For over a decade, I had the symptoms of thyroid disease, but when tested for the “standard, usual biomarker for thyroid disease,” my TSH level, I was always deemed “normal”. I still have a copy of those lab results from 2008, before I was diagnosed with Hashimoto’s. Below the results is a handwritten note from my doctor at the time: “Your thyroid function is normal, no need to do anything.”
He also couldn’t — or wouldn’t — tie my diverse set of symptoms to problems with my thyroid. At the time, I already struggled with chronic fatigue, depression and anxiety, hair loss and terrible digestive issues, which left me popping Pepcid and other antacids like candy.
Perhaps that 2008 lab test showing a TSH of 4.5 μIU/mL would have been deemed normal for a 95-year-old woman, but I was only 25 at the time! And I felt miserable, sleeping 12 hours a day and yet still feeling completely fatigued.
Of course, I didn’t think to question the doctor or request more relevant testing — and most people don’t.
I was left out in the cold (pun intended: feeling cold all of the time was one of my many symptoms!) in regards to deciphering my condition, and found myself doing my own extensive research to find out what was happening to me.
I didn’t know then that the chronic stress in my life, my processed food diet, the Pepcid I routinely took… all of these triggers — and many more — should have pointed the way to a diagnosis for Hashimoto’s. Left unaddressed, they were also making my condition and symptoms worse.
I didn’t know then that by changing my diet, removing common food sensitivities, solving my gut issues and addressing other relatively straight-forward interventions — all that I could do myself without a prescription or significant expense — I would have felt so much better.
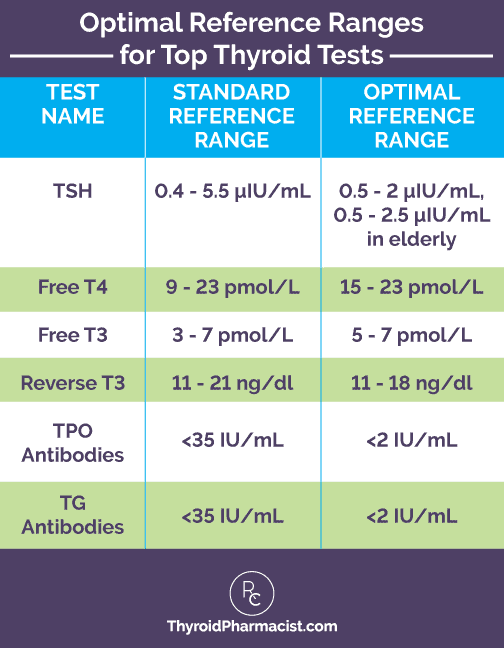
I also didn’t learn until later that my TSH of 4.5μIU/mL far exceeded what is viewed as an “optimal” reference range of 0.5-2μIU/mL. And only later would I learn about other markers such as thyroid antibodies testing that would have clearly shown that my thyroid was already actively being damaged.
Had I been adequately listened to, tested and diagnosed, I wouldn’t have had to suffer so greatly all of those years.
True, because of living for so many years undiagnosed, I likely was much more determined to dig into my root causes of the disease… which resulted in my protocols which have now helped thousands of people with Hashimoto’s. But it was a high price to pay in terms of my overall health, my relationships, and my quality of life for over a decade!
I do the work I do because I don’t ever want you or your loved ones to go through the same.
That is why I believe that an early and accurate diagnosis for Hashimoto’s is so important. I wrote this article for anyone who is not sure if he/she has Hashimoto’s. Please forward it to any friends/family members that may benefit.
This article will cover:
- How to get an accurate Hashimoto’s diagnosis
- The 5 stages of Hashimoto’s
- Testing for thyroid antibodies
- The importance of ultrasounds
- Monitoring and optimizing thyroid levels
4 Key Steps to an Earlier and Accurate Diagnosis
By the time many of my clients come to me, they tell a similar story to my own. Their doctor has told them that they do not have a thyroid issue, and that their TSH level is normal. Many of these doctors have been using now outdated TSH reference ranges. And most are certainly not using “optimal” ranges that functional practitioners advocate.
