kindergarten, I now focus on immune support starting in October. 🙂
I love taking reishi, S. boulardii and astragalus for overall immune health and to support secretory IgA levels, our own first line of defense in our respiratory and digestive tracts. We are also drinking bone broth and taking vitamin D.
Do you ever feel worse in the winter than you do in the summer? A deficiency in vitamin D and a certain spectrum of light may hold the key to feeling better.
Autoimmune conditions are more likely to cluster in regions farther from the equator, and scientists have suggested that one of the potential reasons for this may be due to inadequate vitamin D levels, as vitamin D is primarily produced by the skin when UVB light penetrates uncovered skin that is free of sunscreen. The cutaneous 7-dehydrocholesterol that is present in our skin is converted to pre-vitamin D3, which is then stored in our fat cells until it is needed. When needed, the liver and kidneys will transform the stored vitamin D into the active vitamin D3 form. [1]
Although those who live in warm climates are more likely to be getting enough of the sunshine vitamin, I often find that even people who live in warm climates such as Southern California, Florida, and Arizona, are vitamin D deficient at similar rates to people living in Wisconsin or Minnesota!
This is because our absorption of the vitamin from food sources is minimal, and is often further compromised by digestive enzyme deficiencies and gut conditions that lead to malabsorption of nutrients (such as infections and bacterial overgrowth).
As a result, vitamin D is one of the most under-recognized deficiencies in our society, and an estimated 85 percent of Americans may be deficient in it. [2]
Vitamin D affects about 3,000 to 30,000 genes in our bodies. You may know that it’s necessary for helping our body to absorb calcium and strengthen our bones, but it also plays an important role in our immune system health, keeping its delicate balance in check. Vitamin D may prevent and modulate autoimmunity, while a deficiency in vitamin D is associated with improper immune function. [3]
Many diseases have also been connected to low vitamin D levels, including heart disease, autoimmune disease, depression, and recently, thyroid conditions, including Hashimoto’s. [4]
Optimizing your levels of this important nutrient may be a key part of the puzzle of restoring your health.
In this article, you’ll discover:
- The role of vitamin D within the body
- The link between vitamin D deficiency and thyroid conditions
- How to test for vitamin D deficiency
- Lifestyle tips and supplements to boost your vitamin D levels
What is Vitamin D?
Vitamin D is an essential nutrient and a precursor hormone that plays an important role in many biochemical functions within the body. The body produces vitamin D from cholesterol, when our skin is exposed to sunlight. Vitamin D is also found in certain foods, such as fatty fish and fortified dairy products. However, it is very difficult to get adequate amounts through diet alone.
Vitamin D has several important functions within the body, including the regulation of calcium and phosphorus absorption for bone and tooth growth.
This vitamin has also been shown to reduce one’s risk of developing multiple sclerosis (MS) and heart disease. [5] It plays an important role in regulating mood and preventing depression as well. In fact, researchers behind a 2013 meta-analysis observed that, statistically, people with low vitamin D were at a much greater risk of depression. [6] Another study found vitamin D receptors in the same areas of the brain associated with depression, and concluded that vitamin D plays an important role in brain function and mental health. [7]
Of note, vitamin D can also support the immune system. (In fact, there are vitamin D receptors and activating enzymes on the surfaces of all white blood cells!) By enhancing the pathogen-fighting effects of monocytes and macrophages — white blood cells that are important parts of immune defense — and decreasing inflammation, vitamin D can help reduce the likelihood of contracting viruses, such as the seasonal flu. [8]
An analysis of 10,933 trial participants, yielded the first definitive evidence that vitamin D does protect against respiratory infections. The results of the analysis revealed that, in trial participants, daily or weekly supplementation halved the risk of acute respiratory infection in people with the lowest baseline vitamin D levels (below 25 nmol/L). However, people with higher baseline vitamin D levels also benefited, although the effect was more modest (10 percent risk reduction). Overall, vitamin D supplementation was shown to be helpful in reducing the risk of acute respiratory infection.
The role of vitamin D in the health of the human body has been well described by researchers and the medical community alike. Recent studies have shown that serum vitamin D levels can be directly correlated with human life expectancy. [9] Dr. William Grant, Ph.D., a vitamin D expert, has proposed that raising the optimal serum vitamin D level would prevent 30 percent of cancer deaths each year.
While it is estimated that 1 billion people worldwide have low levels of vitamin D, most don’t realize that they’re deficient, as symptoms are often subtle. Indications that you may have a vitamin D deficiency include:
- Fatigue
- Bone aches
- Back pain
- Muscle pain and weakness
- Stress fractures (especially in your legs, pelvis, and hips)
- Frequent illness or infections
- Depression
- Impaired wound healing
- Osteoporosis
- Hair loss
Additionally, in those with Hashimoto’s, elevated thyroid antibodies may be a sign of a vitamin D deficiency.
Vitamin D and Autoimmune Thyroid Conditions
Numerous studies have connected low vitamin D levels to various autoimmune conditions. For example, a deficiency in vitamin D has been correlated with higher rates of type 1 diabetes. [10] In Finland, the incidence of type 1 diabetes in Finnish children increased when the daily recommended dosage of vitamin D was reduced from 4000-5000 IU in 1964, to 400 IU in 1992. Yet, incidences of diabetes in children have been decreasing since 2006, the year Finland decided to fortify all dietary milk products with vitamin D3.
