In my work as the Thyroid Pharmacist, I have mostly focused on caring for adults. However, in many cases, Hashimoto’s can start developing much earlier in life. Unfortunately, the symptoms in children can present a bit differently than the symptoms seen in adults, and much like adults, many children go undiagnosed for far too long.
I personally suspect that my thyroid condition started around age 4, after my exposure to Chernobyl, which potentially led to panic attacks and depression as a teenager. However, I wasn’t diagnosed until my 20’s. (Puberty can also be a trigger for Hashimoto’s.) Furthermore, even those who become symptomatic or are diagnosed later in life, may have early markers of Hashimoto’s, such as elevated antibodies, 5 to 15 years before a diagnosis is made!
I often get questions from readers about how to address Hashimoto’s, autoimmunity and other conditions (including eczema and asthma), in children and teens.
At the root of all of these is inflammation, and I love that functional medicine can often help all of these conditions with a similar approach. While children are a lot more resilient and can often heal quicker, given the right support, the challenge is that functional medicine approaches often need to be modified and tailored specifically for children.
Dr. Sheila Kilbane, a wonderful integrative pediatrician, has worked with children and teens who have Hashimoto’s, to help them thrive. Furthermore, she is an expert in lowering the overall inflammatory load in children. This can help with so many different conditions, including Hashimoto’s, eczema, asthma, and even some behavioral issues.
I had the pleasure of working with Dr. Kilbane myself, to support my son. I am fortunate to have a lot of functional medicine training and a large network of brilliant practitioners, as well as the resources and time to be present for him… yet, we could not stop my sweet little son’s eczema and slow weight gain. His eczema and feeding regression started around age 1, after a bout of the Norovirus (stomach flu) he had at 11 months of age. 🙁
Despite my best efforts and the support of brilliant local practitioners, things did not improve for over a year, until I got a comprehensive plan after the first appointment with Dr. Sheila and her wonderful team. I still have notes from my second appointment 8 weeks later: my son’s eczema was finally gone, we were able to introduce 30 new foods, and he had gained 4 pounds (which is very impressive for a 2-year-old who had barely gained 2 pounds in the prior year).
Furthermore, he started sleeping in longer stretches (he had been waking up every 2 hours prior to that). If you are a parent yourself, you know that worrying about your child’s health can be a full-time job!
As I get a lot of questions about children’s health issues, including how to support children with Hashimoto’s, naturally, I asked Dr. Kilbane to write a guest blog post for me sharing her experience in improving children’s health (including healing thyroid conditions!) and the research she conducted to write her new book, Healthy Kids, Happy Moms (which I highly recommend).
In this article, Dr. Kilbane will share:
- A teen client’s journey with Hashimoto’s
- The domino effect of inflammation in the autoimmune process
- How to reduce inflammation with diet
- The foundational supplements she used to support her client
- The thyroid medication change that can have a huge impact
- How her clinical practice impacted her own healing experience
Here’s Dr. Kilbane!
Katherine’s Story
Thirteen-year-old Katherine was a sixth-grader at the local Catholic middle school, when her mother brought her to see me in 2016. Sitting beside her mother in her plaid uniform skirt, Katherine listened while her mom relayed her medical history and their strong family predisposition to thyroid disease (Katherine’s brother, father, and both paternal and maternal grandmothers).
Katherine had been diagnosed with Hashimoto’s by an endocrinologist a year earlier, and was placed on Synthroid (100 mcg daily). The lively, athletic girl also struggled with recurrent respiratory infections that required an albuterol inhaler for wheezing, as well as antibiotics. She needed an inhaled steroid intermittently to keep the wheezing at bay, and to her mother’s recollection, she had been on four rounds of oral steroids for wheezing throughout her lifetime.
Like many moms in my practice, Katherine’s had done a great deal of research on nutrition and integrative treatments after finding that the traditional approach to thyroid disease wasn’t giving her daughter the results they had hoped for. “Is it all genetics? Isn’t there something else we can do?”
This new autoimmune (AI) illness, along with a history of recurrent illnesses, indicated to me that Katherine had excess systemic inflammation. We often think of inflammation as a red, warm, swollen joint, but we can also have inflammation that is widespread throughout the body.
In Katherine’s case, I suspected that systemic inflammation was hindering her immune system’s ability to do its job. Minimizing inflammation is one of the first steps in stopping the cycle of recurrent childhood illnesses, as well as slowing or sometimes even reversing an AI condition.
I explained the relationship of inflammation and illness to them — Katherine’s unique genetic predisposition to thyroid disease was interacting with variables in her environment and causing illness. Five main things in the environment trigger inflammation and cause illness:
- Food
- Environmental allergies
- Environmental toxins
- Infectious diseases
- (Physical and emotional) stress
Together, I explained, we would work to uncover Katherine’s triggers of illness, and reduce or eliminate as many of them as possible.

Image Source: SHEILA KILBANE M. HEALTHY KIDS, HAPPY MOMS;7 STEPS TO HEAL AND PREVENT COMMON CHILDHOOD ILLNESSES. [S.l.]: HARPER HORIZON; 2021.