Even in cases where a client has done their own research, learned about the importance of other diagnostic markers such as antibody testing, and requested those tests, they have often been told that they simply don’t need them. I’ve even had clients who printed out journal articles relating to their symptoms and brought them to their doctors, to no avail. Some have even been put on medications for mental health issues relating to their (undiagnosed) thyroid symptoms such as depression and anxiety!
So how does one get diagnosed, earlier and more accurately? And after being diagnosed, how do you monitor how well your treatment and disease management is progressing?
There are a number of things that I recommend in order to get a thorough and accurate diagnosis of Hashimoto’s. When I initially start working with a new client, I walk them through several important steps that include a number of assessments and tests. In working with thousands of clients, I have found these steps most valuable in making an early and accurate diagnosis. These same steps also lay a foundation for you that can help you monitor your treatment plan and symptom improvements.
The great news is that you can start doing 4 of these preliminary steps yourself today!
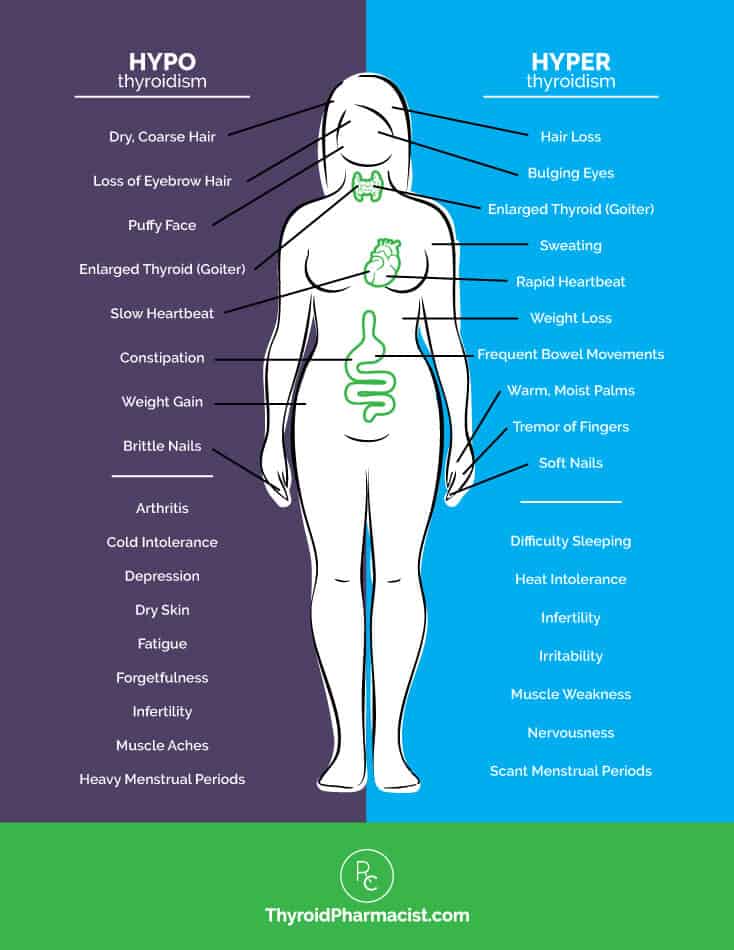
1. Start keeping track of your symptoms. I suggest regular journaling. Capture all of your symptoms, even if they are seemingly unrelated. Look at the graphic which overviews thyroid symptoms and evaluate yourself for each one — you may have missed some of these as you didn’t associate them with your thyroid health. Note in your journal as to when you feel better, or when you feel worse, and what you are doing at those times. (Example: Heartburn — feel worse after yelling at kids/feeling stressed out, also feel worse taking antacids; fatigued — feel worse when I drink at night; digestive issues — feeling better after getting off gluten!, etc.)
Take special note of how your symptoms feel when you eat certain foods. Major food sensitivities include gluten and dairy, but you might be surprised at what triggers your symptoms. I actually found I had issues with pineapples and peaches. When I ate them, I had terrible acid reflux.
2. Document your health timeline. This is such an important step and will help you identify potential triggers for your Hashimoto’s-related symptoms. Think back as far as you can and start documenting periods of illness in your life, infections you’ve had, periods of significant stress, medications you’ve been on (in particular, antibiotics, oral contraceptives, and antacids), toxin exposures you may have had, major dental work, etc.