Vitamin D may be beneficial in balancing the immune system through supporting the production of T-regulatory cells, and suppressing the Epstein-Barr virus, a virus that has been tied to numerous autoimmune conditions, including Hashimoto’s. [11] Research has also shown that vitamin D actively prevents the development of autoimmunity in animal models. [12]
Furthermore, there is a strong connection between vitamin D deficiency and various thyroid conditions. Vitamin D deficiency has been documented in Hashimoto’s, Graves’ disease, thyroid cancer, as well as postpartum thyroiditis. [13]
One study in Turkey found that 92 percent of Hashimoto’s patients were deficient in vitamin D! [14] In 2015, I surveyed 2332 of my readers with Hashimoto’s, and found that 68 percent of them reported being diagnosed with vitamin D deficiency.
In recent years, numerous studies have come out connecting vitamin D deficiency with the development of thyroid antibodies. [15] The lower the vitamin D levels, the higher the thyroid antibodies…
Studies have also found that vitamin D reduces thyroid antibodies (TPO antibodies as well as TG antibodies) in those taking levothyroxine, as well as in people who have “euthyroid” Hashimoto’s, where their TSH is still normal, but they have elevated thyroid antibodies. [16] A Greek study reported about a 20 percent overall decrease in thyroid antibodies with vitamin D supplementation. [17]
Interestingly, researchers have suggested that vitamin D can slow down and prevent the progression of Hashimoto’s.
Research suggests that vitamin D can also support cognitive function (concentration, attention, thinking, etc.) in individuals with Hashimoto’s. One 2018 study found that individuals with Hashimoto’s who had mild cognitive impairment, had lower levels of 25-hydroxy vitamin D. [18]
Vitamin D and Endocrine Health
Along with reducing antibodies and being beneficial to thyroid health, vitamin D has been shown to be helpful for women’s endocrine systems. One study found that women with normal vitamin D levels were found to have lower rates of endocrine and reproductive system conditions such as oligomenorrhea (infrequent periods), amenorrhea (missing periods), and other menstrual cycle irregularities. [19]
Furthermore, vitamin D has also been shown to inhibit uterine fibroid growth through its role in cell growth of uterine tissue. [20]
Who’s at Risk for Deficiency?
As skin cancer awareness and the use of sunscreen has become more widespread, most people are not getting adequate amounts of vitamin D through skin absorption. In fact, a clinical review published in The Journal of the American Osteopathic Association found that nearly 1 billion people worldwide may have insufficient levels of vitamin D related to sunscreen use. [21] The study also found that vitamin D deficiency can be more prevalent in certain populations due to differences in skin pigmentation. For example, 95 percent of African American adults may have vitamin D deficiency.
Furthermore, those living in northern climates are especially at risk for vitamin D deficiency in the colder months, when the body is covered up.
However, even those living in warm countries may be at risk for low vitamin D levels. According to a Spanish study, although Spain receives sufficient sunlight radiation, it is difficult for its population to attain the recommended daily dose of vitamin D in the winter, as sunlight exposure is affected by Spain’s northern latitude. [22] The study also noted that absorption could depend on the time of day and the position of the sun. At 10 am, almost 10 hours would be required to get enough vitamin D — but most people do not get 10 hours of sunshine — and if they did, that would be excessive exposure!
Additionally, those with pancreatic enzyme deficiency may be at risk for vitamin D deficiency. [23] If you are deficient in pancreatic enzymes, you will not be properly digesting and absorbing fats. As such, the body will not be able to optimally absorb and utilize fat-soluble vitamins such as vitamin D.
Testing for Vitamin D Deficiency
You may be wondering, how much vitamin D does your body need?
It’s interesting to note that according to some all-cause mortality studies, patients with vitamin D levels between 30-40 ng/mL had the lowest rate of dying. [24] Levels under 30 ng/mL and over 50 ng/mL had a greater association with dying, so it appears to be beneficial to have vitamin D levels in the mid-range.
That said, I am often suspicious of all-cause mortality studies because “all-cause mortality” means dying of any cause, and there are often a number of uncontrolled variables. For example, vitamin D will not protect you from dying in a car accident, nor prevent an armed assassin from showing up at your door.
While the conventional reference ranges define vitamin D deficiency as under 30 ng/mL, I have found that vitamin D levels should be between 60 and 80 ng/mL for optimal thyroid receptor and immune system function.
There are two common forms of vitamin D:
- Vitamin D2 (ergocalciferol) – This form is found in some fortified foods and certain supplements.
- Vitamin D3 (cholecalciferol) – This is the most biologically active form and is found in some high-quality supplements.
Vitamin D2 and D3 can both be converted by the liver and the kidney into the active form 1,25-dihydroxyvitamin D.