I went on to explain that they could think of inflammation like a glass of water. The glass is our body, and the water is the inflammation. We need inflammation to some extent. For example, if we cut a finger, we need the inflammatory process to stop the bleeding. If we sprain an ankle, we need white blood cells to go to that area and begin to repair the damaged tissues. Problems arise when inflammation goes unchecked and spills over the top of the glass.
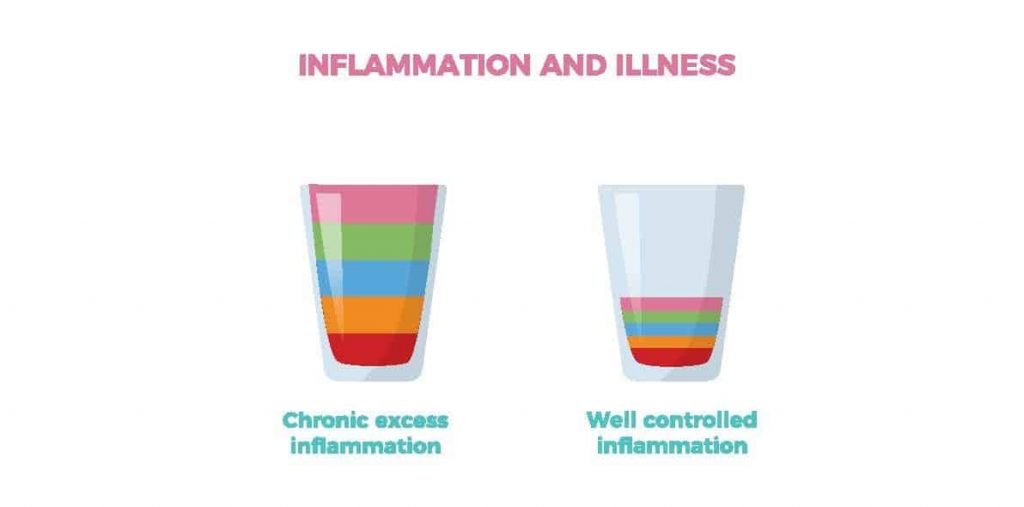
Image Source: SHEILA KILBANE M. HEALTHY KIDS, HAPPY MOMS;7 STEPS TO HEAL AND PREVENT COMMON CHILDHOOD ILLNESSES. [S.l.]: HARPER HORIZON; 2021.
The Domino Effect with Excess Inflammation
With AI conditions, the body mounts a response to something in the environment, such as a bacterial or viral infection, or an irritant such as a food sensitivity, an allergen, a toxin, or even stress. The inflammation that is meant to protect the body, instead, ends up attacking the body with antibodies to specific tissues (such as the thyroid, gut lining, or pancreas).
The goal is always to detect and treat the AI process as quickly as possible so that we can mitigate the ensuing damage. In Katherine’s case, the thyroid antibodies were attacking her thyroid gland.
Once an individual (child or adult) is diagnosed with one AI condition, it puts them at a higher likelihood of developing additional AI diseases (1). Autoimmune thyroid disease (AITD) and celiac disease are two good examples. When we work to keep systemic inflammation to a minimum, we can slow down this domino effect.
Celiac disease involves an AI process where the body (in particular, the lining of the GI tract) creates an immune response to the gluten molecule (a protein found in wheat, barley, rye, and many other processed foods). Gut inflammation ensues, leading to a host of symptoms in the GI tract, and elsewhere in the body. Dr. Wentz has an excellent article about gluten, celiac disease, and Hashimoto’s here.
When I first started practicing medicine in 2002, AI conditions in kids were rare. However, over the past 30 years, the global prevalence has increased significantly. Currently, 5 percent of the pediatric population has an AI illness, with AITD being the most common. (2) The prevalence of AITD among kids with celiac disease ranges anywhere from 2 percent, to as high as 40 percent. (3)
One 2001 Italian study showed that thyroid disease is three times higher in patients with celiac disease. (4) The good news, however, is that when these patients go off gluten, a significant number of them experience resolution of their thyroid disease. (5)
The concept that any AI condition might be reversed was, for all practical purposes, blasphemy to my conventionally trained medical mind when I first came out of residency. I had learned that AI diseases are lifelong and progress until there is so much tissue damage that the original tissue no longer functions.
A trip to India and a two-year integrative medicine fellowship changed the way I viewed the inevitable progression of AI diseases. I was at an Ayurvedic clinic in Mysore, where the practitioner told me their team could potentially help me get off my thyroid medication if I could stay and work with them for several months. Wait, what?! The idea of reversing an AI disease did not even compute in my mind.
The Ayurvedic doctor explained that through nutrition, detoxification, stress reduction, and Ayurvedic herbs, my body could come back into balance, and I could possibly go off the medication I had been taking since 1998. I could not remain in India for three months for their proposed cure, but it set the wheels in motion for the way I started to look at my own diagnosis of Hashimoto’s and that of my patients.
During my Integrative Medicine Fellowship at the University of Arizona, I learned the research behind the role of food in our health. With this additional training, I now approach AI diseases in a more comprehensive way.