Answer the question, “When was the last time you felt well, and what were you doing in the time period right before you started feeling unwell?” When I initially started documenting my own health timeline, I realized that the mononucleosis I had had in college (caused by the Epstein-Barr virus) was likely the trigger that set off my own Hashimoto’s progression.
The Epstein-Barr virus (EBV) has been implicated in triggering many autoimmune conditions such as Hashimoto’s. As an example, in a survey I did of 2,232 people with Hashimoto’s, 11 percent of them reported that they started feeling unwell after acquiring an Epstein-Barr infection!
Hopefully you can see how a thorough health timeline can help pinpoint your own root causes. And it can definitely help your doctor as well.
You’ll be surprised at how many triggers you may uncover when constructing you own health timeline.
3. Find a functional doctor or clinician if your existing doctor won’t listen to your concerns or focus on the symptoms you are experiencing. Here is a directory of functional practitioners. You can also check out my own list of recommended doctors.
Even if your current doctor says you have “normal” TSH levels and no thyroid issue, know that there is a reason you don’t feel well! There is a reason for the symptoms you have, even if they feel random and overwhelming. A good functional practitioner will take the time to listen to you, and will LOVE to see your journal of symptoms and health timeline. That’s who you want to partner with in getting an accurate diagnosis and implementing a good treatment plan. A good functional practitioner will also know the best biomarkers that should be tested.
4. Get the appropriate thyroid function tests, including thyroid antibodies testing. We now know that thyroid antibodies testing is the best “early warning” indicator for having Hashimoto’s!
More on the importance of thyroid antibodies testing as the best diagnostic tool in a moment. But just to reiterate, TSH screening isn’t enough — for a variety of reasons. You can learn more about TSH screening limitations, and can even find a letter on this page that you can take to your physician if he/she is not familiar with the current reference range information.
If you have a good functional practitioner, they will want to do a full thyroid panel, including tests for thyroid antibodies, Free T4 and Free T3. (Note that even if you don’t yet have a good functional practitioner, you can self-order these tests while looking for a new practitioner.) For an accurate diagnosis, some people may also benefit from having an ultrasound of their thyroid. I’ll talk more about this later on in this article.
These same 4 steps continue even after your diagnosis.
Once you are diagnosed and begin medication and/or other treatments, such as dietary interventions, you will need to monitor yourself with ongoing antibody testing and symptom assessments. You’ll also likely need additional lab testing to best understand the root causes of your disease, including tests focused on nutrient levels, as well as adrenal and gut health. You’ll need to continue to track what makes you feel better or worse in your journal.
So let’s talk more about the best testing to diagnosis Hashimoto’s.
And again, it isn’t TSH screening alone!
TSH Screening Only Catches the Later Stages of Hashimoto’s
If we were to perform blood tests in advanced, untreated cases of Hashimoto’s, we would find an elevated TSH and low levels of T3 and T4. Thyroid antibodies would also be found in most cases.
But just like with my own story, most people won’t test with an elevated TSH if they are in the earlier stages of Hashimoto’s disease progression, even though damage may already be being done to their thyroid!
In order to better understand why TSH screening is not the best screening test for early diagnosis, it’s important for you to know just a bit about the 5 stages of the development and worsening of Hashimoto’s.
The 5 Stages of Hashimoto’s Development
If we look at why someone develops Hashimoto’s in the first place, we know from the research that there are three things that are necessary:
- A genetic predisposition. You can read more about genetics and Hashimoto’s, but note that there isn’t a single gene responsible for the condition. While it does tend to run in families, there is a lot one can do to keep any inherited “bad” genes from turning “on”!
- Intestinal permeability, or leaky gut (often caused by diet and exposure to food sensitivities or toxins).
- One or more triggers like stress, infections, food sensitivities, toxin exposures, diet… and many others that you can read about in my book Hashimoto’s Protocol.
A person needs to have all 3 of these in order for Hashimoto’s to develop and progress.