There are two available tests to check your vitamin D levels: 1,25 (OH)D (which checks for the active form of vitamin D) and 25(OH)D (which checks for both D2 and D3). The 25(OH)D (25-hydroxyvitamin D) test is preferred, as it tests for both vitamin D2 and D3 levels and more accurately reflects one’s vitamin D status.
In my experience of performing case reviews for people with Hashimoto’s, vitamin D is the most common deficiency, followed by ferritin. However, as vitamin D excess can be problematic, I always recommend testing for these nutrients before supplementing.
If you have Hashimoto’s and have not had your vitamin D levels checked, I recommend testing as soon as possible. When supplementing, I recommend testing every 3-6 months to ensure you are getting adequate amounts, and then testing again in the winter season.
How to Get Your Vitamin D
Studies are now suggesting that much higher doses of vitamin D than the original recommended daily allowance of 400 IU per day should be taken. In fact, some studies show that 25(OH)D levels under 75 nmol/L may be too low for safety, and are associated with higher all-cause mortality. [25] Moreover, one study found that a daily intake of 6201 IU was needed to achieve the Endocrine Society’s recommendation of serum 25(OH)D values at 75 nmol/L.
Furthermore, I believe that vitamin D is especially important for people who have had a prior Epstein-Barr infection, as the CD8+ T cells that fight the virus are vitamin D dependent.
So how can we get adequate amounts of vitamin D?
Vitamin D can be produced in the skin when exposed to sunlight, or it can be ingested from foods and supplements.
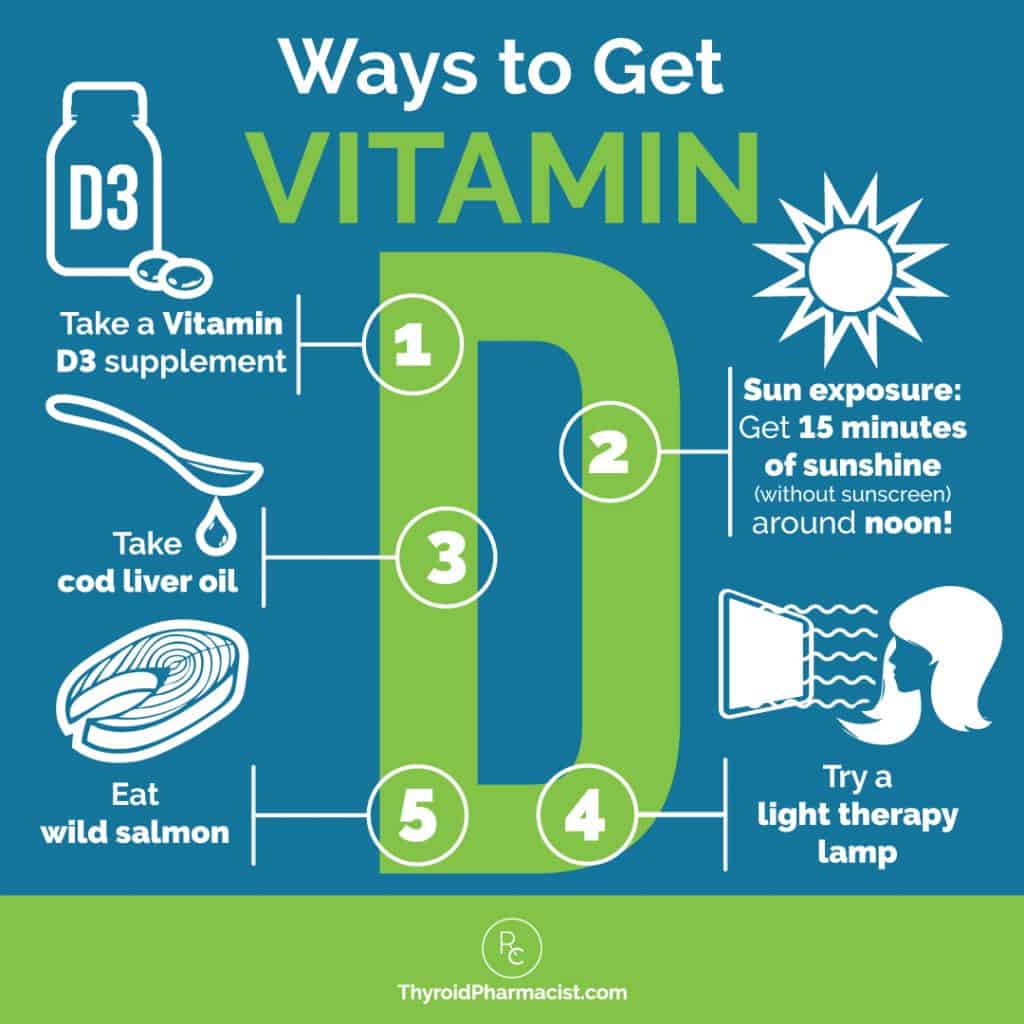
1. Get Outside
One of the best ways to restore optimal vitamin D levels is through sun exposure. (As a bonus, sunlight has natural immune modulating benefits, and can also lift your mood.)
You could say that boosting your vitamin D levels can be a “walk in the park.” 🙂 Vitamin D advocates recommend 15 minutes of unexposed skin, without sunscreen, around noon.