Before we discuss the next steps in Katherine’s treatment, I have summarized thyroid terminology, for those who may not be familiar, below.
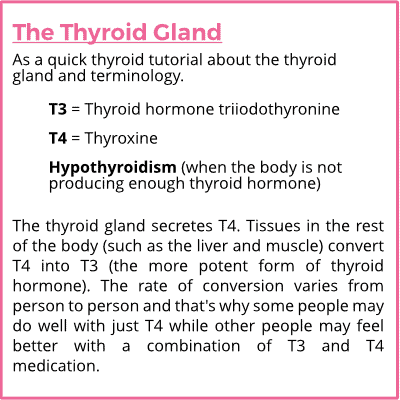
Image by: Dr. Sheila Kilbane
Lab Work and Endoscopy
I started working with Kathrine about a year after her initial diagnosis, and ran the following labs to get a more comprehensive overview of her health:
- Complete blood count with differential
- Thyroid hormone levels (TSH, Free T4, Free T3, Total T3, reverse T3)
- Note: During her initial work-up, I did a few other tests beyond these ones, but the above values are what I follow over time. The timing of the lab draw is important. Currently, we do twice daily dosing of Katherine’s thyroid medication, so she gets her blood drawn 6 hours after her morning dose.
- Thyroid peroxidase (TPO) and thyroglobulin (TG) antibodies
- Celiac panel, which tests three different antibodies:
- Gliadin IgA and IgG antibodies
- Tissue transglutaminase IgA and IgG antibodies
- IgA anti-endomysial antibodies
- Iron binding capacity and ferritin levels
- Vitamin D levels
- Vitamin B12 levels
- Red blood cell magnesium
- Viral titers, to check for evidence of current or past viral infections involving:
- Epstein-Barr virus (EBV), Cytomegalovirus (CMV), Herpes Simplex virus (HSV) 1 and 2, Human Herpesvirus 6 (HHV-6)
- Infectious diseases, as certain infections can sometimes be a trigger for AI conditions. (You can read more about infections common in those with Hashimoto’s, here.)
- MTHFR (Methylenetetrahydrofolate reductase enzyme) gene variation
- This genetic variation plays a role in the metabolism of folate (vitamin B9). (You can read more about this in Dr. Wentz’s MTHFR and Hashimoto’s article.)
- Stool study, to evaluate the gut’s microbiome
The first round of Katherine’s labs showed normal thyroid levels, but her thyroid peroxidase antibodies remained elevated, and she was positive for the three tested celiac antibodies. Furthermore, she had evidence of previous Epstein-Barr virus (EBV) and Human Herpesvirus 6 (HHV 6) infections, but the rest of the viral titers were negative. Her MTHFR test was negative for the two variants that were tested (C677T and A1298C), and her stool study, which looked at the microorganisms of her gut, did not detect any significant abnormalities.
My presumption was that Katherine likely had celiac disease first, and then the inflammation and immune dysregulation caused by gluten consumption, led to her thyroid condition (but that is not always the case for others). I thought that once we pulled her off gluten, her thyroid would normalize because, at the age of thirteen, she had not lived with the disease for very long. (6)
The ongoing progression of Hashimoto’s destroys the thyroid gland over time. Since we caught Hashimoto’s early on in her disease process, I was hopeful that we could stop or reverse the progression for her.
Our goal with the integrative approach to Hashimoto’s, is to utilize nutrition and supplements to reduce the excess inflammation and the antibodies that attack the gland, as well as preserve its function for as long as possible.
Of course, we also want the patient to feel great with good energy levels, a positive mental outlook, and an optimally functioning GI system. After all, we are the product of the nutrients that our GI tract can absorb. If we have gut inflammation, we will not absorb nutrients effectively and efficiently from our food. Eventually, we will become depleted of the natural resources necessary for our bodies to function properly.
The challenging part of this celiac diagnosis for Katherine was that she did not have any GI symptoms. Anytime a child has positive antibodies to celiac disease, I send them to a gastroenterologist so they can have a baseline endoscopy done (if needed) and a good follow-up. The GI doctor would have made the diagnosis based upon blood work alone since Katherine had three elevated celiac-related antibodies. However, Katherine really didn’t want to go off gluten and be singled out as the student who eats differently — just like every middle schooler I have ever met! So before changing her diet, the family confirmed the celiac diagnosis with an endoscopy.
Reducing Systemic Inflammation with Diet
Katherine’s biopsy was positive, so she and her mother removed gluten from their diets. I encourage families to do this together, but not everyone in Katherine’s household was able to do this. It is difficult to resist tasty, gluten-filled food when it’s in the house (I speak from personal experience!). It took several months for both mother and daughter to get into the groove with their new gluten-free lifestyle, but they did it.
Over the ensuing four to six months, as her inflammation decreased, Katherine’s recurrent illnesses — wheezing, and need for inhalers and antibiotics — resolved, as gluten was no longer triggering her inflammation and hindering her immune system from working as it should. As you can imagine, she and her mother were extremely happy about this.