So let’s assume we are talking about Person X and that eventually Person X will have all 3 requirements for Hashimoto’s. They have a mother and aunt with Hashimoto’s (and have lived a lifestyle that “turned on” the bad genes), they have intestinal permeability due to sensitivities to dairy, and they had an infection and chronic stress (like I did in college!) showing up in their health timeline, which are likely their initial triggers.
So let’s see what happens to Person X as they go through the 5 Stages of Hashimoto’s Development (And pay attention to when the TSH level screening is actually elevated as a concern! Hint: It isn’t until Stage 3):
Stage 1 of Hashimoto’s: The Genetic Predisposition
Initially, Person X won’t have any manifestations of Hashimoto’s. The disease simply runs in Person X’s family. If tested, they are going to have a normal TSH and will have normal thyroid function. They will not have any elevated thyroid antibodies. If you were to biopsy their thyroid gland, it would look perfectly normal. They just have the genes at this point.
Stage 2: The Breakdown of Immune Tolerance
Somewhere along the way, Person X has a trigger, or multiple triggers. They’ve encountered life events that have “turned on” one of the bad genes associated with the disease.
Perhaps they lived through a period of chronic stress, or had an infection, that triggered their disease progression. They may have ongoing food sensitivities to dairy that have also created an intestinal permeability issue. Now they have all 3 requirements for developing Hashimoto’s.
In this second stage, you start seeing the breakdown of the thyroid’s immune tolerance. This is when we will start seeing elevated thyroid antibodies in most people. More about this below, but note that this stage can go on for many years —a decade or more — before a person moves on to Stage 3 or 4, where we start to actually see symptoms and changes in thyroid function. (However, a person can have Hashimoto’s even if their thyroid antibody test is negative. I’ll discuss this more in a minute.)
TSH levels can show as completely normal, and that’s the problem with using it as a screening test to diagnose Hashimoto’s!
Stage 3: Subclinical Hypothyroidism
Stage 3 is when subclinical hypothyroidism occurs, and can occur many years after Stage 2. In this stage, Person X is going to finally screen for an elevated TSH in addition to having thyroid antibodies. They will have immune cell infiltration into the thyroid gland, although their T3 and T4 levels are still going to be normal.
Many people will experience some symptoms of hypothyroidism or autoimmune disease at this stage.
Stage 4: Overt Hypothyroidism
Stage 4 is when we will start seeing overt hypothyroidism. There has likely been a lot of damage that has now occurred to the thyroid gland. The thyroid will no longer be able to compensate nor keep the thyroid hormone levels normal, and we will start seeing a change in T3 and T4 levels.
Stage 5: Hashimoto’s and Other Immune Disorders Progress
In Stage 5, as Hashimoto’s progresses, we may have a progression to other immune disorders. At this time, Person X may get diagnosed with rheumatoid arthritis, lupus, or any of the other types of autoimmune conditions.
Note that our earliest “warning” about Person X having Hashimoto’s, and our best opportunity for early intervention, is during Stage 2 when we initially find evidence of thyroid antibodies.
If Person X doesn’t have their antibodies tested, how will they know the reason for their symptoms? If they don’t maintain a journal and a health timeline, they may not see the clues for their disease, or share the right information with their doctor. If they don’t have a doctor who asks the right questions, or is willing to do early screening for thyroid antibodies, they may be told they do not have a thyroid issue.
Thyroid Antibodies: My Immune System is Attacking My Thyroid!
We know thyroid antibodies can show up in Stage 2, earlier than an abnormal TSH level will appear, and can be a good “early warning” for Hashimoto’s. But many people may still not really understand what is happening in their bodies that results in the appearance of antibodies in the first place.
Thyroid antibodies appear because:
- 90 to 97 percent of people with thyroid disease have Hashimoto’s.
- Whenever you have an autoimmune condition, your body will produce antibodies that result in an attack to some part of the body.
- All autoimmune conditions, including Hashimoto’s, result in the body developing something called “a lack of self-tolerance”. The body is no longer able to recognize its own tissue as separate from the foreign “invader” (such as a bacterial infection). In the case of Hashimoto’s, the body’s immune system initially focuses on some invading cells, but due to something called molecular mimicry the body may then target other cells (in the thyroid gland) that resemble these invaders.