Perhaps you can consider going for a walk during lunchtime? If you are fair-skinned and not used to the sun, you may need to start slower. Be careful not to overexpose yourself, to prevent getting a sunburn.
However, some health care professionals suggest that in cases of severe deficiency, getting adequate vitamin D levels would require you to spend four to six hours exposed on a sunny beach… for seven days straight. Sounds awful, right? However, many of us simply can’t get to the beach and live in climates that do not provide us with adequate amounts of sun exposure yearound, so we’ll need to look for alternate sources of vitamin D.
Please note that people with darker skin tones may actually need more light, due to having more melanin in their skin. Studies have shown that people with darker skin require more sun exposure to achieve adequate vitamin D levels, versus light-skinned people. [26] Some sources say they need as much as six times more sun to get enough vitamin D! [27]
I generally recommend beach vacations for those of us living in Northern climates this time of year, but this isn’t always realistic for many! As such, we have to get sunshine when we can, as well as really focus on food and supplements.
2. Food Pharmacology
As we can also absorb vitamin D in the small intestine, we can get vitamin D from dietary sources, including wild salmon (which contains 800 IU of D3 per 3.5 oz), cod liver oil (700 IU per teaspoon), fish, fortified dairy products and orange juice, and eggs.
However, the amount of vitamin D we absorb from food is limited, and people with fat malabsorption, food sensitivities, and other digestive issues common in Hashimoto’s, may be further impaired in their ability to absorb nutrients. Additionally, dairy, eggs and sugary drinks can be problematic for people with Hashimoto’s and blood sugar issues, so I don’t recommend relying on these foods for adequate vitamin D. This is why supplementation can be incredibly helpful, and why I recommend vitamin D supplements for most people with Hashimoto’s.
3. Supplements
My recommendation for those who can’t get out in the sun, is to take an oral vitamin D3 supplement.
As the recommended daily allowance of 400 IU of vitamin D has been shown to be inadequate for most people, I generally recommend 5,000 IU per day as a starting point for my clients with Hashimoto’s. Taking your vitamin D supplements with a meal can be helpful in increasing its absorption by 30-50 percent. [28]
However, I also recommend monitoring vitamin D levels to ensure that levels are within the optimal range (60 to 80 ng/mL for optimal thyroid receptor and immune system function).
In some cases, practitioners may utilize doses as high as 20,000 IU to get to the goal, but I would not recommend doing this on your own, as vitamin D is a fat-soluble vitamin and can build up. (If you’re looking for a practitioner to help you on your journey, you can download my list of patient-recommended clinicians here.)
Please note: Some people with Hashimoto’s may also be deficient in vitamin K, especially when they have issues with fat malabsorption. Vitamin K deficiency is not routinely tested, but symptoms may include easy bruising, excess bleeding, and heavy menstrual periods. [29]
Supplementing with vitamin D when one is deficient in vitamin K can have a negative impact on our arteries. Vitamin D supplements liberate calcium from our bodies, and in the case of vitamin K deficiency, the calcium may go to our arteries instead of our bones. Adequate vitamin K can prevent arterial calcification and encourage more calcium into the bones, which is beneficial in osteoporosis, a common condition seen in people with Hashimoto’s. As such, I recommend taking vitamin D with or without added vitamin K, depending on your individual needs.
The vitamin D supplements I recommend include:
- Pure Encapsulations Vitamin D 5000 IU (without Vitamin K) — you can also purchase this through Fullscript. If you don’t have a Fullscript account, you can sign up with my credentials here.
- Designs for Health Vitamin D Supreme (with Vitamin K*) — you can also purchase this through Fullscript. If you don’t have a Fullscript account, you can sign up with my credentials here.
*Please note, soybean peptone is used as a raw material in the fermentation process for the vitamin K2. The finished vitamin K2 is tested for contamination of soy protein and contains less than 10 ppm (parts per million). If you do not tolerate soy, you may want to opt for the Pure Encapsulations version, without vitamin K, instead.
Additionally, vitamin K supplements are generally safe and well tolerated, but if you take blood thinning medications like warfarin, speak to your doctor or pharmacist before starting a supplement that contains vitamin K.
Blue Light Therapy – Another Winter Tool
If you find yourself feeling worse in the winter than you do in the summer (and especially if you have the winter blues), vitamin D may help, but you would likely have the best outcomes if you combined it with blue light therapy.
A recent study published in Scientific Report suggests that exposure to sunlight may be beneficial to our immune system, via mechanisms that are separate from vitamin D. [30] The researchers noted that blue light, in particular, which is produced naturally by the sun, may activate key immune cells and boost immune function. In their study, blue light exposure triggered the synthesis of hydrogen peroxide, which inactivated pathways that signaled an increase of motility of the T cells (which play a role in mounting an immune response against infections), in both mouse and human T lymphocytes.
Blue light is known to reach the second layer of the skin, where there is a higher concentration of T lymphocytes compared to those found in the bloodstream. The study, therefore, suggests that there could be a separate pathway through which sunlight — specifically blue light exposure — may boost the immune system.