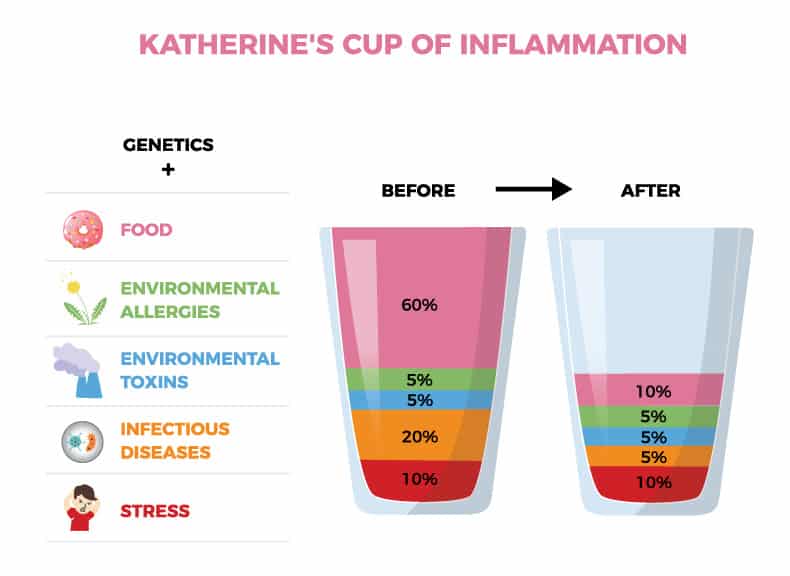
Image by: Dr. Sheila Kilbane
As the months marched on, we continued to follow her thyroid levels. I wish I could tell you that once we removed gluten, her antibodies went to zero, and that her thyroid levels normalized without the need for medications. However, although her antibodies decreased, she remained on thyroid medication six years later. (More on her thyroid medication regimen further on in this article.)
If Katherine had been living in a vacuum when she was originally diagnosed, her mother and I would have helped her remove dairy from her diet, besides gluten. Dairy is another food that triggers inflammation in all of us and can further contribute to immune dysfunction (read more about dairy and Hashimoto’s here).
Katherine’s mother and I frequently discuss the benefits of having Katherine remove dairy from her diet, but as a teenager who already has to avoid gluten, she has not been willing to remove dairy from her diet as well.
I feel it is important to let kids and teens be a part of the decision process with their own health, as much as possible. Katherine’s mother and I have respected her choice to continue eating dairy, and perhaps one day in the future she will decide to remove it. Katherine otherwise does an absolute rock star job of eating well at home (though being out and about with friends creates some challenges). In addition to small amounts of high-quality dairy, she fills her diet with fresh fruits, vegetables, and clean sources of fiber, proteins, and fats.
I also asked Katherine to cut back on her spinach intake because it is high in a compound called oxalates. Oxalates, found in foods such as raw spinach and rhubarb, are extremely acidic and are a major cause of kidney stones. They can also affect thyroid metabolism and contribute to symptoms such as joint and muscle pain. (You can learn more about oxalates and Hashimoto’s here.) Katherine was not experiencing such symptoms, but she was eating raw spinach daily in her smoothies, so I asked her to rotate the greens, as well as incorporate microgreens, lettuce, kale, and bok choy into her smoothies.
Supplemental Support
Over the years, I have recommended different dietary supplements for Katherine, based upon her lab results and how she feels. We initially started her off with what I call our foundational five supplements: probiotics, digestive enzymes, omega-3 fats, vitamin D in the wintertime, and a whole food supplement.
I have a specific way and order in which I start supplements with kids. Since so few people have access to an integrative pediatrician, I created a foundational supplement guide, which you can access here.
Katherine consistently takes magnesium to support the 300+ enzymes in the body that require it, and for two years, we had her on choline (in the form of phosphatidylcholine), which I affectionately call “the nectar of the gods.” It is found in egg yolks, red meat, liver, sunflower, and some legumes. It supports good cellular health by creating healthy cell walls (it’s like an oil change for our cell walls). Read more about choline in this article on brain fog.
Choline is also a major component of bile, and bile from the gallbladder is critical for the digestion and absorption of fats, which are required for proper hormone production, including thyroid hormones. (Learn about the connection between gallbladder health and Hashimoto’s here.)
Once Katherine entered high school and her academic stress increased, I also placed her on an adrenal support supplement. Adrenal glands provide the backbone for so many other systems in our bodies. They help us leap out of the way of a moving car when needed, as well as stay up late to study for a test. If we ignore them, our body will become depleted of the resources we need in order to make our adrenal hormones.
Furthermore, it is imperative to support adrenal function in order to optimize the function of the thyroid gland. You can read more about that in this article on adrenal health.
Thyroid Medication
I have been studying with an ENT surgeon, Alan McDaniel, MD, who travels the globe lecturing to other physicians on AITD. I learned about twice daily dosing from him (it more closely resembles the body’s natural thyroid hormone secretion than does a once-daily dose), and I use this method with Katherine’s thyroid medication regimen.
Two years ago, we changed Katherine’s thyroid medication to this twice-a-day regimen. We currently have her on Cytomel (T3) and Synthroid (T4) in divided doses, twice daily.