- Scientists think that within the body’s immune system, B cells in the thyroid gland and lymph nodes secrete thyroid antibodies, and that the antibodies somehow erroneously direct T-cells to damage the thyroid gland (instead of the foreign invader).
The good news is that in most cases of Hashimoto’s, early testing of thyroid antibodies can detect this breakdown of immune tolerance before thyroid function is affected.
By the time I was finally tested for Thyroid Peroxidase (TPO) antibodies, they were above the 2000 IU/mL range, and damage was already being done to my thyroid gland. (Note that the optimal range for TPO antibodies is less than 2 IU/mL).
You can read much more about thyroid antibodies here.
Along with being the most recommended thyroid screening test, thyroid antibodies testing is very helpful to monitor how thyroid medication or other treatments are helping with disease management. We’ll talk a bit more about monitoring Hashimoto’s at the end of this article. In my clinical practice, we routinely measure decreases in antibodies due to any number of interventions, some of the most dramatic being dietary changes. You can read more about the interventions that result in lowering thyroid antibodies here.
Antibody Testing is Easy
While I always prefer to have a good functional practitioner in the picture when people are looking to explain their symptoms (and that is why it is part of the “4 Key Steps” already discussed), you do always have the option of ordering your lab tests yourself through Ulta Lab Tests. They offer self-order options for several of my own discounted panels, which can be ordered anywhere in the US. You will receive a lab order that can be taken to your local lab, and the results will be sent to you electronically.
In many cases, you can then send the receipts for reimbursement to your insurance. (Please check with your insurance to ensure that they will accept this, as well as to understand the required submission procedures). For a Hashimoto’s diagnosis, “E06.3” is a billable/specific ICD-10-CM code that can be used for reimbursement purposes.
There are three thyroid antibodies tests, and two of these, Thyroid Peroxidase (TPO) and Thyroglobulin (TG) antibodies, are created by the immune system and associated more greatly with Hashimoto’s.
80 to 90 percent of people with Hashimoto’s will have either TPO or TG antibodies, or both.
The more elevated the thyroid antibodies are, the greater the likelihood of developing overt hypothyroidism, as well as possibly additional autoimmune conditions. Note that you can still have Hashimoto’s without showing antibodies. If you are experiencing symptoms and/or if Hashimoto’s runs in your family, but you are not testing positive for antibodies, you might want to get an ultrasound. I’ll discuss ultrasounds in a moment.
The third type of thyroid antibodies is TSH-Receptor (TSH-R) antibodies, including thyroid-stimulating immunoglobulin (TSI). This marker is elevated in more than 90 percent of people with Graves’ disease. Another TSH-R antibody is known as TSH-binding inhibiting immunoglobulin (TBII). This is elevated in over 50 percent of people with Graves’ disease. TSH-R antibodies are also more common in people who have thyroid cancer.
You can order all 3 antibody tests online:
- TSH Receptor antibodies (TSH-R)
You can also opt for a full thyroid panel which includes tests for TSH, free T3, free T4, and two of the thyroid antibodies (TPO and TG):
For additional information on the full thyroid panel, you can check out my article on thyroid testing.
Why You Need a Good Functional Doc or Clinician: Interpretation and Treatment Monitoring
Even if you initially self-test (and let’s say you see you have elevated antibodies and symptoms pointing to a diagnosis of Hashimoto’s), as you’ll know from the “4 Key Steps” section earlier in this article, I highly recommend finding a good functional doctor or clinician to work with!
One of the important reasons for this step is to have the right person to interpret your lab findings, symptoms and health timeline, as well as to assess “how you feel” as you try different interventions and treatments. This “medical partner” may also recommend medication, and if so, he or she will need to monitor you while you take it (via follow-up thyroid lab testing as well as listening to “how you feel” and what is happening to your symptoms). They may change medication dosage, or even the medication, based on this ongoing monitoring and support.
While testing provides important information and a measure, one of the other important things someone like me, a clinician, needs to always look at is whether my client is feeling better or worse based on what we are having them do.