Blue light therapy devices have also been studied in seasonal affective disorder (SAD), aka “the winter blues”, with great success. [31]
I like this blue light therapy device to reap the benefits of blue light exposure anytime, from the comfort of my home, without having to wait for the weatherman to announce a sunny day. It’s also great to have around during the winter. While I recommend using it for about 15 minutes a day, you can set the timer according to your needs. This light therapy can also be really helpful if you have trouble waking up in the mornings. I recommend keeping it at your bedside and turning it on when you wake up, or keeping it in your bathroom and turning it on while you get ready. The little blue light therapy device has helped me through many dark winters in Chicago, cloudy days in Amsterdam, and long Colorado winters.
A Word of Caution…
Some research has shown an interesting link between levels of two different forms of vitamin D (1,25-D and 25-D), autoimmunity, and thyroid health.
Research suggests that elevated levels of 1,25-D (the active form of vitamin D) may be linked to promoting autoimmune processes. A ratio of elevated levels of the 1,25-D form, and low levels of the 25-D form, is a result of inflammatory processes of the immune system, and further maintains an inflamed autoimmune response.
The high 1,25-D:low 25-D ratio is associated with changes in the VDR gene, which is responsible for producing vitamin D receptors (VDR). [32] Changes in how the VDR gene is expressed can lead to the dysfunction of vitamin D receptors — this may be how the inflammatory processes are maintained.
The 1,25-D form specifically has an affinity for thyroid nuclear receptors. Thus, elevated levels of this form of vitamin D can create dysregulation of thyroid hormone production by affecting T3 hormone activity through thyroid nuclear receptor activity.
Supplementing without testing for vitamin D levels (both 1,25-D and 25-D forms) can contribute to the detrimental high 1,25-D:low 25-D ratio, which then can be harmful to the thyroid. Those who are deficient in vitamin D may find benefit from supplementing with high quality vitamin D3.
However, as previously mentioned, excess vitamin D can be toxic… and may contribute further to the inflammatory (and thyroid damaging) high 1,25-D:low 25-D ratio. Thus, I always recommend getting one’s vitamin D levels tested and continuing to consistently monitor levels to ensure vitamin D levels are not too high.
The Takeaway
Vitamin D has been helpful in my recovery, and I’ve found that exposure to sunshine, vitamin D supplements, and blue light therapy are strategies that consistently make my clients and readers feel better. In my survey of 2232 people with Hashimoto’s, 67 percent of my readers reported their fatigue improved and said they felt significantly better after taking a vitamin D supplement. Improvements in mood, pain reduction, as well as a reduction in antibody titers, are also things I see time and time again.
Because of the prevalence of vitamin D deficiency in Hashimoto’s, and due to its known connection to autoimmune disease in general, I’ve recommended vitamin D testing and supplementing to my readers and clients since 2013. I have noticed that those who are struggling most with thyroid symptoms often have vitamin D deficiency; and those who feel their best and/or who are in remission from Hashimoto’s tend to have vitamin D levels between 60-80 ng/mL. While it’s not a magic bullet, optimizing vitamin D levels can be a really simple and inexpensive way to feel better and optimize the immune system.
I’d love to hear from you! How much sunshine do you get in your part of the world? Do you take a vitamin D supplement?
As always, I wish you the best on your journey to better health.
P.S. I love interacting with my readers on social media, and I encourage you to join my Facebook, Instagram, TikTok, and Pinterest community pages to stay on top of thyroid health updates and meet others who are following similar health journeys. For recipes, a FREE Thyroid Diet start guide, notifications about upcoming events, and the Nutrient Depletions and Digestion chapter from my first book for free, be sure to sign up for my email list!
If you’re curious about other vitamin deficiencies and symptoms related to them, you can download my FREE Supplements to Subdue Symptoms eBook below!
References
[1] Yang CY, Leung PS, Adamopoulos IE, Gershwin ME. The implication of vitamin D and autoimmunity: a comprehensive review. Clin Rev Allergy Immunol. 2013;45(2):217-226. doi:10.1007/s12016-013-8361-3
[2] Siddiqee MH, Bhattacharjee B, Siddiqi UR, MeshbahurRahman M. High prevalence of vitamin D deficiency among the South Asian adults: a systematic review and meta-analysis. BMC Public Health. 2021;21(1):1823. Published 2021 Oct 9. doi:10.1186/s12889-021-11888-1
[3] Sizar O, Khare S, Goyal A, Givler A. Vitamin D Deficiency. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 17, 2023.