Since thyroid medication needs to be taken on an empty stomach, this can prove to be slightly challenging, but she and her mother make it work. They set an alarm for the late afternoon/evening dose. Changing your dosing to twice daily should only be done if this is something your doctor is familiar with. If you are well controlled with once-a-day dosing, I would suggest you stick with what is working for you.
In addition to prescription thyroid medication, I also have Katherine on a prescription medication called Low Dose Naltrexone (LDN), to help balance her immune system.
According to her most recent lab results, her TPO antibodies are still elevated, but less than half of what they had been when we first started working together. (They were at 288 IU/mL in September 2016, and 87 IU/mL in September 2020!)
As a teenager, Katherine often eats out with friends and continues to take the gluten communion wafer each week when she attends church services at school. I do think we would see a further reduction of her antibodies if she is eventually able to be 100 percent gluten free and remove dairy from her diet.
With that said, she is currently in a good place in terms of energy, mood, and sleep. Katherine feels great and is physically active. She plays basketball, snowboards in the winter, is a social butterfly, and works out in a heated room five to six days a week, with her mother and sister. Her GI system works beautifully.
Most importantly, Katherine understands how nutrition impacts her body and her immune system, and I am confident that as she moves into adulthood, she will take good care of herself.
My Experience with Hashimoto’s
The peak age of onset for Hashimoto’s in women is between 30 and 50 years of age, so I was close to the norm when I was personally diagnosed. When I was starting medical school in 1998, I started going home in-between classes to nap, for the first time in my life. Luckily, one of my medical school classmates — who was a nurse before coming to medical school — looked at my neck and said, “Sheila, you have a goiter, you need to go get that checked.”
I went to the Student Health Center and my thyroid antibodies (the ones that were attacking my thyroid gland) were off the charts. The doctor literally opened the textbook up while I was with her and said to me, “Of all the diseases to get, Hashimoto’s hypothyroidism is a good one because you only have to take a pill for the rest of your life, and you’ll be fine.” She painted a rosy picture of how lucky I was, that a single pill would fix this illness. She started me on Synthroid (T4): one tablet each morning (I can’t remember now how much I was taking back then).
I had no idea at the time that nutrition and stress could be playing a role in my thyroid disease. My diet as a busy medical student consisted of pizza, pasta, and fast food!
Fast forward a couple of years later, the Ohio State University Endocrinology Clinic on campus was so busy that they had to bring in one of their retired endocrinologists to help out. I told the one whom I spoke with that I was tired. Of course, I was in medical school after all, so it was difficult to ascertain whether the disease process was not fully controlled, my medication dose was off, or my lifestyle was to blame.
The retired endocrinologist shared with me that years ago, they used to treat thyroid patients using a combination of T3 and T4 medications. He also shared a study conducted out of Italy, in adult patients with hypothyroidism. It was a small study, but it showed that with the addition of T3, the participants saw a significant benefit to their mood and cognitive function. (7,8) Other studies suggested that about 15 percent of patients do not respond optimally to treatment with T4 alone. (9,10) So, besides the T4 (Synthroid) that I was taking, he added in T3, in the form of Cytomel.
I quickly felt an improvement in energy, and I have remained on a combination of T3 and T4 ever since. However, I was still having significant GI symptoms that persisted and continued to get worse. I will expound upon that in a moment.
When I entered residency in 2005, anytime I was interacting with my pediatric endocrinology-attending physicians, I suggested we consider adding in T3 to the children’s treatment plan if their labs looked normal but they were still not feeling optimal. One of the endocrinologists in particular was very receptive to that suggestion, and I shared the Italian study with him.
Whenever I worked with him over the course of my three-year residency, we added in Cytomel for a handful of patients who didn’t seem to have optimal energy levels on T4 medication alone. After finishing residency, I got two or three texts from him, sharing with me that he had added in T3 for his patients, and they experienced a benefit from that.
Today, we have so many more medication options than we did back then, including natural forms of thyroid medications that are a combination of T3 and T4, such as NP Thyroid, Nature-Throid, and Armour Thyroid. (Learn about thyroid medication options in this article.)
Switching one’s thyroid medication can bring great results, but was my new regime of T3 and T4 the final chapter in my story? Not at all.
My Experience Without Gluten and Dairy
I never thought to mention my GI symptoms to the med school endocrinologist because I didn’t think they could remotely have anything to do with my thyroid disease. I had constipation (it took me a significant length of time in order to have bowel movements, and they were painful). I also had hemorrhoids and often felt abdominal discomfort and bloating after eating.
Fast forward to 2010 as I was finishing up my integrative medical training, which included in-depth nutrition education as it relates to different health conditions. I started advising parents on how to deal with constipated children by removing dairy from their diets, but somehow, I still wasn’t connecting the dots in my own life. I had a bowel movement almost every day, so I didn’t think my bowels and the time and effort it took to go, were even a thing.
I was taking patients off gluten and dairy and seeing magic happen. Bowels were beginning to function properly, life-long stomach aches were going away, the allergy march (progression of the allergy-related diseases eczema, allergies and asthma) was improving. As a bonus, behavior, focus, and sleep were also improving. Parents were noticing fewer meltdowns, outbursts, and mood swings in their children.