A good functional practitioner will also know when to recommend getting an ultrasound done. This may be needed for diagnosis in cases where you don’t have detectable thyroid antibodies, but may still show symptoms and/or have a family history of thyroid conditions.
The Diagnostic Value of Thyroid Ultrasounds
Remember, 80 to 90 percent of people with Hashimoto’s will have either TPO or TG antibodies, or both.
But research also suggests that 10 to 50 percent of people with Hashimoto’s may not test positive for antibodies. In these cases, a person might have a less aggressive version of Hashimoto’s known as antibody negative or seronegative Hashimoto’s.
In these cases, a thyroid ultrasound can be used to find physical changes in the thyroid gland that point to Hashimoto’s.
In fact, 10 percent of people diagnosed with Hashimoto’s are diagnosed using an ultrasound.
I actually recommend that everyone with Hashimoto’s or thyroid disease has at least one ultrasound in their lifetime, especially women of childbearing age. If thyroid nodules are found, then I recommend having an annual ultrasound.
A thyroid ultrasound is a very simple, non-intrusive test that only takes about 10 minutes. It uses sound waves to image the thyroid. A lubricant jelly is placed on the skin and a small hand-held transducer is passed over the thyroid. The ultrasound will show any change in gland size and texture. Clinicians can find changes in thyroid size (shrunken or enlarged), tissue density and texture (rubbery), as well as nodules (abnormal growths), which are all characteristic changes found with Hashimoto’s. Growths can also be a signal for cancerous nodules. If there is a concern with that, the next step would be to have a nodule biopsy, and you can read more about that in my article on thyroid cancer.
Monitoring Treatment and Feeling Better!
Again, just think back to my “4 Key Steps” to see what needs to happen after you’ve been diagnosed with Hashimoto’s. You’ll want to continue to track your symptoms and add to your health timeline, as well as work with a good functional clinician to interpret your initial thyroid lab tests and implement a customized treatment plan created for you and your particular set of symptoms and triggers.
Then you’ll want to monitor how that treatment plan makes you feel. That’s more than just lab numbers, although those are important, too.
I typically recommend repeating TSH, Free T3 and Free T4 labs when evaluating whether a particular dosage adjustment needs to be made or whether a change to a completely different medication may be warranted. I also recommend retesting every 4-6 weeks until the dose that works best is established. Once we have the right dose and no new symptoms pop up (like anxiety or other issues associated with too much medication), then I recommend testing every 6 months.
I like to look at “optimal” ranges, as I know that many people feel their “best” when they are more aligned with optimal than standard reference ranges. I know I feel best when my TSH is between 0.5μIU/mL and 2μIU/mL.
Here are the standard and optimal ranges:
You can find more information on these optimal ranges here.
I’ll also test TPO antibodies every one to three months to determine the progress from various interventions, such as dietary changes, stress management programs, or nutrient supplementation. Thyroid antibodies are not only “early warning” indicators of Hashimoto’s, but are also a great marker to monitor disease progression and remission. If you are seeing a reduction in antibodies, especially when accompanied by a reduction in symptoms, it is a good indication that your condition is improving and that you are on the right path with your specific interventions.
I also suggest a number of other assessments once an initial diagnosis of Hashimoto’s is confirmed.
Additional evaluations and testing are discussed in my book Hashimoto’s Protocol, including: food intolerance testing, gut function testing, adrenal testing, nutrient deficiencies testing, genetics testing (specifically the MTHFR gene variation to look at nutrient extraction), and more.
Get Started Today with the 4 Key Steps
You can get started on your diagnosis today, just begin with the initial “4 Key Steps.”
Start with the easiest step, which is to reflect on your symptoms and why you don’t feel well. Write things down in your journal. You may find it is easier to do that than to trying to talk to your very busy doctor about “all the little things that seem to be off with you” during a routine checkup! Most people with Hashimoto’s will have a lot of symptoms, seemingly all unrelated. Don’t let that overwhelm you.
Then, start focusing on your own health timeline. In doing so, you may uncover triggers for Hashimoto’s that you had completely forgotten about, such as an earlier infection or toxin exposure.