[4] Judd SE, Tangpricha V. Vitamin D deficiency and risk for cardiovascular disease. Am J Med Sci. 2009;338(1):40-44. doi:10.1097/MAJ.0b013e3181aaee91; Menon V, Kar SK, Suthar N, Nebhinani N. Vitamin D and Depression: A Critical Appraisal of the Evidence and Future Directions. Indian J Psychol Med. 2020;42(1):11-21. Published 2020 Jan 6. doi:10.4103/IJPSYM.IJPSYM_160_19; Ucan B, Sahin M, Sayki Arslan M, et al. Vitamin D Treatment in Patients with Hashimoto’s Thyroiditis may Decrease the Development of Hypothyroidism. Int J Vitam Nutr Res. 2016;86(1-2):9-17. doi:10.1024/0300-9831/a000269
[5] Brown SJ. The role of vitamin D in multiple sclerosis. Ann Pharmacother. 2006;40(6):1158-1161. doi:10.1345/aph.1G513; Latic N, Erben RG. Vitamin D and Cardiovascular Disease, with Emphasis on Hypertension, Atherosclerosis, and Heart Failure. Int J Mol Sci. 2020;21(18):6483. Published 2020 Sep 4. doi:10.3390/ijms21186483
[6] Anglin RE, Samaan Z, Walter SD, McDonald SD. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. Br J Psychiatry. 2013;202:100-107. doi:10.1192/bjp.bp.111.106666
[7] Menon V, Kar SK, Suthar N, Nebhinani N. Vitamin D and Depression: A Critical Appraisal of the Evidence and Future Directions. Indian J Psychol Med. 2020;42(1):11-21. Published 2020 Jan 6. doi:10.4103/IJPSYM.IJPSYM_160_19
[8] Gruber-Bzura BM. Vitamin D and Influenza-Prevention or Therapy?. Int J Mol Sci. 2018;19(8):2419. Published 2018 Aug 16. doi:10.3390/ijms19082419
[9] Zeng J, Li T, Sun B, et al. Change of vitamin D status and all-cause mortality among Chinese older adults: a population-based cohort study. BMC Geriatr. 2022;22(1):245. Published 2022 Mar 24. doi:10.1186/s12877-022-02956-1
[10]Papadimitriou DT. The Big Vitamin D Mistake. J Prev Med Public Health. 2017;50(4):278-281. doi:10.3961/jpmph.16.111
[11] Fisher SA, Rahimzadeh M, Brierley C, et al. The role of vitamin D in increasing circulating T regulatory cell numbers and modulating T regulatory cell phenotypes in patients with inflammatory disease or in healthy volunteers: A systematic review. PLoS One. 2019;14(9):e0222313. Published 2019 Sep 24. doi:10.1371/journal.pone.0222313; Rolf L, Muris AH, Mathias A, et al. Exploring the effect of vitamin D3 supplementation on the anti-EBV antibody response in relapsing-remitting multiple sclerosis. Mult Scler. 2018;24(10):1280-1287. doi:10.1177/1352458517722646; Janegova A, Janega P, Rychly B, Kuracinova K, Babal P. The role of Epstein-Barr virus infection in the development of autoimmune thyroid diseases. Endokrynol Pol. 2015;66(2):132-136. doi:10.5603/EP.2015.0020
[12] Arnson Y, Amital H, Shoenfeld Y. Vitamin D and autoimmunity: new aetiological and therapeutic considerations. Ann Rheum Dis. 2007;66(9):1137-1142. doi:10.1136/ard.2007.069831
[13] Kivity S, Agmon-Levin N, Zisappl M, et al. Vitamin D and autoimmune thyroid diseases. Cell Mol Immunol. 2011;8(3):243-247. doi:10.1038/cmi.2010.73
[14] Mackawy AM, Al-Ayed BM, Al-Rashidi BM. Vitamin d deficiency and its association with thyroid disease. Int J Health Sci (Qassim). 2013;7(3):267-275. doi:10.12816/0006054
[15] Simsek Y, Cakır I, Yetmis M, Dizdar OS, Baspinar O, Gokay F. Effects of Vitamin D treatment on thyroid autoimmunity. J Res Med Sci. 2016;21:85. Published 2016 Oct 18. doi:10.4103/1735-1995.192501
[16] Krysiak R, Szkróbka W, Okopień B. The Effect of Vitamin D on Thyroid Autoimmunity in Levothyroxine-Treated Women with Hashimoto’s Thyroiditis and Normal Vitamin D Status. Exp Clin Endocrinol Diabetes. 2017;125(4):229-233. doi:10.1055/s-0042-123038
[17] Ucan B, Sahin M, Sayki Arslan M, et al. Vitamin D Treatment in Patients with Hashimoto’s Thyroiditis may Decrease the Development of Hypothyroidism. Int J Vitam Nutr Res. 2016;86(1-2):9-17. doi:10.1024/0300-9831/a000269
[18] Xu J, Zhu XY, Sun H, et al. Low vitamin D levels are associated with cognitive impairment in patients with Hashimoto thyroiditis. BMC Endocr Disord. 2018;18(1):87. Published 2018 Nov 26. doi:10.1186/s12902-018-0314-7
[19] Łagowska K. The Relationship between Vitamin D Status and the Menstrual Cycle in Young Women: A Preliminary Study. Nutrients. 2018;10(11):1729. Published 2018 Nov 11. doi:10.3390/nu10111729
[20] Bläuer M, Rovio PH, Ylikomi T, Heinonen PK. Vitamin D inhibits myometrial and leiomyoma cell proliferation in vitro. Fertil Steril. 2009;91(5):1919-1925. doi:10.1016/j.fertnstert.2008.02.136; Halder SK, Goodwin JS, Al-Hendy A. 1,25-Dihydroxyvitamin D3 reduces TGF-beta3-induced fibrosis-related gene expression in human uterine leiomyoma cells. J Clin Endocrinol Metab. 2011;96(4):E754-E762. doi:10.1210/jc.2010-2131
[21] Pfotenhauer K, Shubrook J. Vitamin D Deficiency, Its Role in Health and Disease, and Current Supplementation Recommendations. J Am Osteopath Assoc. 2017;117(5), 301-305.