This aligned with emerging research by Dr. Alessio Fasano, the head of pediatric gastroenterology and nutrition at Harvard. Dr. Fasano’s research found that gluten can create inflammation in the gut, which leads to systemic inflammation, even in individuals who do not have celiac disease.
Around this same time, my sister (who also has hypothyroidism) took gluten out of her diet, and felt a whole lot better. I took the plunge as well. The change was remarkable, like night and day, as if someone took a bag off my head. Suddenly (within days), I had a clear head, no energy slumps after eating, and my bowel movements were so much easier. Though they still took a little while, having easier bowel movements was a miracle to me!
In addition, my stomach stopped hurting after every meal, and my skin took on a fresh glow. I had been through all of this schooling and training — four years of traditional medical school, three years of pediatric residency, two years of integrative medical fellowship, in addition to five or six years of clinical practice — and I was just now figuring out I had a food sensitivity for much of my life?
I don’t remember having bowel issues or recurrent abdominal pain in childhood. When I lived at home, I was eating a much healthier diet and always playing sports.
This wasn’t the case when I went to university. My constipation started at that time with the sudden and rapid increase in my intake of pizza and beer (gluten and dairy), in conjunction with a lack of exercise and increased stress (even though I loved college).
As you can see in the photo below, I had significant systemic inflammation throughout my body. Besides the 15+ pounds I had gained, the other signs of inflammation were all the GI symptoms I discussed above (constipation, bloating, and abdominal discomfort after meals). If you recall the analogy I made earlier about excess systemic inflammation in our bodies being like a cup overflowing with water, you can see that mine was full for sure.
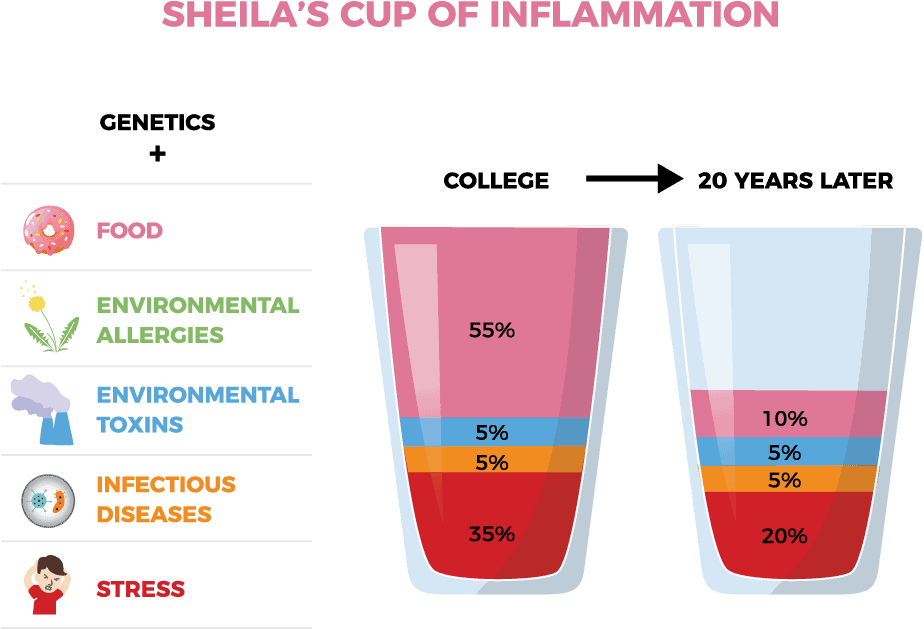
Image by: Dr. Sheila Kilbane
The longer I remained off gluten, the better and better I felt. I started to enjoy food again, and I could eat more because I wasn’t so bloated. It made me realize that I had previously become one of those people who eat because they have to eat, not because I enjoy the food.
About a year after I went off gluten, I attended a medical conference where one of the speakers explained the role of nutrition and how it impacts the gut — pun intended. In particular, she was extolling the virtues of a gluten-free, dairy-free diet for some people.
When she said that bowel movements should only take the time you take to urinate, I perked up in my auditorium chair. Hold on… what?!
The concept that moving your bowels should be quick, easy and without strain, did not compute with me. But this doctor had said it, and it made sense when I thought back to what I know about the physiology of our GI system. As I listened to this lecture on bowel movements and thought about the notion that they should be quick and easy, I took pause and thought, once again, about the connection between my bowels and my diet.
Should I also be off dairy? I had adjusted to losing one delicious food group by removing gluten. Was I prepared to lose another?
Dairy was a different story than gluten for me. Cheese was one of my favorite foods, and as a busy pediatrician, cheese was easy. There was no cooking or preparing — I could just grab a slice on the go and feel satiated for another couple of hours.
Nonetheless, I gave up dairy. Although my bowel movements had gotten tremendously easier since I had gone off gluten, when I went off dairy — while remaining off gluten — I could get in and out of the bathroom with the speed and efficiency of a NASCAR pit crew.