Once you have a good functional practitioner working with you, and the right tests, you’ll find that some fairly straight-forward interventions will make you start feeling better. Many dietary changes, as just one example, not only make the majority of people with Hashimoto’s feel better, but have been shown to reduce thyroid antibodies as well.
I wish you all the best on your healing journey!
P.S. Sign up for my weekly newsletter to keep posted on easy-to-understand information that may help you feel better more quickly! In doing so, you’ll receive a free Thyroid Diet Guide, 10 Thyroid friendly recipes, and the Nutrient Depletions and Digestion chapter of my Root Cause book. You can also follow my Facebook page to keep up with updates about new research, resources, giveaways, and helpful information.

 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
I live in Australia. I am 80 years old, almost 81.
All the information is very interesting and believable. I am glad about the recommendation about checking my gut function for which I already have the kit…
The problem I have on top of having Hashimoto’s is that since June 2015 when I had an Addison’s crisis, I have not been able to find a doctor who wants to help me.
My 8th doctors, the one I see at present, does not like me taking T3 (40 mcg/day) (I was feeling rather well, but the TSH!!!! was out of whack) and insisted on giving me T4 (50 mcg/day) together which I did as I do not have more doctors to see nearby to try. I felt really bad. After a month, I stopped the T4. I was supposed to have a due colonoscopy (I grow polyps), and my endocrinologist wrote a letter to the gastroenterologist, asking him not to colonoscopy me so to speak because I could have a heart attack or a stroke. My pulsations are 70ppm or a bit below (before taking T3 the pulsations were below 60). I feel very cold still and I have constipation (from birth by the way), but I feel less tired. All and all with 40 mcg/day I feel better. My body temperature goes 36.6C to 37. (It used to be, 3 years ago below 36C) But my endocrinologist like all the others, does not want to hear about T3 (I buy it from US). Now, I have a hernia also and I cannot have surgery because my endocrinologist will write a letter to the surgeon telling him not to have surgery because I can have a heart attack or a stroke. I am desperate
Monsie – thank you for reaching out and sharing your journey with me. I understand how hard all this is. I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic diseases, rather than disease symptoms. I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time.
If you cannot find a Functional Medicine practitioner in your area, it is possible to work with an overseas practitioner remotely via Skype or some other online video platform. Here’s a link which might help:
http://www.thyroidpharmacistconsulting.com/europe1.html
I live in Spain. After reading your book and following the diet I took blod test again and find that my TSH has come from 4.1 to 7.8.
To be honest I stoped taking the Levotyroxin two weeks before (It was warm and I was travelling so could not take it with me) But such a rise on the levels of TSH is not logical. I will take again Levotyroxin but I´m not sure if to follow the diet is really helping me at all.
M.Pilar – thank you for reaching out and sharing your journey. <3 I know how overwhelming everything can be. Gut healing is a journey; you may need various interventions like removing reactive foods and infections, taking enzymes and probiotics, and balancing nutrients. Remember, be kind to yourself and learn to listen to your body so that you can support and feed it properly! You are worth it! You may find this article helpful as well!
WHAT'S CAUSING YOUR LEAKY GUT
https://thyroidpharmacist.com/articles/whats-causing-your-leaky-gut/
SIBO
https://thyroidpharmacist.com/articles/sibo-prevent-remission-hashimotos/
6 DIFFERENT ROOT CAUSES
https://thyroidpharmacist.com/articles/6-different-hashimotos-root-causes/
Hi, I didn’t notice a mention of fluoride in the water. Those who have spent decades drinking fluoride will indeed develop thyroid issues. Also, no mention of EMFs from mobile phones, cell phones, microwave ovens, smart meters, etc. And then there’s glyphosate in the veggies if they’re not organic, esp. the greens, and we need the leafy green phytonutrients most of all. Note that for those who are taking levothyroxine, there may be aluminum lake in the coloring — except for the white tablet.
Clare – thank you so much for sharing this information with me! I am collecting suggestions of different research projects and I will add these to my list. <3 Here is an article you might find interesting:
FLUORIDE AND YOUR THYROID
https://thyroidpharmacist.com/articles/fluoride-and-your-thyroid/
I am still confused about the connection between Hashimotos and Thyroiditis. My surgical oncologist (began my journey with breast cancer almost 18 years ago) said that “simply”…I have thyroiditis and that my body was attacking my thyroid gland. As well, he said that having only a TSH test was next to useless. Since then I have insisted that my family doctor test for more. Last year my ANTI-TPO was 391 with others in a normal range. I have been taking synthroid 0.175mg for many years. Need some clarification between those two.