[22] Serrano MA, Cañada J, Moreno JC, Gurrea G. Solar ultraviolet doses and vitamin D in a northern mid-latitude. Sci Total Environ. 2017;574:744-750. doi:10.1016/j.scitotenv.2016.09.102
[23] Min M, Patel B, Han S, et al. Exocrine Pancreatic Insufficiency and Malnutrition in Chronic Pancreatitis: Identification, Treatment, and Consequences. Pancreas. 2018;47(8):1015-1018. doi:10.1097/MPA.0000000000001137
[24] Garland CF, Kim JJ, Mohr SB, et al. Meta-analysis of all-cause mortality according to serum 25-hydroxyvitamin D. Am J Public Health. 2014;104(8):e43-e50. doi:10.2105/AJPH.2014.302034; Gröber U, Reichrath J, Holick MF. Live longer with vitamin D?. Nutrients. 2015;7(3):1871-1880. Published 2015 Mar 12. doi:10.3390/nu7031871
[25] Papadimitriou DT. The Big Vitamin D Mistake. J Prev Med Public Health. 2017;50(4):278-281. doi:10.3961/jpmph.16.111
[26] Webb AR, Kazantzidis A, Kift RC, Farrar MD, Wilkinson J, Rhodes LE. Colour Counts: Sunlight and Skin Type as Drivers of Vitamin D Deficiency at UK Latitudes. Nutrients. 2018;10(4):457. Published 2018 Apr 7. doi:10.3390/nu10040457
[27] Mon J, Juzeniene A. Why skin colours differ. University of Oslo. 2011. Accessed November 22, 2023. https://www.mn.uio.no/fysikk/english/research/news-and-events/news/2011/why-skin-colours-differ.html.
[28] Mulligan GB, Licata A. Taking vitamin D with the largest meal improves absorption and results in higher serum levels of 25-hydroxyvitamin D. J Bone Miner Res. 2010;25(4):928-930. doi:10.1002/jbmr.67
[29] Eden RE, Daley SF, Coviello JM. Vitamin K Deficiency. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 8, 2023.
[30] Phan TX, Jaruga B, Pingle SC, Bandyopadhyay BC, Ahern GP. Intrinsic Photosensitivity Enhances Motility of T Lymphocytes. Sci Rep. 2016;6:39479. Published 2016 Dec 20. doi:10.1038/srep39479
[31] Howland RH. An overview of seasonal affective disorder and its treatment options. Phys Sportsmed. 2009;37(4):104-15. doi: 10.3810/psm.2009.12.1748.
[32] Eyles DW, Smith S, Kinobe R, Hewison M, McGrath JJ. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat. 2005;29(1):21-30. doi:10.1016/j.jchemneu.2004.08.006
Note: Originally published in October 2016, this article has been revised and updated for accuracy and thoroughness.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Hi Izabella,
Can you recommend a lower dose Vitamin D supplement? Strange situation—-I was diagnosed over ten years ago with Hashimoto’s by my functional doctor. I began taking 5000iu of D3, twice per day along with NDT as well as Probiotics (both regular and SB) and Bosweila. Not long after I began this regimen, I began getting acne after being acne free for 15 years. The breakouts were almost constant and I had no idea what the cause was. My doctor put me on Aldactone to help control it. I tried different types of thyroid meds, and tried eliminating each of the many supplements I take (except Vitamin D). No improvement. I stopped eating dairy and gluten 3 years ago. Very little improvement if any. During the pandemic, I found myself out of Vitamin D and it took me a few weeks for some reason to remember to buy some. But during this time, I seemed to not break out. I found only one article online about Excess Vitamin D linked to acne but nothing else. Being my levels were 125, I decided to see how much longer I would have clear skin. Sure enough I stopped breaking out. I want to go back to taking D, as my levels have since fallen to 55 but I am worried about getting the acne again. I am 44. It has been so nice having clear skin again just like in my 20’s! Lol Anyway, I was wondering if there is a way I can take D but not 5000IU. Also have you ever seen this issue before?
Antoinette – thank you for reaching out and sharing. ❤️ You certainly can get Vitamin D in smaller dosages. However, considering you had this reaction I recommend talking to your practitioner and testing your levels before continuing to supplement and consistently monitor levels to ensure vitamin D levels are not too high.
I always enjoy your articles and even submitted some to my traditional primary care physician ( initially she recommended I familiarize myself with your work for a heads up on Hashimoto’s.
I do think that when recommending supplements you should urge people to look up reputable sights that explain in depth uses, benefits, dosages and warnings. Many cannot afford a doctor or natural health practitioner and so may put themselves at harm especially if there are other health conditions that they also have. Also, sometimes their traditional doctor may not have the knowledge needed to guide a patient.