I really didn’t know that bowel movements could be so easy. And then I was in for another surprise six months after I went off dairy. I did a brief cleanse with a like-minded group. For three weeks, we took gluten, dairy, sugar, all animal products, caffeine, and alcohol out of our diets.
From a bowel movement perspective, doing this “cleanse” was like heaven, and I felt fantastic. While I couldn’t keep up that level of elimination for much longer than three weeks, it served an essential purpose: it showed me how my body could function, and helped me establish a different baseline of eating. It also gave me great insight into how I could further help my patients and help their parents understand what was going on with their children.
What I have learned from my practice and experience with my health, is that bowel rhythms give us a window into inflammation levels and gut health. From an integrative medicine perspective, the gut is the body’s powerhouse — the system that can set the tone for the body’s other systems.
When it comes to autoimmune diseases, keeping systemic inflammation to a minimum while optimizing cellular health can allow the immune system to function more effectively and efficiently.
By the time I learned all of this, my thyroid gland had too much damage to recover. I have not been able to reverse my disease after so many years, but wow, did nutrition play a significant role for me.
Just like Katherine, I manage my Hashimoto’s with twice-a-day dosing of T3 and T4, but I take NP Thyroid. I feel stronger and healthier than I did 20 years ago. And I think we can all agree that I look better than I did 20 years ago!
The Complexity of Testing For Food Reactions
In conventional pediatrics, if a child has constipation or AITD, we may test them for celiac disease (IgA antibodies) and for allergies to dairy and wheat (IgE antibodies). If those are negative, we advise the child to continue eating those foods.
This is where the need for understanding food sensitivities is essential. The children with negative tests for allergies and celiac disease may still have sensitivities to these foods, and if so, consuming these foods will cause excessive systemic inflammation. This was my case with gluten and dairy — I was not allergic to either, and did not have celiac disease, but eating them was throwing everything out of whack.
Food sensitivities are best assessed by doing a selective elimination diet. Blood tests which look for food sensitivities (IgG antibodies) have become more and more popular, but from conventional medicine’s standpoint, they are controversial. I use them in certain situations in my practice, but as of the writing of this blog, I most often use a selective elimination diet to determine food sensitivities.
The complexity of testing for food reactions led me to write an entire chapter on the topic, in my new book. If I had not figured out the connection between gluten, dairy, and my health, and if I had continued to eat them, I most certainly would have gone on to be diagnosed with other autoimmune conditions such as fibromyalgia or chronic fatigue syndrome.
There is so much misunderstanding about this for both patients and physicians, and I’d like to change that. You can download the Five Ways Food Triggers Inflammation in the Body reference table that I created to help illustrate the different ways that we can test for food reactions. The table also includes a list of symptoms associated with celiac disease.
Similar Approach Despite Different Test Results
Katherine and I both removed gluten from our diets after being diagnosed with Hashimoto’s. However, we have differences in our symptoms and our testing. Katherine tested positive for celiac disease, but I did not.
Ironically, I physically felt a big difference off of gluten, but Katherine did not. (Her recurrent illnesses and need for inhalers and recurrent rounds of antibiotics had resolved when she removed gluten.)
For Katherine, other, more persistent and widespread physical symptoms of celiac disease, may have taken years to manifest. This is also likely part of the reason why 97 percent of people who have celiac disease are currently undiagnosed. For those with undiagnosed celiac disease, the risk of lymphoma (cancer of the lymph system) increases. This is just one among a litany of reasons why it is important to understand how food affects us.
Here’s an overview of the differences between our diagnoses:
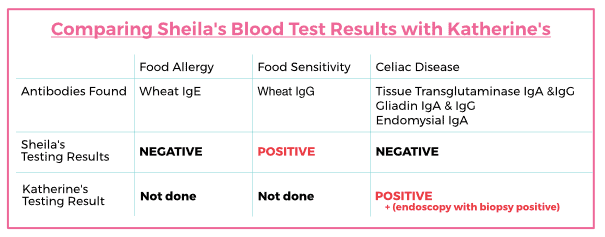
Image by: Dr. Sheila Kilbane
As you can see, there are many subtle and important variables with any AI disease. I encourage you to continue to do your own research when needed, and to find an integrative or functional medicine doctor to help you navigate your condition so that you can get the right treatment as quickly as possible!
Takeaways
If your child has been diagnosed with Hashimoto’s thyroiditis, there are several steps you can take to slow down (or halt) the domino effect. First, it is important to follow your doctor’s advice and start medication right away. Ask to have your child tested for celiac disease, as Hashimoto’s and celiac disease are common co-occurring conditions.
Seek out an integrative or functional medicine doctor to help you do more in-depth lab testing to look for vitamin and mineral deficiencies that may need to be addressed. Functional nutritionists may also be a great resource in terms of nutrition.
Consider removing gluten and dairy from your child’s diet after they have been tested for celiac disease. As a review, I encourage you to download the Five Ways Food Triggers Inflammation in the Body table I created.
You may also download my foundational supplement guide for general supplement recommendations, then work with your practitioner for more specific guidance.
In addition to implementing these dietary changes and supportive supplements into your routine, following all the regular “good habits of health” is a great place to start:
- Get plenty of sleep.