Thank- you Dr Izabella
Ruth – thank you for reaching out and sharing your journey! I am so sorry you have had to go through all this. I do understand how overwhelming it can be. <3 Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target. We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are the links to my books:
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Hi,
I am a 73 year old woman, who was diagnosed about 2 years ago with hypothyroidism, and put on medication. While I do feel better, I still do not feel “right.” My mother had a goiter, and my daughter was diagnosed shortly before I was with hypothyroidism also. My doctor kept telling me that my numbers were right in the middle, and where they should be. Unfortunately, no one told my body that. About three years previously, when I broke a hip, routine blood work showed that I was deficient in B12, for which I began taking shots. When I moved to a new location, my new doctor found the thyroid problem. This doctor moved, and my new doctor doesn’t seem in a hurry to go further with different tests, and I am not sure how to address this issue. I have other issues which began at about the same time. I have cataplexy, narcolepsy, terrible stomach issues of long standing, as well as other health problems. Before I was put on meds for my thyroid, and B12, my memory had slipped to the point where I was online constantly taking Alzheimer’s tests because I thought I was losing it. I couldn’t even sew on a button or use my hands. Thank goodness, that is better, but …………… (Also been told I have Reynards). I would like to know where to go from here. How can I approach this new physician? I an tired of just being tired.
Maryann – thank you for reaching out and sharing your journey. <3 I am so sorry you are struggling with this. Hashimoto’s often is a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better.
Hashimoto's is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission.
You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto's. Once you do, you will know what types of changes you need to implement to make yourself feel better.
BUILDING YOUR OWN HEALTH TIMELINE
https://thyroidpharmacist.com/sample-health-timeline/
I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://www.thyroidpharmacistconsulting.com/pages/clinician-database
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
http://www.thyroidpharmacistconsulting.com/recommended-compounding-pharmacies.html
I had hyperthyroid about 10 years ago. I was healed after going on a detox and restricted gluten and dairy.
However these days I feel tired even after sleeping, feel like I have a sore throat, seem to have phlegm all the time, and feel difficulty swallowing.
Couple of years ago I had a greatly elevated TPO but didnt do anything as I was feeling fine.
I am worried 🙁 i am not in the US. Alternative practitioners are expensive too. 🙁 any advice for me? 🙁
Lis – thank you so much for reaching out and sharing. <3 I'm so sorry to hear you are struggling with all of this. Fatigue was the most debilitating symptom I experienced with Hashimoto’s. It actually started 8 years before I was finally diagnosed in 2009 after I got Mono (Epstein-Barr Virus) in college. I needed to sleep for 12 hours each night to be able to function, and by “function” I mean after hitting the snooze button on my alarm clock for two hours (ask my poor husband), I would drag myself out of bed and then had to drink 46 cups of caffeine everyday to keep myself awake. I often had Red Bull and Pepsi for breakfast, and was the epitome of “wired but tired”. I hope my articles help you get started 🙂
OVERCOMING THYROID FATIGUE
https://thyroidpharmacist.com/articles/strategies-overcome-hashimotos-fatigue/
THIAMINE AND THYROID FATIGUE
https://thyroidpharmacist.com/articles/thiamine-and-thyroid-fatigue
I am 33, I have TSH : 6.09, T3 : 3.10, T4 : 1.07 and TP AB : 1.0 what do you recommend at this point. We are trying to have our third baby since 8 months but no success.
Fahim – thank you for reaching out. <3 Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormon Here are some articles you might find helpful:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://thyroidpharmacist.com/articles/top-6-thyroid-tests/
HASHIMOTO’S AND PREGNANCY
https://thyroidpharmacist.com/articles/hashimotos-and-pregnancy
BEST ADVICE FROM HASHIMAMAS
https://thyroidpharmacist.com/articles/best-advice-hashimamas/