Nina – thank you so much for sharing your feedback! ❤️ I believe that most nutrients should come from the diet. This is why I always list food sources in the book and on the blog, for most of the nutrients, vitamins, minerals. and probiotics that are depleted in Hashimoto’s. However, some may require or prefer supplements. I recommend getting tested for deficiencies to determine your need for a supplement as instructed in the book and blog. I also don’t recommend starting multiple supplements all at once. I recommend starting one at a time and then adding another a week or so later once it has been confirmed that the first supplement is not causing any harm. Here are some article links which might help:
WHICH SUPPLEMENTS ACTUALLY HELP HASHIMOTO’S
https://thyroidpharmacist.com/articles/which-supplements-actually-help-hashimotos/
USING ENZYMES TO OVERCOME HASHIMOTO’S
https://thyroidpharmacist.com/articles/using-enzymes-to-overcome-hashimotos/
THE FOUR BEST PROBIOTICS FOR HASHIMOTO’S
https://thyroidpharmacist.com/articles/the-four-best-probiotics-for-hashimotos/
What is considered a safe tanning bed? There are some located at my gym and I have felt better in the past when tanning but definitely want to be safe.
Pam – thank you for following. ❤️ UVB tanning beds are thought to be a safer option (of course, always use caution and best practices with any type of tanning bed or sun light exposure). UVB helps make vitamin D, and has a shorter wavelength than UVA, so it penetrates less deeply into the skin.
Hi Izabella,
Thanks for this article. Vitamin D supplements always crash me and make me incredibly tired, but weirdly give me insomnia if taken in the evening. I have tried paring it with vitamin K, magnesium and vitamin A in different combinations with no success. So whenever I am prescribed it I am unable to take it. I have hypothyroidism (negative for hashimotos) and am post menopause. I try to get some sun, but have pale skin that burns quickly. I have asked my GP, integrative Dr and an endocrinologist, but they can’t explain it and say this should not happen. Any ideas would be appreciated.
Thanks,
Karen
Karen – thank you so much for sharing. Have you had your vitamin d levels checked? I always recommend having your levels checked before supplementing. You may want to check the added ingredients in the vitamin d you were using as some people are sensitive to some additives. I do have some other options to help boost your levels if the are low listed above such as the blue light therapy. I hope this helps.
Kendal – thank you for reaching out. I recommend following the directions on the bottle and checking with your practitioner to determine the right dosage for you.
I was diagnosed with Hashimoto Thyroiditis 18 years ago. Many years ago I also was tested for Vitamin D and I was low. It took a 2 month bout of pneumonia in January 2020 for me to finally take Vitamin D seriously. I did not realize at the time how this would affect my thyroid. I could tell that something was different, but continued to take my thyroid medication. In August 2022 I had Acute Thyroiditis and in the process realized that I was taking too much thyroid medication. I lowered my dose for the first time in 18 years. This summer I am again having to lower my dose because I am again having symptoms of too much thyroid medication. I attribute this to taking my Vitamin D deficiency seriously and taking supplements. It is amazing what this has done for my thyroid. I now realize that the thyroid can be healed and am trying other things from you to heal it further. I am enjoying learning about my thyroid condition from your resources and book. Thank you!
Brenda – Thank you so much for sharing your journey with me! I’m so happy to hear you are listening to your body and taking charge of your health. I do hope you will keep me posted on your continued progress.❤️
Is this a continual supplementation? I got my D levels up to 62 with 6000iu (woo hoo). My question would be do we have to keep taking this amount to maintain?
Maddy – thank you for reaching out. Great job getting your vitamin D levels up. Generally, I recommend 5000IU when supplementing. I also recommend testing every 3-6 months to ensure you are getting adequate amounts, and then testing again in the winter season as well. There are other options for raising your vitamin d levels mentioned in the article as well that you may want to consider.
Thank you for sharing, Dr. Wentz! I always appreciate your well researched and written articles 🙂 I have Hashimoto’s and I have been taking a D3 and K2 sublingually for a couple years. Before that I was taking capsules daily (3-5,000 iu daily) and then injections weekly to help my levels. My levels fluctuated between 17-34, until I made the switch to sublingual. Then they jumped to 86 within 3 months and have maintained healthy levels between 60-70 since. I’m looking to switch brands as my previous is harder to order. As I’m shopping around, I’m curious about the K2 having soy exposure. I have a low level soy sensitivity so I do try to avoid. Do you know of any liquid or even capsule D3 with K2 where the K2 doesn’t have soy exposure?
Mellay, Thank you so much for your kind words and for sharing your experience! Sublingual vitamin D3 with K2 can be very effective, especially for those with absorption challenges. Regarding K2 and soy, many forms of MK-7 (a common form of K2) are derived from natto, a fermented soy product. However, there are soy-free versions of MK-7 available, typically labeled as non-soy or chickpea-derived. I recommend looking for a D3/K2 supplement that is clearly marked soy-free and ideally third-party tested. A few professional brands offer this option in both liquid and capsule form, just be sure to check the ingredient label or contact the manufacturer directly to confirm. As always, consult your practitioner to find the best fit for your needs!