- Stay hydrated with fresh, filtered water.
- Be sure that the air you’re breathing at home is clean.
- Eat organic food whenever possible.
- Build your toolbox of ways to manage stress.
- Practice deep breathing each day.
- Stay physically active (try to break a sweat at least three times a week).
- Practice gratitude for the things that are going right in your life and along your health journey.
Be sure to check out my new book, Healthy Kids, Happy Moms, to discover a step-by-step PLAN you can use to transform your child’s health for good.
I hope these resources help your child on their journey!
References
- Ventura A, Neri E, Ughi C, Leopaldi A, Città A, Not T. Gluten-dependent diabetes-related and thyroid-related autoantibodies in patients with celiac disease. J Pediatr. 2000;137(2):263-265. doi:10.1067/mpd.2000.107160
- Minelli R, Gaiani F, Kayali S, et al. Thyroid and celiac disease in pediatric age: a literature review. Acta Biomed. 2018;89(9-S):11-16. Published 2018 Dec 17. doi:10.23750/abm.v89i9-S.7872
- Diamanti A, Ferretti F, Guglielmi R, et al. Thyroid autoimmunity in children with coeliac disease: a prospective survey. Arch Dis Child. 2011;96(11):1038-1041. doi:10.1136/archdischild-2011-300595
- Sategna-Guidetti C, Volta U, Ciacci C, et al. Prevalence of thyroid disorders in untreated adult celiac disease patients and effect of gluten withdrawal: an Italian multicenter study. Am J Gastroenterol. 2001;96(3):751-757. doi:10.1111/j.1572-0241.2001.03617.x
- Sategna-Guidetti C, Volta U, Ciacci C, et al. Prevalence of thyroid disorders in untreated adult celiac disease patients and effect of gluten withdrawal: an Italian multicenter study. Am J Gastroenterol. 2001;96(3):751-757. doi:10.1111/j.1572-0241.2001.03617.x
- Ventura A, Neri E, Ughi C, Leopaldi A, Città A, Not T. Gluten-dependent diabetes-related and thyroid-related autoantibodies in patients with celiac disease. J Pediatr. 2000;137(2):263-265. doi:10.1067/mpd.2000.107160
- Bunevicius R, Kazanavicius G, Zalinkevicius R, Prange AJ Jr. Effects of thyroxine as compared with thyroxine plus triiodothyronine in patients with hypothyroidism. N Engl J Med. 1999;340(6):424-429. doi:10.1056/NEJM199902113400603
- Toft AD. Thyroid hormone replacement–one hormone or two?. N Engl J Med. 1999;340(6):469-470. doi:10.1056/NEJM199902113400611
- Solter D, Solter M. Benefit of combined triiodothyronine (LT(3)) and thyroxine (LT(4)) treatment in athyreotic patients unresponsive to LT(4) alone. Exp Clin Endocrinol Diabetes. 2012;120(2):121-123. doi:10.1055/s-0031-1297253
- Panicker V, Saravanan P, Vaidya B, et al. Common variation in the DIO2 gene predicts baseline psychological well-being and response to combination thyroxine plus triiodothyronine therapy in hypothyroid patients. J Clin Endocrinol Metab. 2009;94(5):1623-1629. doi:10.1210/jc.2008-1301

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Great article and brilliant MD trying to help others. It saddens me however that not many doctors realise that diet plays such a huge role and what are the factors causing these illnesses. Also, it is frightening that it took many years of studying and practice for Dr Sheila to apply the method to herself and to be able to heal children. Thank goodness for the internet these days so the commoners such as us can search and obtain this information quickly. The triggers of inflammation mentioned are correct yet until doctors come to conclusion that current extensive childhood immunizations are the culpit of AI diseases and other chronic diseases we may have to continue to keep eliminating more types of food and live more restricted life.
Anna – thank you so much for sharing! ❤️ I’m so glad you found this article helpful!
I am 67 and was a sickly child. I wish all these things were known years ago. I was diagnosed with thyroid disease at age 49, but only found out on my own at age 57 that it was Hashimotos. About dairy, I tested myself and found that I was reacting to casein, but not lactose. I would become very stuffed up and have post nasal drip a lot. After realizing it was casein and gave up dairy, my chronic sinus infections stopped. I was wondering if the type of milk mattered. I do not drink regular A1 cow’s milk, but found I can tolerate and do not get stuffy with A2 or Goat’s milk. I feel better without A1 milk, but just wonder if the A2 and goat’s milk might still be an issue, although I seem to be symptom free while drinking those forms of dairy. Then again, at 67, if a bowl of A2 ice cream doesn’t stuff me up, I probably will continue to indulge. Thank you for so much helpful information!
Jane – thank you for sharing. Some people may not be able to tolerate even raw dairy. If you have been sensitized to casein in conventional cow’s milk, most will likely react to the casein in raw milk, goat milk, sheep milk and lactose-free milk. Casein is a protein within dairy that is highly problematic for people with Hashimoto’s. Here’s an article you may find helpful:
DAIRY AND HASHIMOTO’S
https://thyroidpharmacist.com/articles/going-dairy-free-to-reverse-hashimotos/